CHAPTER 15 Foot and nail care
1. Correlate medical conditions with potential foot problems.
2. Describe the structure and function of the foot and nails.
3. Compare and contrast foot malformations addressing key features, prevention, and management.
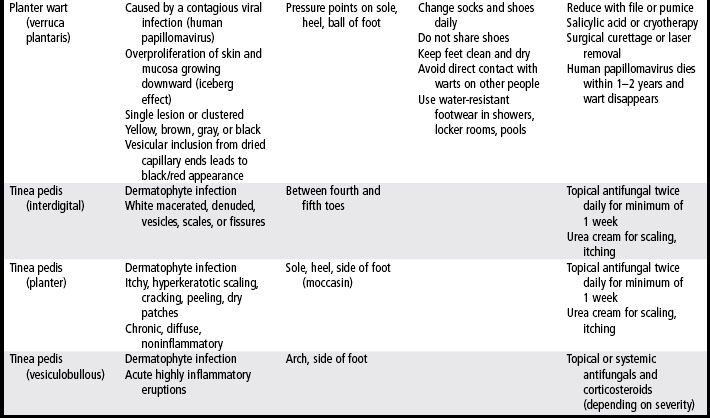
4. Describe common foot lesions, including their etiology, manifestations, treatment, and prevention.
5. Distinguish between two toenail disorders and their treatments.
6. Develop an appropriate plan for routine care of the foot.
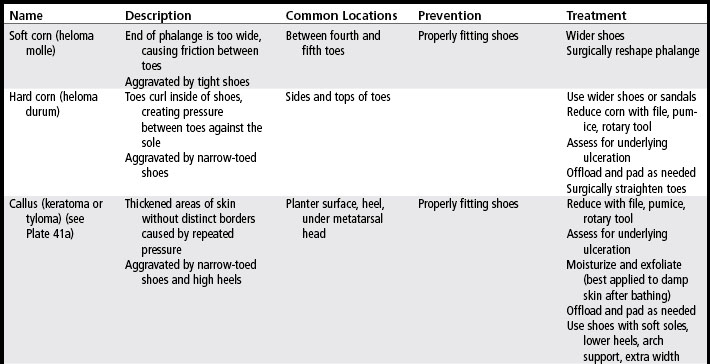
Foot problems occur in at least 75% of Americans (Menz et al, 2001). The five most common problems in the elderly population are toenail disorders (75%), toe deformities (60%), corns and calluses (58%), bunions (37%), and dry skin, fungal infections, or maceration between the toes (36%). Most of these foot problems can be prevented by proper foot care performed on a regular basis (Badlissi et al, 2005).
Chronic foot problems (i.e., those lasting more than 2 weeks) are associated with diabetes, peripheral vascular disease, neuropathy, atherosclerosis, arthritis, and obesity. In fact, the signs and symptoms of many of these systemic disorders manifest initially in the feet. Improper shoe wear, overuse, or systemic disease can trigger chronic foot pain. These issues magnify the importance of a good foot assessment (Popoola and Jenkins, 2004).
Quality of life
Foot diseases and their treatments have a tremendous impact on quality of life (Katsambas et al, 2005). In fact, patients with diabetes who have foot ulcers report a poorer quality of life than patients with diabetes who have amputations (Price and Harding, 2000). In a large-scale, quality-of-life survey of 45,593 patients with various foot diseases representing 17 countries (the Achilles Project), the researchers found that 40.3% of the respondents experienced discomfort in walking, 30.7% had pain, 27.3% had embarrassment, and 19.6% experienced limitations in their activities of daily living (Katsambas et al, 2005).
Overall, foot disease has a significantly greater effect on the quality of life of women than of men with regard to their experience of pain, discomfort in walking, and embarrassment (Katsambas et al, 2005; Leveille et al, 1998). One explanation is that the many types of shoes typically worn by women are tighter-fitting, which increases their risk of developing toenail onychomycosis, which is associated with pain and discomfort in walking.
Structure and function
The foot has two key functions: weight bearing and propulsion. To perform properly, the foot requires a high degree of stability and must be flexible to adapt to uneven surfaces. Flexibility is provided by the numerous bones and joints in the foot; these bones also form the arch to support weight (Quinn, 2009). Each foot contains 26 bones, 33 joints, and a network of more than 100 tendons, muscles, ligaments, blood vessels, nerves, and nails. Together, the feet comprise a quarter of the 206 bones in the body. An average day of walking brings a force equal to several hundred tons to bear on the feet. As such, feet are more subject to injury than is any other part of the body (Cavanagh and Ulbrecht, 2008; Mix, 1999).
Skeletal components
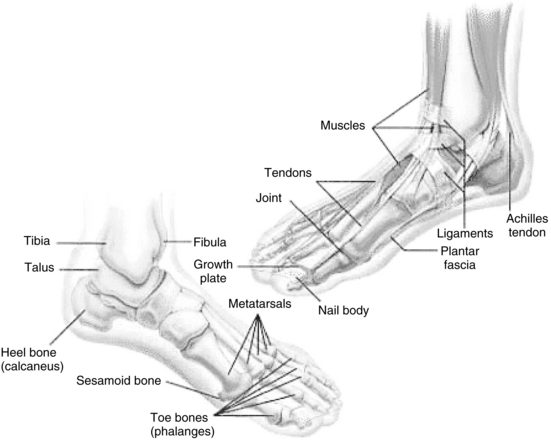
The three functional units of the foot are the hindfoot (2 bones), midfoot (5 bones), and forefoot (19 bones). All units must work together to provide both flexibility and stability (Figure 15-1).
Within the forefoot are the phalanges (toes) and the five metatarsal bones. Each toe (phalanx) is made up of several bones. The great toe (also called the hallux) consists of two phalanx bones: proximal and distal; these phalanges are larger than all the other phalanges. Phalanges two through five have three phalanx bones each: proximal, distal, and intermediate (an additional middle bone). Each phalanx is connected to a metatarsal at the metatarsophalangeal (MTP) joint; together the MTP joints form the ball of the foot. The proximal portion of a metatarsal is called the base, the middle is the shaft, and the distal is the head (Figure 15-2). Each of the five metatarsals is unique in size. The first metatarsal is the shortest in length, the largest in diameter, bears the most weight and plays the most important role in propulsion (Quinn, 2009). At the head of the first metatarsal bone on the plantar surface of the foot are two sesamoid bones that serve to attach small muscles and aid in stabilizing the first MTP joint. (A sesamoid bone is a bone imbedded within a tendon and functions to protect the tendon where it passes over a bony prominence.) The second, third, and fourth metatarsal bones are the most stable metatarsal bones. At the fifth metatarsal base is an eminence on the lateral aspect called the tuberosity of fifth metatarsal or styloid process. This area is easily palpated on the lateral aspect of the foot.
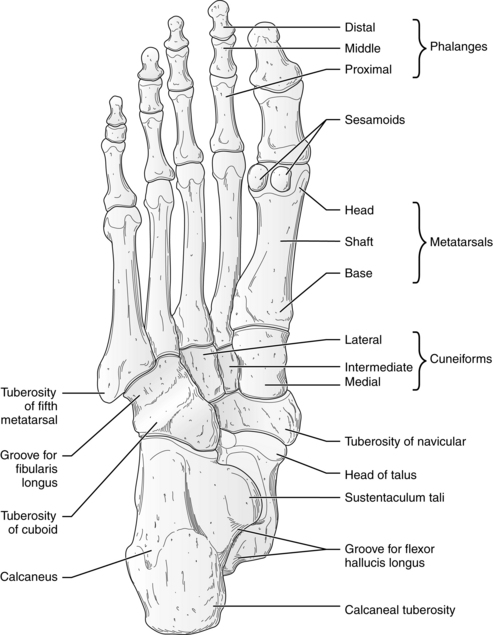
FIGURE 15-2 Dorsal view of anatomic structures of foot.
(From Jenkins DB: Hollinshead’s functional anatomy of the limbs and back, ed 9, St. Louis, 2009, Saunders/Elsevier, p 333.)
In the midfoot, five of the seven tarsal bones are located (Figure 15-2). These irregularly shaped tarsals (the navicular, cuboid, and three cuneiform) form the arch and contain multiple joints. The three cuneiform bones articulate with the navicular bone in the proximal midfoot. The midfoot connects with the forefoot at the five tarsometatarsal (TMT) joints and connects to the hindfoot by muscles and ligaments.
The hindfoot links the midfoot to the ankle and consists of two of the seven tarsal bones, the talus and the calcaneus. The talus sits on top of the calcaneus and articulates with the tibia and fibula at the calcaneus and navicular bones, allowing the foot to move up and down. The calcaneus forms the heel and is the largest tarsal and the largest bone in the foot. It allows the foot to become rigid or loose to accommodate the process of walking. It is also the cause of numerous heel-related pains (Jolly et al, 2005).
Ligaments hold the bones together at the joints. The Achilles tendon stretches from calf muscle to heel and is the largest, strongest tendon in the foot. The planter fascia is the longest ligament and forms an arch on the sole of the foot from the heel to the toes. These long fibrous strands are vulnerable to injury (e.g., a strain or sprain in the foot or ankle) because the ligaments can overstretch, break, and curl back on themselves. Over time the strain heals with scar tissue; however, the scar is never as strong as the original fibers of the ligament.
Neurovascular
As shown in Figure 10-2, the dorsalis pedis pulse is palpated or auscultated over the navicular and middle cuneiform bones. The posterior tibial pulse is palpated over the medial malleolus of the tibia.
Cutaneous and subcutaneous components
The skin on the plantar surface of the foot is thick and hairless and contains numerous sweat glands. Eccrine sweat glands are densely populated on the soles of the feet, palms, and axillae. Their primary function is thermoregulation through evaporation of sweat. The sebaceous and apocrine sweat glands empty into the upper portions of the hair follicles. Sebaceous glands produce lipid-rich sebum that prevents the skin and hair from drying out. Because the foot has little hair growth and therefore very few sebaceous glands, the foot is extremely vulnerable to dryness and xerosis.
Three anatomic areas on the plantar surface of the foot have increased fat in the form of fat pads: the calcaneus, the metatarsals, and the lateral longitudinal arch. Contained by the subcutaneous tissue, the fat pad absorbs impact and tolerates weight-bearing as a means of protecting the underlying bones. With age, these fat pads thin and provide less shock absorbency. More pressure is then exerted over the calcaneus and metatarsal. Thinning of the fat pad is accelerated by obesity, diabetes, and constant high impact. The thinning process begins as early as 30 years of age. An orthotic or insole cushioning can be used to provide additional shock absorption (Ozdemir et al, 2004).
Nail structure
Nails are made of epidermal cells converted to hard plates of keratin. The highly vascular nail bed lies beneath the plate, giving the nail its pink color. The stratum corneum layer of the skin covering the nail root is the eponychium (cuticle), which forms a seal between the nail and the digit to prevent foreign matter from entering. The paronychia is the soft tissue surrounding the nail border. The normal nail is composed of six parts: nail root, nail bed, nail plate, eponychium (cuticle), perionychium, and hyponychium as illustrated in Figure 15-3 and described in Box 15-1.
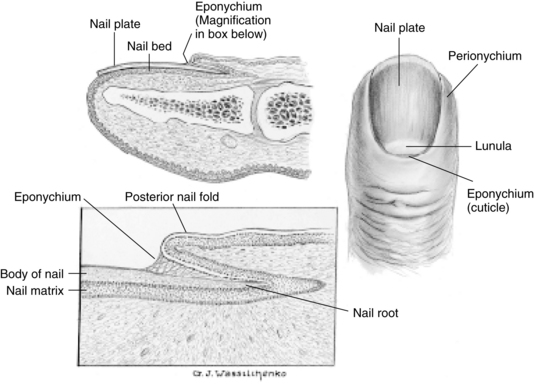
FIGURE 15-3 Anatomic structures of the nail.
(From Thompson JM et al: Mosby’s clinical nursing, ed 5, St. Louis, 2002, Mosby.)
BOX 15-1 Nail Anatomy
Nail Root (Matrix): Root of fingernail is also known as the matrix. The matrix begins 7 to 8 mm under proximal nail fold to lunula (white crescent at distal nail). Fingernail root produces most of volume of nail plate and nail bed.
Nail Bed: Part of nail matrix, under the nail plate. Extends from lunula (white crescent at distal nail) to hyponychium. Nail bed contains blood vessels, nerves, and melanocytes or melanin-producing cells. As nail is produced by root, it streams down along the nail bed, which adds material to the undersurface of the nail, making it thicker.
Nail Plate: The actual fingernail, made of translucent keratin. Pink appearance of nail comes from blood vessels underneath nail. Underneath surface of nail plate has grooves along length of nail that help anchor it to the nail bed.
Eponychium (Cuticle): Fold at proximal end of nail plate. Nail plate has very firm adhesion to the cuticle. Both epidermal structures are directly continuous with one another, overlapping the lunula. Fusing of these structures provides a waterproof barrier.
Perionychium: Skin that overlies nail plate on its sides. Also known as the paronychial edge. Site of hangnails, ingrown nails, and infection of skin called paronychia.
Hyponychium: Area between free edge of nail plate and epidermis of toe. Continuous fusing of these areas to epidermal structures provides waterproof barrier.
Periungual: Tissue around nail plate.
Subungual: Tissue under nail plate.
From Mix G: The salon professional’s guide to foot care, Albany, NY, 1998, Milady Salon Ovations.
Nails grow all the time, but their rate of growth slows with age and poor circulation. Fingernails grow faster than toenails. They grow at a rate of 3 mm per month and take 6 months to grow from root to free edge. Toenails grow approximately 1 mm per month and require 12 to 18 months to be completely replaced. Actual growth rate is dependent upon age, gender, season, exercise level, diet, and hereditary factors (Sinni-McKeehen, 2007).
Physical assessment
Components of an initial evaluation of the patient with an actual or potential foot disorder are listed in Checklist 15-1. Because so many patients with foot disorders have concomitant lower extremity disease, perfusion and sensation must be assessed (see Chapters 10, 11, 12, and 14), and a baseline health history is essential. The following discussion presents the unique assessment parameters for the foot and nail.
CHECKLIST 15-1 Components of Initial Evaluation of Patient with Foot Disorder
History
✓ Presenting complaint including detailed description of pain
✓ General: vision, strength, dexterity, mobility
✓ Blood glucose readings for past month
✓ Personal or family history: skin, hair, or nail disease (especially rashes), lichen planus, psoriasis, diabetes, heart or vascular disease, obesity
✓ Specific history of foot problems: foot malformations, lesions, skin alterations, nail disorders, changes in sensation, foot/ankle strength
✓ Current and prior treatments and medications (including over-the-counter) used to treat nail and foot problems
✓ Health habits: smoking, exercise, hygiene, nutrition, weight management
Physical assessment
Specific information should be elicited about routine care of the foot, any history of foot and nail problems, and how these problems were treated either personally or by a health care provider. Effects of prior treatments, including prescription and over-the-counter medications, should be assessed (Piraccini, 2004; Sprecher, 2005). Quality-of life-information should be solicited (Garrow et al, 2004; Vileikyte et al, 2003).
Musculoskeletal function
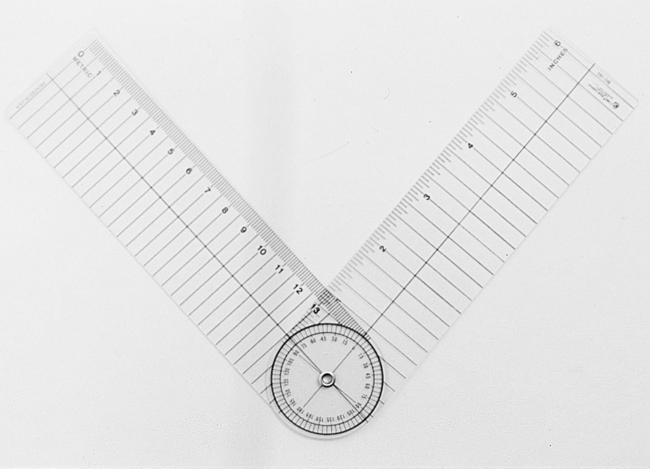
Musculoskeletal function of the foot involves assessment of range of motion, deformities, and strength. Passive range of motion of the first MTP joint and the subtalar joint should be assessed. Maximal range of motion is determined from maximal inversion to maximal eversion of the subtalar joint of the foot (Figure 15-4). If available, a goniometer can be used to quantify the arc or range of motion (Badlissi et al, 2005) (Figure 15-5). Range of motion can also be tested by supporting the heel with the hand and grasping the foot with the other hand, then moving the foot in dorsiflexion, plantar flexion, eversion, and inversion. The dorsiflexion position tests for shortening of the Achilles tendon. Inversion will be limited by a spasm of the peronei. Eversion will be limited with a rigid flat foot. Restrictions in range of motion of the ankle might limit the ability to correct a loss of balance (Duthie, 2007).
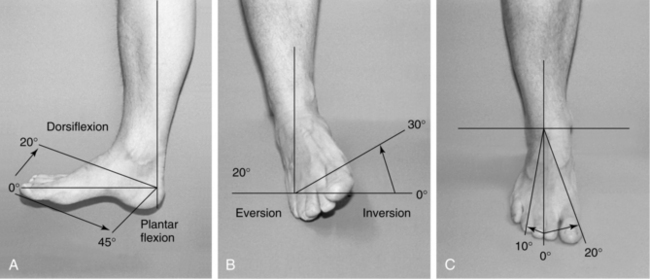
FIGURE 15-4 Range of motion of the foot and ankle.
(From Seidel HM et al: Mosby’s guide to physical examination, ed 6, St. Louis, 2006, Mosby.)
The strength of the anterior leg muscles can be tested by having the patient stand on the heels. Muscle strength can also be assessed by comparing both feet as the patient walks a few steps on the toes and then the heels. If the patient has difficulty with balance, cannot walk, or both, strength can be assessed with the patient sitting. With the clinician’s hand under the patient’s foot, the patient is asked to flex and extend the foot against resistance by “pressing down on the gas pedal.” Next, with the clinician’s hand positioned on the top of the patient’s foot and the clinician’s thumbs underneath, the patient is instructed to pull the “toes toward the nose” while the clinician applies gentle pressure downward. Any differences in strength currently or in the past 6 months should also be recorded (Frey, 2005).
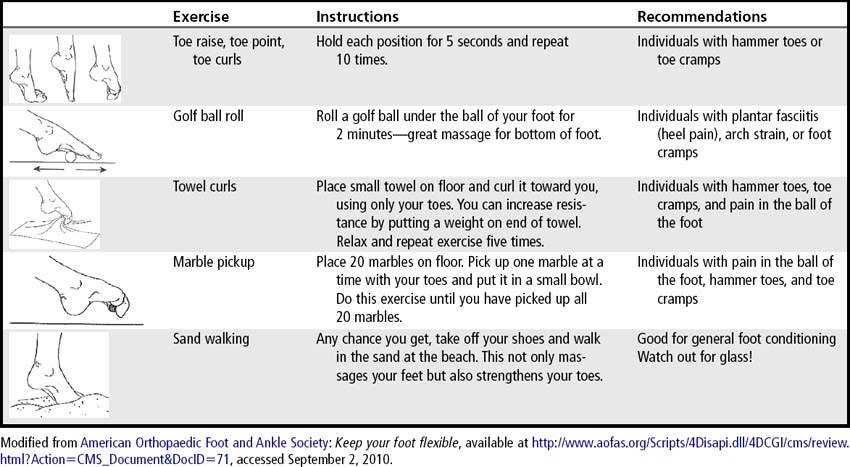
To assess toe flexibility, the patient can be instructed to pick up a marble or a small dishtowel with the toes (Table 15-1). To test ankle flexibility, the patient is instructed to stand on a stair step, hang his or her heel off a step, and let the heel drop below the level of the stair. If this motion causes pain, the exercise should be stopped. The heel should be able to drop below the level of the stair without causing strain in the calf. Some strain can be improved with flexibility exercises (Frey, 2005).
Muscle strength reflexes (deep tendon reflexes) usually show no changes in the elderly patient, although nearly half have a diminished Achilles tendon reflex. This is likely due to slow nerve conduction and decreased tendon elasticity. Hyperactive deep tendon reflexes suggest upper motor neuron disease; hypoactive reflexes suggest lower motor neuron dysfunction. Tone is assessed through passive motion. Increased tone is suggestive of upper motor neuron dysfunction; decreased tone is suggestive of lower motor neuron dysfunction.
Functional ability
The patient’s functional ability is a significant factor influencing his or her ability for self-care and safety. Assessments of functional ability should address cognition, vision, strength–hand dexterity, coordination, balance, proprioception, and gait. Because key interventions in the prevention and management of foot and nail disorders are patient education and self-care, the patient will need adequate cognition to conduct self-care or communicate pain. Vision and strength–hand dexterity are essential so that patients will be able to inspect their feet and remove footwear (Duthie, 2007). Many of these functional abilities can be assessed through observation and demonstration return.
Coordination can be determined with a rapid alternating movement that includes heel to shin testing. Another test in which the patient taps the feet rhythmically against the floor will assess the accuracy and reproducibility of endpoints as well as the ability to maintain motor movements over time. The coordination testing is documented qualitatively because no quantification guidelines are available (Duthie, 2007).
The Romberg test (Box 15-2) is positive in the patient with proprioception disturbances (Jarvis, 2004). In addition, the patient’s gait may be slightly wide while the stride length is normal or a little reduced (Willacy, 2008). Gait should be assessed without an assistive device if possible so as not to mask deviations. Proprioception and vibration sense are carried by the same nerve pathways. Therefore, testing vibration may reveal proprioception disturbances. To test vibration sense, a 128-Hz tuning fork is applied over a bony prominence such as the medial malleolus and the patient is asked to report when the vibration stops (Jarvis, 2004).
Condition of legs, feet, toes, and nails
Lower extremity assessment should include all of the components discussed in Chapter 10. In addition to examining skin integrity, color changes, sensation, pain, and vascular conditions, the foot must be inspected for skin that is too dry or too moist, evidence of fungal or bacterial infection, lesions, foot malformations, and nail conditions (Boulton and Armstrong, 2008). All surfaces (dorsal, plantar, medial, lateral, posterior surfaces) of the heel, areas between the toes (interdigitally), and each nail should be examined. Note the character of skin changes from the proximal leg to the distal foot. Compare the skin on the lower extremity and feet to the skin on the arms and hands.
Ulceration and amputation risk
The data collected during the examination will assist in identifying risk for ulceration and amputation. Risk assessment tools with management strategies are given in Tables 14-2 and 14-3. Risk factors include history of plantar ulcer, presence of foot deformity, presence of protective sensations, and presence of diseases that lead to decreased sensation. Risk categories range from 0 (no risk) to 3 (greatest risk). The level of risk determines the patient’s management strategy. Yetzer (2004) recommends foot examinations at each visit (at least four times per year) regardless of risk score.
Prevention and routine management
Routine foot hygiene
Routine foot care includes daily inspection and moisturizing. Cleansing and bathing should be based on the individual needs of the patient and should consist of mild skin cleansers and lukewarm water to minimize drying effects. After bathing, the feet must be dried completely, especially between the toes. Patients should wear socks to provide extra padding to bony prominences and to wick away moisture from the skin. Socks may need to be changed more than once per day if feet sweat excessively.
Maceration between the toes (interdigital) and under the toes (subdigital) is a very common foot problem. Such overhydration of the skin, characterized by a white, “waterlogged” appearance, weakens collagen, promotes overgrowth of bacterial and fungal species of skin flora, and decreases the skin’s ability to resist trauma (Kelechi, 2005; Stroud and Kelechi, 2006). Pseudomonads as well as gram-negative organisms are common etiologic agents (Schwartz, 2009). Overhydration of the skin can occur with excessive perspiration (hyperhidrosis) related to endocrine, neurologic, or sweat gland disorders.
Maceration is prevented by keeping the skin dry and protected. Absorbent foot powder (e.g., Zeasorb) can be used twice per day. After bathing, the patient should pay special attention to drying the interdigit spaces; using a hair dryer on a cool setting may be helpful. Skin sealants may be used to protect the skin from moisture. If maceration persists after 1 week of care, consider the presence of interdigital tinea (Table 15-2) or superimposed bacterial infection. Treatment includes drying the interdigital web spaces, topical econazole, and daily to three times a day local application of Castellani paint (a drying agent containing 1.5% phenol in a water and alcohol base) (Schwartz, 2009).
Foot odor is caused by excessive perspiration from the more than 250,000 sweat glands in the foot. Bacteria living in shoes and socks metabolize the sweat to form isovaleric acid, which is responsible for foot odor. In addition to washing the feet and changing shoes and socks even more frequently than daily, the patient can dust the feet with a nonmedicated spray, foot powder, or antiperspirants. Soaking feet in vinegar and water can help lessen odor (American Podiatric Medical Association, 2010). Severe cases of foot odor may be caused by hyperhidrosis (excessive perspiration formation related to endocrine, neurologic, or sweat gland disorders). The prescription-strength antiperspirant Drysol can be used if over-the-counter antiperspirants or sprays fail (Hill, 2010). In severe cases the nerve controlling the sweat glands in the feet may be surgically severed, but compensatory sweating in other areas of the body may occur after surgery.
Anhidrosis (inability to produce sweat) is associated with autonomic dysfunction caused by endocrine or neurologic disorders, environmental conditions, and aging. Xerosis is a consequence of the skin’s loss of natural moisturizing factors and loss of moisture from the stratum corneum and intercellular matrix (Hill, 2008). Clinically, xerosis appears as excessively dry, rough, uneven, and cracked skin. Raised or uplifted skin edges (scaling), desquamation (flaking), chapping, and pruritus may be present. This condition occurs particularly on the heels and bottoms of the feet. A person who has a decrease or loss of function of the sweat glands on the plantar surface of the foot will experience xerosis or anhidrosis of the feet (Kelechi, 2005). Xerosis can lead to fissures (linear cracks in the skin), which may serve as a portal of entry for bacteria. Consequently, fissures are associated with increased risk of cellulitis and foot ulceration (Hill, 2008). Fissures are treated with humectants and exfoliant moisturizers or sealants, such as Dermabond. Prevention includes ongoing use of moisturizers and exfoliants and wearing of shoes that do not flop at the heel. Hyperkeratotic tissue is common around fissures and often necessitates debridement and exfoliation. Table 15-3 provides a formulary of products for the prevention and treatment of dry skin.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree