The true incidence of ankle fractures in the general population is unknown, as it changes with increased participation in athletics and trends in fashion footwear. There is also a great deal of interobserver reliability when it comes to classifying these fractures.
A great deal of research has been conducted to determine the incidence of age-related fractures, particularly in the elderly population. Barrett et al. (1) analyzed Medicare data in 1999 and found that ankle fractures were the fourth most common fracture in the elderly population (65-90 years of age). The study also demonstrated that elderly blacks were less likely than whites to fracture the ankle.
The examination of the ankle should begin with a thorough visual inspection noting abnormal swelling, redness, or deformities. The physician should also palpate the ankle to determine the extent of any swelling, identify any abnormal bony prominences or incongruities, determine specific areas of point tenderness or extreme pain, and evaluate the neurovascular status of the patient.
The neurovascular examination should include an assessment of the dorsalis pedis and posterior tibial pulses. Additionally, the physician should evaluate the capillary refill, light touch, and two-point discrimination distal to the ankle.
Gross deformity of the ankle is a likely indicator of dislocation, which should be reduced and splinted prior to radiographic examination or further evaluation.
The physician will then evaluate the range of motion of the ankle. The normal range of ankle motion is 30 degrees of dorsiflexion and 45 degrees of plantarflexion. The range of motion necessary for ankle functionality or ambulation is 10 degrees of dorsiflexion and 20 degrees of plantarflexion (21).
It is important to evaluate the stability of the ankle when suspecting a fracture. The squeeze test is performed to rule out disruption of the tibiofibular syndesmosis. The squeeze test is performed by squeezing the leg, approximating the tibia and fibula, at or slightly above the level of the belly of the gastrocnemius. An indicator of syndesmotic disruption is pain at the distal tibiofibular articulation when the squeeze test is performed (18). The physician should also perform an anterior drawer test to evaluate the laxity of the complex ligamentous support network of the ankle. Pain with dorsiflexion and external rotation should also be noted because this may represent posterior bony injury or tendinous disruption.
The Ottawa ankle rules are a valuable guideline in determining the need for radiographic examination in a patient suspected to have an ankle fracture. Radiographic examination is required if the patient is unable to bear weight, if the patient has pain with palpation within 6 cm proximal or distal to the talar articulation, or if the patient has bony tenderness at the posterior edge or tip of either malleolus (34).
The ankle is best examined radiographically with an anteroposterior (AP), lateral, and mortise view. Three-view radiographs demonstrate greater reliability when compared to various combinations of two-view radiographs (4). Abnormal radiographic findings are greater than 2 mm of talar tilt (difference in lateral and medial joint spaces in AP view), misalignment of the talar dome under the tibia in AP or lateral views, and a demonstrated tibiofibular overlap of less than 10 mm in the AP view or the mortise view (25). Stress radiographs may be valuable but are difficult to standardize. Patients are most tolerant of the gravity stress test whereby a mortise view of the ankle is obtained with the patient lying on their injured side and their distal tibia and injured ankle off of the table unsupported (32). Although normative data are not adequately reported in the literature, the Telos stress device is being used to standardize the amount of stress about the ankle during routine radiographic stress examinations.
Magnetic resonance imaging (MRI) is best suited for the examination of the integrity of the ankle ligaments, and a bone scan is often helpful to rule out osteochondral lesions in patients with chronic ankle injuries.
There are three primary classification systems used to define ankle fractures. The Danis-Weber classification is based solely on the fibula and the location of the fracture in relation to the ankle mortise (10). The Lauge-Hansen classification describes the ankle fracture according to foot position and movement of the foot in relation to the leg (supination-adduction, supination-external rotation, pronation-abduction, pronation-eversion, and pronation-dorsiflexion). The most common mechanism of ankle fracture is of the supination-external rotation variety (22). Lastly, the AO classification is based on the level of the fibula fracture, medial malleolar involvement, and syndesmotic disruption (16). A summary of the aforementioned classifications can be found in Table 66.1.
The goal of treatment of ankle fractures is to restore the anatomic congruity of the ankle joint, promote pain-free restoration of range of motion, and restore and maintain fibular length.
Nondisplaced, stable ankle fractures and stable, reduced ankle fractures can be managed nonoperatively with great success. Once swelling is reduced, long leg casting is indicated with transition to short leg cast or fracture bracing after 4-6 weeks (25). Diabetics are a special subgroup of patients who may need more time in the long leg cast before adequate bone growth is evident and are less likely candidates for operative intervention. Recent studies suggest that diabetics have higher postoperative complication rates when compared to nondiabetics. Blotter et al. (3) reported a 43% complication rate in diabetics as compared to a 15% complication rate in nondiabetics. Diabetics also demonstrate a higher postoperative infection rate after ankle surgery as reported by Flynn et al. (14) in 2000 and Leyes et al. (23) in 2003.
Table 66.1 Classification Systems of Ankle Fractures
Fracture Classification
Type
Location of Fracture
Associated Injuries
Danis-Weber
A
Below ankle mortise and tibiofibular articulation
Syndesmosis likely intact
B
At level of mortise and tibiofibular articulation
Syndesmosis likely intact
C
Above level of mortise and tibiofibular articulation
Likely disruption of syndesmosis with positive squeeze test
Lauge-Hansen
Supination-adduction
Transverse fracture of lateral malleolus
Stage 1: Tear of lateral ligaments
Stage 2: Fracture of medial malleolus
Supination-external rotation
Avulsion fracture of lateral malleolus
Stage 1: Rupture of anterior tibiofibular ligament
Stage 2: Spiral or oblique fracture of lateral malleolus
Stage 3: Posterior tibial fracture
Stage 4: Fracture of medial malleolus or torn deltoid ligament
Pronation-abduction
Medial malleolus
Stage 1: Torn deltoid ligament
Stage 2: Syndesmotic disruption and posterior tibial fracture
Stage 3: Oblique fracture of fibula above mortise
Pronation-external rotation
Medial malleolus
Stage 1: Torn deltoid ligament
Stage 2: Syndesmotic disruption
Stage 3: Spiral fracture of fibula above mortise
Stage 4: Posterior tibial fracture
AO
A
Fibula at or below plafond
Intact or possible avulsions medial and posterior
B
Fibula at plafond extending proximally
Tibiofibular ligaments torn; possible avulsions medially and posteriorly
C
Fibula above plafond
Syndesmosis always torn; deltoid ligament torn
Displaced, unstable, open, or unreducible ankle fractures must be treated operatively with reduction and internal or external fixation (8,35).
Open fractures require emergent orthopedic consult, and it is very likely that these patients will be taken to the operating room urgently. Studies have shown that most open ankle fractures are associated with wounds less than 1 cm long and that infection rates after operative treatment of these fractures are comparable to infection rates seen in the treatment of closed fractures. Chapman and Mahoney (7) demonstrated in their series of open ankle fractures in which immediate fixation was achieved, that the rate of infection in open fracture wounds less than 1 cm was 2% and the rate of infection in open fracture wounds with extensive soft tissue damage and wounds greater than 1 cm was 29%.
The most important aspects of ankle fracture management are to immediately reduce dislocated ankles prior to radiographic study, clean and dress open wounds in a proper sterile fashion, document and evaluate neurovascular status, and apply a posterior splint with a U-shaped component at the ankle when transporting the patient or preparing them for further workup by an orthopedic surgeon.
The foot comprises a total of 26 bones. The hindfoot consists of the talus and calcaneus, whereas the midfoot includes the navicular, cuboid, and cuneiforms, and their articulations with the proximal metatarsals. The metatarsals and phalanges make up the forefoot.
Most foot injuries involve innocuous sprains; however, a small percentage of them involve significant injuries with subtle radiographic findings. The rarity of these injuries limits physician familiarity and accounts for frequent misdiagnosis (36). Foot injuries involving the talus are the most often misdiagnosed (20).
Fractures of the talus are the second most common tarsal bone injury, with an incidence ranging from 0.1% to 0.85% of all fractures (30).
The talus has five articulating surfaces as 60% of the talus is covered with articular cartilage. There are no muscle or tendinous attachments. Blood supply to the talus is tenuous, and fractures can easily disrupt the blood supply, resulting in osteonecrosis (15).
Talus fractures can occur at the talar head, neck, body, or lateral or posterior processes. An os trigonum remains a separate ossicle in 14% of normal feet and can sometimes be mistaken for an acute fracture posterior to the lateral tubercle of the talus (2).
Patients with fractures of the talus may present with swelling and ecchymosis of the hindfoot or midfoot. Pain with palpation or with motion of the hindfoot should raise suspicion for the presence of a fracture.
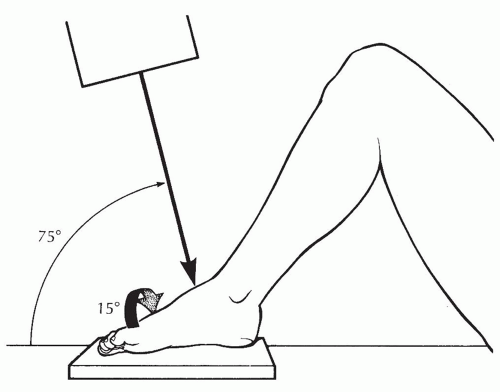
Physicians evaluating talus fractures should obtain three-view radiographs of both the foot and ankle. The Canale view can provide an optimal view of the talar neck (6). This is performed with the foot placed flat on the cassette and the ankle in equinus and pronated 15 degrees with the beam directed 15 degrees cephalad from the vertical (Fig. 66.1).
Computed tomography (CT) is indicated when displacement cannot be ruled out with plain radiographs. A CT will assist with characterization of fracture patterns, displacement, and articular involvement. The role of bone scans or MRI is limited to the evaluation of occult fractures or cartilage lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree