5 Foot and Ankle Injuries
Ankle Sprains
Ankle sprains are common injuries in active individuals, with an estimated incidence of 61 ankle sprains per 10,000 persons each year (Maffulli and Ferran 2008). They are the most common injury sustained by high school and collegiate athletes, accounting for up to 30% of sports injuries (Hass et al. 2010). An age of 10 to 19 years old is associated with higher rates of ankle sprains. Half of all ankle sprains occur during athletic activity. Although most of these injuries respond well to conservative therapy, chronic instability and dysfunction are known risks. In a study of 202 elite track and field athletes with lateral ankle sprains, Malliaropoulos et al. (2009) found that 18% sustained a second sprain within 24 months; low-grade acute ankle sprains (grade I or II) resulted in a higher risk of reinjury than high-grade (grade III) sprains. Because of the potential for reinjury and chronic dysfunction and the importance of a normally functioning ankle in active people, it is important that ankle sprains be managed correctly with a thorough rehabilitation and reconditioning program.
Relevant Anatomy
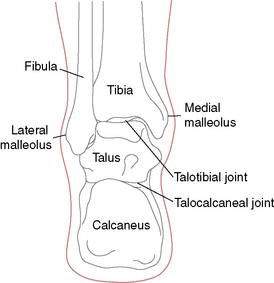
The ankle, or talocrural joint, is a junction of the tibia, fibula, and talus (Fig. 5-1). The anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL) provide static support to the joint laterally (Fig. 5-2A), whereas the deltoid ligament complex (DLC), made up of the anterior and posterior tibiotalar ligaments, the tibiocalcaneal ligament, and the tibionavicular ligament, provides medial support (Fig. 5-2B). The inferior anterior and posterior tibiofibular ligaments and the interosseous membrane provide additional support for the talocrural joint (Fig. 5-2C and D).
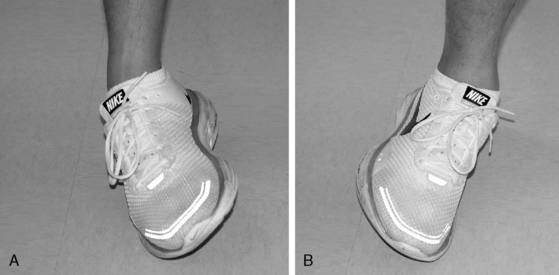
The ATFL is the most commonly injured ligament, followed by the CFL. The CFL is usually injured in combination with the ATFL. Sprains to both the ATFL and CFL are a result of a combined inversion and plantarflexion mechanism (Fig. 5-3A). A less likely mechanism of eversion may cause injury to the DLC (Fig. 5-3B). Injury to the anterior and posterior tibiofibular ligaments (syndesmosis) and the interosseous membrane are discussed later in this chapter.
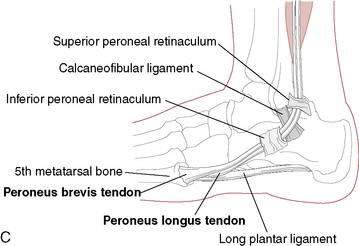
The muscles that attach to and act upon the foot provide dynamic control of the ankle. The peroneal muscle group, composed of the peroneus brevis, longus, and tertius muscles, is of significant importance because they are responsible for everting the ankle and, therefore, resisting inversion (Fig. 5-3C). Because there are no muscles that attach directly to the talus, motion of the talus is dictated by foot and ankle position. The most stable position of the ankle is in dorsiflexion. As the foot moves into dorsiflexion, the talus glides posteriorly and the widest portion of the talus becomes wedged into the ankle mortise. As the ankle moves into plantarflexion, the talus glides anteriorly and the ankle becomes less stable, which is why most ankle sprains involve some degree of plantarflexion as the mechanism.
Classification of Ankle Sprains
Diagnosis
It is only through a thorough examination that the severity of an ankle sprain can be established (Table 5-1). Detailed information on conducting a thorough examination of the ankle is beyond the scope of this text; however, common signs and symptoms associated with each grade of lateral ankle sprain are listed in Table 5-2. The examiner must also be aware of additional injuries that can occur with ankle sprains. Such injuries include, but are not limited to, avulsion fractures, fractures, muscle and tendon strains, articular cartilage damage of the ankle mortise, and tarsal subluxations and dislocations. Although some of these injuries (such as muscle strains) can be adequately treated with the following standard treatment protocol, others (such as articular cartilage damage) may require revisions of the standard treatment protocol for ankle sprains.
Table 5-1 Examination of the Ankle After an Inversion Injury
| Palpation of the Lateral Collaterals (Anterior Talofibular Ligament and Calcaneofibular Ligament) |
| Medial palpation of the deltoid ligament |
| Palpation of the proximal fibula close to the knee to rule out a Maisonneuve fracture (tearing of the interosseous membrane and proximal fibula fracture) |
| Squeeze test to rule out ankle syndesmosis tearing with resultant ankle mortise instability |
| External rotation (Cotton) test to test for syndesmosis injury |
| Palpation of the proximal (base) fifth metatarsal to rule out avulsion fracture from peroneus brevis pull |
| Anterior Drawer and Inversion (Talar Tilt) Stress Testing |
| Motor testing of posterior tibial (inversion) and peroneal tendons (eversion) |
Table 5-2 Clinical Signs and Symptoms Associated with Ankle Sprains
| Grade I | Grade II | Grade III |
|---|---|---|
| Stretching of ligaments, usually the ATFL Point tenderness Limited dysfunction No laxity Able to bear full weight Little to no edema | Partial tearing of ligaments, usually the ATFL and CFL Point and diffuse tenderness Moderate dysfunction Slight to moderate laxity Antalgic gait and pain with FWB, may need supportive device to ambulate Mild to moderate edema | Substantial tearing of ligaments, may involve the PTFL in addition to the ATFL and CFL Point and diffuse tenderness Moderate to severe dysfunction Moderate to severe laxity Limited to no ability for FWB without supportive device Severe edema |
ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; FWB, full weightbearing; PTFL, posterior talofibular ligament.
Treatment and Rehabilitation Protocol for Acute Ankle Sprain
Without ignoring where the injury is in the healing process, the clinician should progressively manage the patient’s signs and symptoms, functional limitations, and impairments instead of solely focusing on the number of days since the injury. Table 5-3 lists the common signs and symptoms associated with each stage of tissue healing. Changes in the signs and symptoms, in addition to the number of days postinjury, can help the clinician determine when to progress the patient’s treatment and rehabilitation program.
Table 5-3 Clinical Signs and Symptoms Associated with the Stages of Tissue Healing
| Acute Stage | Subacute Stage | Maturation Stage |
|---|---|---|
| Pain at rest, ⇑ w/ activity TTP ⇑ swelling Heat Protective guarding and muscle spasm Loss of function* Restricted and painful ROM Laxity w/ stress tests* | ⇓ pain, TTP, swelling, heat ⇓ spasm and guarding ⇑ function ⇑ ROM w/ ⇓ pain ⇓ laxity w/ stress tests* | No s/s of inflammation ⇑ function ⇑ ROM |
⇑, increased; TTP, tenderness to palpation; ROM, range of motion; ⇓, decreased; s/s, signs and symptoms.
* Presence and amount depend on severity of sprain.
The steps in treating and rehabilitating ankle sprains typically follow this progression:
While the rehabilitation program is progressing through these steps that focus on the injured ankle, it is important to maintain overall strength and conditioning for the rest of the body. Rehabilitation Protocol 5-1 provides an outline of the ankle sprain rehabilitation protocol described here.
REHABILITATION PROTOCOL 5-1 Ankle Sprain Rehabilitation
Lateral Ankle Sprain
Acute Phase
Goal: Protect from further injury
Goal: Encourage tissue healing
Goal: Limit pain, swelling, spasm
Goal: Maintain function of noninjured tissues
Goal: Maintain overall body conditioning
Subacute Phase
Goal: Minimize pain and inflammation
Goal: Restore range of motion and flexibility
Goal: Re-establish neuromuscular control and restore muscular strength and endurance
Goal: Re-establish proprioception, agility, and coordination
Goal: Maintain overall body conditioning
Maturation Phase:
Goal: Restore ROM and flexibility
Goal: Improve muscular strength, endurance, and power
Goal: Improve proprioception, agility, and coordination
Goal: Restore functional/sports-specific skills
Goal: Maintain overall body conditioning
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree