The foot is the link between the body and the surface that it moves across. Four interrelated requirements permit this everyday feat to occur.
The foot must be stable, allowing weight-bearing at rest, and capable of absorbing the accelerations and decelerations of walking and running. These forces can be up to 5.5 times an individual’s body weight.
The foot must be flexible and able to adapt and provide optimum contact with the surface in various positions.
The foot must act as a sensory organ, providing information to the central nervous system about pressure, temperature, vibration, and its position in space.
The foot acts as a propulsion unit, responding to central nervous system inputs to move the body through space.
These four characteristics enable the human body to move with minimal expended energy. As an organic system, the foot is subject to some of the highest mechanical stresses in the body, yet it is an end organ with respect to its vascular supply. The combination of high mechanical stresses and lack of collateral vascular supply predispose the foot to demonstrate disorders early in the disease process.
Most foot disorders fall into three major categories:
– Biomechanical
– Infectious
– Manifestations of systemic disease
The aging process can exacerbate existing foot disorders or create new ones.
The pathophysiology of most foot disorders is complex. Both osseous and soft tissues are involved. Biomechanical factors are related to all foot disorders because of the static and dynamic stresses imposed by the body. Also to be considered is the fact that hip and knee disorders can impose abnormal loads on the foot.
When examining the foot, precise evaluation and documentation of physical characteristics is required. These normal variables are appearance, contour, and mobility. These variables are used to classify the foot.
7.2 Clinical Examination
Clinical examination of the foot should begin with a complete examination to exclude other diseases that might be responsible for the reported symptoms. Examine the patient for gout and rheumatoid arthritis, and for changes in the lumbar or sacral region of the spine.
Pay special attention to axial deviations in the lower extremities. These may influence the structural mechanics of the foot.
Examining the hands often provides useful information, especially in the presence of gout, rheumatoid arthritis, psoriasis, and Dupuytren contracture. Moist warm palms and evidence of nail biting are valuable signs of the patient’s autonomous and psychological condition.
Standard Examination
Both feet should be examined and compared. The legs should be bare, from the knees down at least. All deformities such as flatfoot, metatarsus varus, and varicosities are evaluated with the patient standing as they will be more pronounced during weight bearing than when the patient is supine.
The form of the foot including its height, circumference, width, and the relative size of the forefoot and calcaneal region are described. Document the size of both feet. If there are significant deviations between the feet, shoes of different sizes will be required. Identify valgus or varus deformities of the heel and arthropathy or hypertrophy of the calf from behind the standing patient. Then have the patient walk back and forth in a relaxed, natural manner and observe the motion of the foot and ankle.
Toe walking, heel walking, and walking on the lateral edge of the foot are rough indications of muscular control and stabilization of the foot. Difficulty or inability to perform any one of these gaits will require more detailed examination of muscular status.
Document the range of motion of the ankle and midfoot in plantar flexion and dorsiflexion, and in pronation and supination, using the neutral-0 method. It is difficult to completely separate pronation and supination from adduction and abduction of the forefoot. For this reason, inversion is a more suitable term as it refers to a combination of adduction and supination. Similarly, eversion describes the combination of abduction and supination. Document the range of motion in flexion and extension of the metatarsophalangeal joints and the proximal and distal interphalangeal joints. Describe any differences in active and passive ranges of motion, joint crepitus, or painfully limited motion at the end of the range of motion, as well as dislocations, subluxations, or rigid joint deformities.
The examination should also include palpation of the pulse of the dorsalis pedis artery distal to the ankle between the tendons of the flexor hallucis longue and the flexor digitorum longus, and of the posterior tibial artery posterior to the medial malleolus. Palpate the courses of the tendons of the peroneal group, extensors, and flexors. In addition, evaluate the tone of the subcutaneous tissue and bursa.
Patient History
The history should cover four areas:
– Evaluation of systemic disorders.
– Identification of changes with secondary effects on. the foot, and occupational and athletic stresses.
– Description of localized foot symptoms.
– Previous injuries and treatments.
Systemic Disorders
Certain systemic disorders tend to involve the foot. Frequently the foot will be the site where systemic disorders are manifested. Such diseases include diabetes mellitus, peripheral vascular disease, gout, psoriasis, collagen diseases, and rheumatoid arthritis.
Peripheral vascular disease can occur with diabetes mellitus. There will be both large and small vessel involvement. The end result is ulcerative lesions of the foot.
Congestive heart failure or impaired venous or lymphatic drainage can cause bilateral edema of the feet.
Inquire in detail about any previous medical or surgical events. The same applies to medication allergies.
The history should be supplemented by laboratory tests, particularly of serum glucose levels. A glucose-tolerance test is indicated in the presence of borderline normal-to-elevated blood glucose levels to exclude latent diabetes mellitus. The uric acid level can be important for identifying foot symptoms.
Document any congenital disorders as they are frequently associated with foot deformities that do not respond to treatment.
For example, arthrogryposis multiplex congenita should be distinguished from true clubfoot. Congenital hip subluxation or dislocation is associated with clubfoot; radiographic or ultrasound examination of the hip is indicated wherever clubfoot is diagnosed.
Neurologic disorders such as peroneal muscular atrophy (Charcot–Marie–Tooth disease), neurofibromatosis, and Friedreich’s ataxia frequently affect the foot in young patients. Three-quarters of patients with Friedreich’s ataxia have associated pes cavus and scoliosis. In most cases, peroneal muscular atrophy develops into pes cavus. However, in neurofibromatosis, the soft tissue can produce gigantism of the foot or of one or more toes.
Disorders with Foot Manifestations
Axial deviation and abnormal rotation can produce secondary foot symptoms. For example, an internal rotation deformity of the tibia can lead to a flatfoot deformity.
Other disorders of the central nervous system can present with foot pain. These include spina bifida and herniated lumbar disks, which can cause radicular symptoms such as pain in one side of the foot. Back pain is not necessarily always present in herniated lumbar disks.
Also inquire about foot stresses in occupation and advocation. Ballet and other professional dances predispose the patient to sesamoiditis, synovitis, and osteoarthritis because of the stresses caused by tiptoe positions. Be prepared to distinguish sesamoiditis from osteochondritis of the sesamoid. Sports such as volleyball and soccer involve an increased incidence of tendonitis, neuropathy, tenosynovitis, bursitis, and ligament injuries.
Local Foot Symptoms
The type, intensity, duration of symptoms, and causes of local foot symptoms should be described. Gout frequently begins as an acute disorder, associated with heightened sensitivity and pain during motion. Morton’s neuroma of the interdigital nerve frequently manifests itself only during exercise or when the patient wears tight shoes. Osteoid osteomas in the foot can be effectively treated with aspirin so that a diagnosis by trial of treatment can be made. Intermittent claudication permits diagnosis of peripheral occlusive vascular disease. Pain while walking on uneven surfaces, such as a broken pavement, suggests subtalar pathology.
The quality of pain is also useful in arriving at a diagnosis. Burning pain under the heads of the metatarsals is typical of anterior metatarsalgia with hyperkeratosis. The pain in heel spur syndrome typically appears with initial weight bearing, such as when taking the first few steps in the morning. This is an intense stabbing pain. However, a heel spur may also be totally asymptomatic (Fig. 7.1).
There are patients who, for reasons best known to themselves, describe various symptoms and pains that cannot be objectively demonstrated. These patients frequently describe multiple, varying symptoms that do not have an anatomic basis. Objective findings are absent. Local anesthetics are often ineffective in these patients. Despite this overlay of non-organic pathology, these patients can suffer from actual foot disorders.
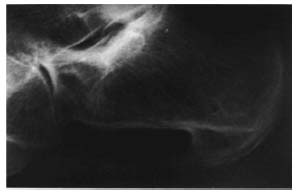
Fig. 7.1 Prominent heel spur in a 68-year old female patient without clinical symptoms (incidental finding during diagnostic studies for a foreign body).
Previous Foot Injuries and Treatments
The history must document any information about previous injuries to the legs and feet and the treatment of these injuries.
Immobilization in a short-leg cast or traction with a Steinmann pin through the calcaneus can lead to pain and stiffness in the subtalar joint, even if the original injury was not in the foot.
Occasionally foreign-body granulomas can be responsible for foot symptoms. These granulomas may be due to injuries from thorns or splinters that the patient no longer remembers.
Ask the patient about all previous foot symptoms and treatments. Even questioning about the type of previous examinations can be helpful. You may want to request examination material from the previous attending physician. Also inquire about orthotics.
Many patients are unable to explain where they hurt, or how they were injured. Often this can give rise to verbal misunderstanding. To avoid confusion, the patient’s feet and calves should always be exposed for the examination, and the patient should indicate the points of greatest pain himself or herself. It may be helpful to have the patient demonstrate the mechanism of injury because terms like “twisting to the inside or outside” are often misunderstood. The patient’s demonstration of the mechanism of injury is usually more reliable.
Observation
Inspection of the foot includes describing the shape of the foot, its position, and noting vascular changes and skin eruptions.
The shape of the foot may be categorized according to the length of the lesser toes in relation to the great toe. The Egyptian form, in which the great toe exceeds the length of the lesser toes, is distinguished from the Greek form, in which the length of the first digit is less than that of the others, and from the intermediate or square form (Figs. 7.2a-c).
Measure the width of the forefoot and hindfoot during weight bearing and at rest. The full extent of splayfoot and metatarsus varus is only apparent when the foot is bearing weight with the patient standing.
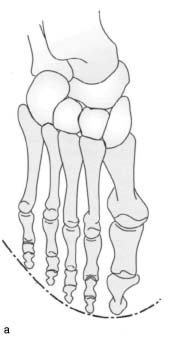
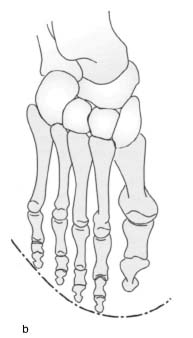
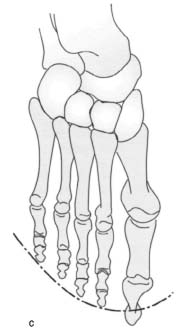
Figs. 7.2a-c Foot shapes, (a) Square, (b) Creek, (c) Indifferent or Egyptian.
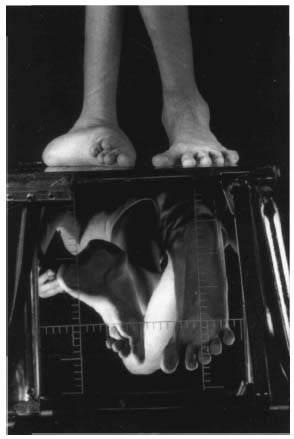
Fig. 7.3 Image of the foot of a 16-year-old boy with Marfan syndrome and right-sided spastic hemiplegia on a podometer. Disintegration of the ankle and extreme talipes valgus can be seen in the right foot. The sole bears almost no weight and the heel and the head of the first metatarsal are subject to medial weight bearing.
The position of the hindfoot relative to the horizontal plane or the longitudinal axis of the dorsal distal calf can be measured using a protractor of transparent plastic to document varus or valgus deformities. The degree to which a valgus deformity of the heel may straighten out when the patient stands on tiptoe is an important sign of the flexibility of the deformity.
Deviations in adduction and abduction can be clinically determined by evaluating the axial alignment of the heel and tarsals, as can pronation and supination deformities.
The height of the medial longitudinal arch of the foot is described while bearing weight and at rest. When examining the arch, note the pattern of calluses on the sole, as well as the position of the calcaneal region relative to the metatarsus and the position of the metatarsus relative to the forefoot.
Describe the coloration, consistency, size, location, mobility, temperature, and painfulness of any prominences such as swelling, exostoses, or joint effusions. Also document the location and size of any calluses.
Evaluate the alignment of the toes. Document any axial deviation, deformities, subduction, or superduction. Record any joint deformities, contractures, subluxations, or dislocations, proceeding from proximal to distal and from the great toe to the fifth toe. There are four degrees of deformity:
– Grade 0: no deformity
– Grade I: dynamic deformity
– Grade II : contracted deformity
– Grade III : dislocation
For example, a contracted hammer toe in the proximal interphalangeal joint of the second toe, accompanied by a dynamic deformity in the metatarsophalangeal joint, is documented as follows: hammer toe MTP 2 grade I – PIP 2 grade II – DIP 2 grade 0.
A podometer is outstanding for quickly quantifying foot deformities. The feet are placed on a glass plate illuminated from below. A mirror beneath the glass plate reveals the distribution of weight-bearing surfaces on the sole of the foot. The device is particularly suitable for photographic documentation because the foot is simultaneously visible from the front or back and from the sole with its weight-bearing surfaces (Fig. 7.3).
Pes Planus
The term “pes planus” includes all foot deformities involving an extremely low or nonexistent medial longitudinal arch. Normally, the talar head and/or navicular in the inferomedial aspect will be prominent in pes planus. Abduction of the forefoot will be more or less pronounced, and the great toe will be pronated with hallux valgus. Since pes planus is usually associated with an unstable talocalcaneonavicular joint, hammer-toe deformities will frequently develop as a sign of flexor stabilization.
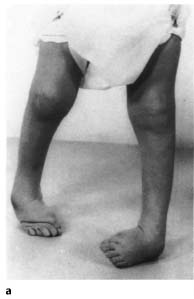
The deformity is often associated with a valgus hindfoot (pes planovalgus; Fig. 7.4). The small toes will be visible on the lateral margin of the foot because of the abduction of the forefoot. In contrast, the toes will not be visible next to the heel in a normal foot because of their axial alignment.
Pes Cavus
The generic term “pes cavus” refers to foot deformities with talipes equinus of the forefoot relative to the hindfoot. This significantly increases the height of the medial longitudinal arch. Pes cavus is more frequently associated with a varus deformity of the hindfoot than with a valgus deformity. Prominent calluses under the heads of the metatarsals indicate increased weight bearing in this area, while there will frequently be no calluses in the midsole, even on the lateral aspect. The talipes equinus deformity in the forefoot or metatarsus can often simulate superior displacement of the heel. Motion analysis will reveal decreased dorsiflexion. This is because the talocalcaneal complex is in dorsiflexion in the ankle to compensate for the pes cavus deformity in the tarsus.
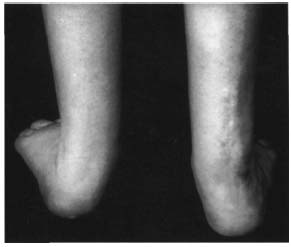
Fig. 7.4 Talipes valgus. The photograph shows a child with pes planovalgus. The valgus position of the hindfoot is conspicuous, as is the phenomenon of “too many toes” on the left side. The right foot has already undergone prior surgery.
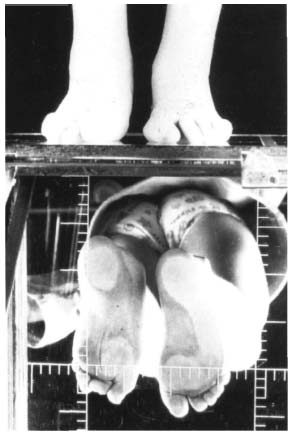
Fig. 7.5 Podometer view of pes cavus in a child with spina bifida and pes cavus in the left foot. The pedometer image shows the different patterns of weight bearing in the right and left feet. Weight distribution is nearly physiologic in the right foot, whereas in the left foot weight is borne solely by the heel and the medial ball of the foot. Secondary findings include hallux valgus in the left foot with a pronounced pronation deformity.
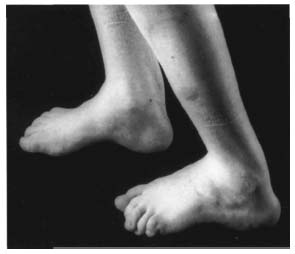
Fig. 7.6 Lateral view of pes cavus. The lateral view of Figure 7.5 demonstrates the pes cavus deformity.
The varus deformity of the hindfoot can be caused by fixed plantar flexion of the great toe because the supination of the forefoot forces the hindfoot into varus in the standing position. The standing-block test evaluates the flexibility of the varus deformity of the hindfoot. Place a block about 1.0-1.5 in thick under the lateral aspect of the foot. A flexible varus deformity of the hindfoot will straighten out as the lateral column is supported and the medial column hangs freely.
Hammer-toe deformities may develop because of the increased activity of the extensors (Figs. 7.5, 7.6).
Clubfoot
The term “clubfoot” describes a large complex of symptoms encompassing various types of deformities. The talus plays a key part in this deformity. Inspection will reveal superior displacement of the heel with a varus deformity of the hindfoot. A supination deformity of the metatarsus is present, and there is increased adduction of the forefoot.
Untreated clubfoot can be recognized by a typical callus pattern with increased callusing in the laterodorsal cuboid area. Hammer-toe deformities will also frequently develop with this deformity ; in contrast to pes cavus, these involve a flexion deformity.
A clubfoot deformity should be described according to the rigidity of its individual components and the degree to which these are correctable (Figs. 7.7a, b). To evaluate correction potential, grasp the heel between your middle and index fingers while pressing the cuboid with your thumb. This will move the foot into abduction and pronation. At the same time, try to correct the talipes equinus at the calcaneus.

Figs. 7.7a, b Infant with idiopathic clubfoot. The two photographs demonstrate the varus deformity of the hindfoot, talipes equinus component, and supination deformity.
Elasticity can be ascertained by applying moderate traction in the direction of correction.
Preliminary Examination of the Lower Extremity
Examination of the foot includes a preliminary examination of the lower extremity. Evaluate the range of motion in the hip and knee. Determine the angle of femoral anteversion with the patient supine. Evaluate for tibial torsion with the patient supine and the legs dangling from the examination table.
Determine differences in leg length using clinical methods or by radiographic examination.
Axial deviations such as coxa valga, coxa vara, genu valgum, or genu varum are determined by clinical or radiographic examination.
Instability of the knee involving cruciate or collateral ligament deficiency is also important when evaluating foot symptoms and planning appropriate therapy.
Palpation
Palpation is an important part of the clinical examination because complex deformities make it difficult to document many findings in diagnostic imaging studies. Symptoms involving nerves, tendons, joints, bursae, and vascular supply are also accessible to thorough palpation.
Examine the skin for trophic changes and possible infections. Lymphatic swelling can be distinguished from venous swelling since pressure applied to the dorsum of the foot will leave a temporary depression in venous engorgement. Examine vascular supply to the foot by palpating the dorsalis pedis artery slightly below the anterior aspect of the ankle between the extensor hallucis longus and extensor digitorum longus, and the posterior tibial artery directly posterior to the medial malleolus. Remember that the dorsalis pedis artery may be absent in 10% of the general population due to normal variants in vascular anatomy.
Palpating the posterior tibial artery may be difficult or impossible in patients with large amounts of adipose tissue in the ankles, or with an edema or synovial thickening posterior to the medial malleolus.
If palpation does not reveal the arteries, Doppler studies are indicated. Where signs of occlusive disease of the arteries is present, vascular supply to the lower extremities should be evaluated in Doppler ultrasound studies prior to any invasive procedure. Preoperative angiography is rarely indicated unless vascular surgery is indicated. The appropriate literature should be consulted for further information on vascular diagnostic methods.
The presence of a palpable pulse does not exclude small-vessel disease that occurs with diabetes or arthrosclerotic disease.
The tendons and peritendinous tissue are palpated to detect synovitis and painful degenerative or traumatic changes. The peroneal tendons can be distinguished from each other at the peroneal tubercle of the calcaneus. The peroneus brevis tendon courses superior to the tubercle and the peroneus longus inferior to it.
The flexor hallucis longus tendon can be readily palpated along its plantar course with the great toe in dorsiflexion (see also Fig. 7.24). Stenosing synovitis of the flexor hallucis longus tendon will cause symptoms near the posterior process of the talus.
The tibialis anterior and tibialis posterior tendons are best palpated during muscle strength tests.
Examine the Achilles tendon for thickening, swelling, and palpable defects.
Compression neuropathies of the foot can be divided into three groups:
– Superficial neuromas caused by repetitive trauma
– Interdigital neuromas (Morton neuroma)
– Tarsal tunnel syndrome
Compressive neuropathy syndromes require specific palpation according to the anatomy and symptoms. The examination should also include evaluation of the patient’s shoes for possible projections, edges, or ridges that may contribute to the compression neuropathy.
The nerves of the dorsum of the foot are particularly exposed, as are the sensory branches of the superficial peroneal nerve, the sural nerve, and the saphenous nerve at the Achilles tendon. Radiating tingling sensations can be elicited by palpating and tapping the nerves.
Interdigital neuromas usually occur between the heads of the third and fourth metatarsals and can simulate metatarsalgia. Applying dorsal and plantar compression with the thumb and index finger elicits characteristic pain and tingling.
Pain can occur along the course of the posterior tibial nerve where it branches into the tarsal tunnel or in the heel region. This pain can be identified by tapping about 1 cm dorsal and inferior of the medial malleolus. Accompanying tenosynovitis that presents as swelling posterior to the medial malleolus may also contribute to the compression syndrome.
Assessing Range of Motion
Instruct the patient to walk on tiptoe, on the heels, and on the medial and lateral borders of the feet. These maneuvers are a rough but effective way of assessing muscle strength in the foot and ankle and demonstrating the range of motion in the ankles and subtalar joints.
If the Achilles tendon is torn, the patient will be unable to walk on tiptoe. Subtalar injuries and symptoms will make walking on the medial borders, and to a greater degree the lateral border, of the feet difficult and painful.
An internally rotated gait may be due to internal tibial torsion or increased femoral anteversion. Normally, the toes and feet are dorsiflexed with each step. A “drop-foot” gait warrants further investigation. A patient simulating a disorder will often exhibit a drop foot or weak extensor hallucis, but then walk with normal dorsiflexion of the foot and toes.
Examine the foot independent of the gait cycle. The patient should sit on the examining table so that the popliteal fossa of each knee is in contact with the table and the feet dangle freely. Sit on a stool directly in front of the patient. Normally the foot will hang in slight plantar flexion and inversion. The spastic flat-foot will typically be involuntarily held in dorsiflexion and eversion.
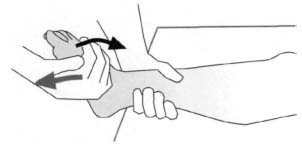
Fig. 7.8 Tibialis anterior test. To test the tibialis anterior, stabilize the calf above the ankle with one hand while exerting pressure in plantar flexion and eversion on the dorsum of the foot with the other hand.
Evaluate the strength of the dorsiflexors, plantar flexors, evertors, and inverters.
Acute tears of the tibialis posterior are rare. Tears in the tibialis anterior tendon can occur suddenly. Neither tendon can be palpated across the ankle. Injuries of the tibialis posterior tendon result in pes valgus and pes planus. The defect can be palpable across the medial navicular tubercle. Chronic degeneration changes in the posterior tibial tendon may have diffuse tenderness to palpation along its entire course.
Evaluation of the range of motion of the ankle, subtalar joint, and toes should take both age and individual variability into consideration.
Examining the Muscles
Tibialis anterior. The patient is seated with the knees flexed. If severe weakness is present, the patient may be placed in a lateral position. Immobilize the distal calf with one hand while exerting pressure in plantar flexion and eversion with the other hand on the dorsomedial aspect of the foot. Instruct the patient to invert the foot and dorsiflex it with the toes and the extensors of the great toe relaxed. It is crucial that the toe extensors be relaxed because they can supplement the tibialis anterior in dorsiflexion. The foot should be in inversion as opposed to a neutral position or eversion to eliminate the action of the extensors and peroneus tertius. A weak tibialis anterior is often accompanied by a talipes equinus deformity. The tibialis anterior can also be tested by having the patient walk on his or her heels with the feet inverted (Fig.7.8).
Tibialis posterior. The patient is in a lateral position lying on the affected side so that the lateral margin of the foot is in contact with the examining table. In the presence of severe weakness, the foot should dangle over the end of the examining table. Immobilize the distal calf with one hand while applying pressure to the medial side of the forefoot to move the foot into eversion and abduction and to move the ankle into dorsiflexion. Make sure the toes are in a neutral position and are not actively flexed to eliminate the action of the flexor hallucis longus (Fig. 7.9).

Fig. 7.9 Tibialis posterior test with muscle weakness. To test the tibialis posterior, have the patient supinate the foot from a lateral position.
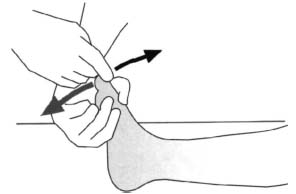
Fig. 7.10 Extensor hallucis longus test. To test the extensor hallucis longus, immobilize the tarsus and apply dorsal pressure to the distal phalanx of the great toe.
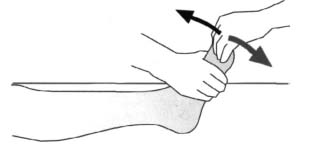
Fig. 7.11 Extensor digitorum longus test. To test the extensor digitorum longus, immobilize the tarsus and apply dorsolateral pressure to the distal small toes.
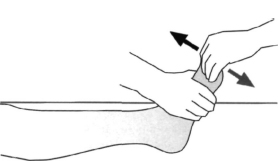
Fig. 7.12 Extensor digitorum brevis longus test. To test the extensor digitorum brevis, immobilize the tarsus and apply dorsolateral pressure to the proximal phalanges of the small toes.
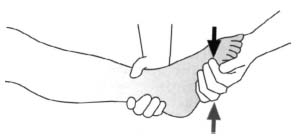
Fig. 7.13 Peroneus brevis longus test. To test the peroneus brevis, immobilize the calf slightly proximal to the ankle with one hand while pressing the lateral margin of the foot into adduction and inversion with the other hand.
Extensor hallucis longus. The patient is seated or supine on the examining table. A lateral position may be used for muscle weakness. Immobilize the tarsus with one hand so that the foot is in the neutral-0 position. Press the great toe on the distal phalanx into plantar flexion with the other hand. Now have the patient dorsiflex the great toe. It is difficult to separate the action of the extensor hallucis brevis from that of the extensor hallucis longus. In paralysis of the extensor hallucis longus, the extensor hallucis brevis will only be able to dorsiflex the proximal phalanx of the great toe. Aside from this, the great toe will be moved slightly toward the second toe (Fig. 7.10).
Extensor digitorum longus. The patient is seated or supine. Immobilize the forefoot in the neutral-0 position with one hand and apply pressure to the dorsum of the four lateral toes with the fingers of the other hand to move the toes into plantar flexion. Then have the patient extend the toes. If isolated muscle weakness is present, each toe can be tested individually (Fig. 7.11).
Extensor digitorum brevis and extensor hallucis brevis. The patient is seated or supine. Again, hold the metatarsus in a neutral position with one hand. Apply pressure to the proximal phalanges with the fingers of the other hand, moving them into plantar flexion against the patient’s resistance. Instruct the patient to extend the toes (Fig. 7.12).
Peroneus brevis. The patient is in a semi-lateral position on the contralateral side with the ankle in the neutral-0 position. Immobilize the distal calf with one hand proximal to the ankle while pressing the lateral margin of the foot into inversion with the other hand. Instruct the patient to evert the foot and the talocalcaneonavicular joint in a neutral position. Make sure that the long extensors are relaxed and the toes are held in slight flexion (Fig. 7.13).
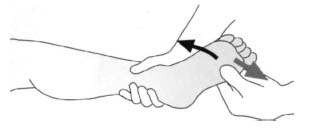
Fig. 7.14 Peroneus longus test. To test the peroneus longus, immobilize the calf slightly proximal to the ankle with one hand, and press the head of the first metatarsal into inversion and the ankle into dorsiflexion with the thumb and index finger.

Fig. 7.15 Gastrocnemius test II with normal muscle strength. To test the gastrocnemius, have the patient lift the heel off the floor into a tiptoe stance.
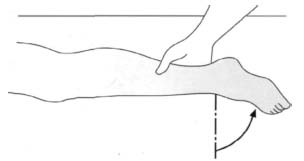
Fig. 7.16 Gastrocnemius test I with muscle weakness. Test the gastrocnemius with the patient supine and the knee extended. Have the patient move the ankle into plantar flexion.
Peroneus longus. The patient is in a semi-lateral position on the contralateral side. The ankle is in plantar flexion. Immobilize the distal calf proximal to the ankle with one hand. At the same time, press with the other hand against the head of the first metatarsal to elevate it, invert the foot, and move the ankle into dorsiflexion. Instruct the patient to evert the foot and bring the head of the first metatarsal into plantar flexion. Make sure that the toe extensors are relaxed for this maneuver (Fig. 7.14).
Triceps surae. This test is performed with the patient standing on one leg. Instruct the patient to stand on tiptoe without flexing the knee. The rest results are considered normal when the patient can successfully complete this maneuver ten times. Five successful maneuvers are considered good, one is satisfactory, and inability to achieve full plantar flexion is poor (Fig. 7.15).
With normal and poor results, repeat the test without weight bearing. Have the patient lie prone with the knee and ankle in the neutral-0 position. Immobilize the calf with one hand while pressing the posterior portion of the heel into dorsiflexion with the other. Now instruct the patient to move the foot into plantar flexion (Fig. 7.16). If the foot is not in the neutral-0 position but inverted, the tibialis posterior can contribute to the movement when the peroneal group is elongated. The same maneuver can be performed with the knee flexed 90° to test the soleus since the gastrocnemius components are relaxed in this position (Fig. 7.17).
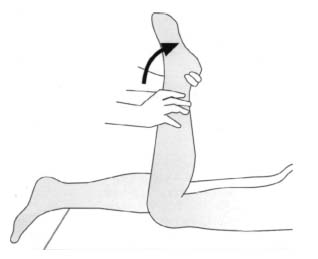
Fig. 7.17 Soleus test. To test the soleus, place the knee in flexion to eliminate the action of the gastrocnemius and have the patient move the ankle into plantar flexion.
The Silverskjöld test has proven effective in distinguishing the gastrocnemius and the soleus in talipes equinus deformities. The patient is supine. Grasp the heel to avoid any deviations in the valgus or varus alignment. If possible, bring the foot into 10°–20° dorsiflexion with the hip and knee flexed. This position eliminates the action of the gastrocnemius so extending the knee will produce an uncorrectable talipes equinus position. This is referred to as a positive gastrocnemius sign.
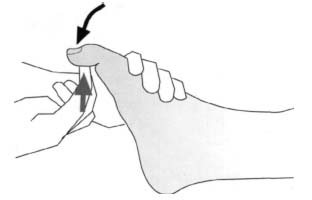
Fig. 7.18 Flexor hallucis longus test. To test the flexor hallucis longus, apply pressure to the distal phalanx of the great toe.
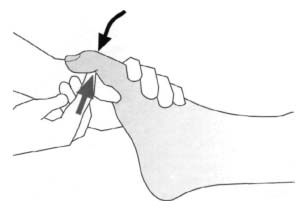
Fig. 7.19 Flexor hallucis brevis test. To test the flexor hallucis brevis, apply pressure to the proximal phalanx of the great toe.

Fig. 7.20 Flexor digitorum longus test. To test the flexor digitorum longus, apply pressure to the distal phalanges of the small toes.
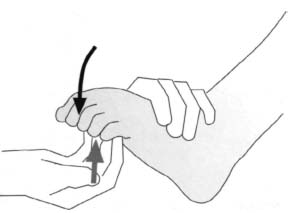
Fig. 7.21 Flexor digitorum brevis test. To test the flexor digitorum brevis, apply pressure to the proximal phalanges of the small toes.
Flexor hallucis longus. The patient is seated or supine. Stabilize the metatarsophalangeal joint with one hand. Hold the proximal phalanx of the great toe in a neutral position with the ankle in 30°–40° plantar flexion. Apply pressure to the distal interphalangeal joint with the other hand, moving it into dorsiflexion. Instruct the patient to flex the distal interphalangeal joint of the great toe. Make sure that the ankle is not completely dorsiflexed because the interphalangeal joint of the great toe flexes passively in dorsiflexion. On the other hand, complete plantar flexion weakens the muscle by moving its origin and insertion closer together (Fig. 7.18).
Flexor hallucis brevis. The patient is seated or supine. One hand stabilizes the head of the first metatarsal with the ankle held in plantar flexion to eliminate the action of the flexor hallucis longus. With the other hand, press against the plantar surface of the proximal phalanx of the great toe to dorsiflex it while instructing the patient to flex the toe (Fig. 7.19).
Flexor digitorum longus. The patient is seated or supine. One hand immobilizes the proximal and middle phalanges in a neutral position with the ankle in a neutral position. With the other hand, press against the plantar surface of the distal phalanges of the small toes to dorsiflex them while instructing the patient to flex the distal phalanges.
Because the two heads of the quadratus plantae insert into the lateral, dorsal, and plantar margin of the flexor digitorum tendon, it can contribute, to a certain extent, to flexion in the distal interphalangeal joint (Fig. 7.20).
Flexor digitorum brevis. The patient is supine. One hand immobilizes the proximal phalanges with the ankle flexed about 40°. With the other hand, press against the plantar aspect of the middle phalanges to move them into dorsiflexion while instructing the patient to flex the toes (Fig. 7.21).
Abductor hallucis. The patient is supine. Holding the foot in a neutral position with one hand, press the great toe toward the small toes with the other while instructing the patient to abduct the great toe.
Abductor digiti quinti. The patient is supine. Hold the forefoot in the neutral-0 position with one hand. Instruct the patient to abduct the small toe against your resistance as you press with the other hand against the lateral aspect of the small toe to move it into adduction. The dorsal interossei abduct the third and fourth toes. However, the average patient is unable to abduct the small toe.
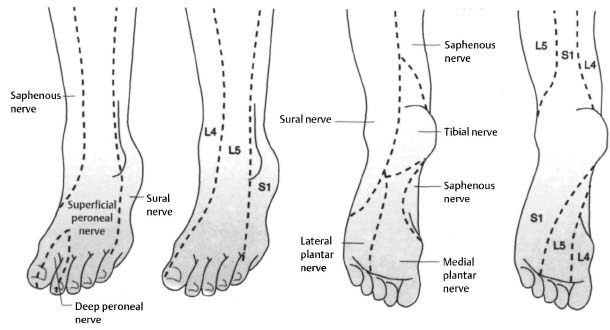
Fig. 7.22 Sensation in the foot.
Adductor hallucis and digitorum. The patient is seated or supine. Abduct the toes and press the great toe medially. Now have the patient move the great toe toward the small toes.
To evaluate the function of the plantar interrossei, hold the metatarsals of the third, fourth, and fifth toes in abduction. Instruct the patient to adduct against this resistance.
Lumbrical muscles. The anatomy of these muscles is highly variable in contrast to the lumbricals of the hand, and the muscles may even be missing. For this reason, they are not usually tested.
Neurologic Examination
Preliminary neurologic examination of the foot includes evaluation of the Achilles tendon, tibialis posterior, and patellar tendon reflexes, testing the Babinski reflex, and testing for atrophy in the intrinsic musculature of the foot (see p. 228). Sensation is tested on the lateral and medial margin of the foot and in the first and second web to evaluate the sensory supply of the deep peroneal nerve (Fig. 7.22).
If muscle weakness is present, it is evaluated and documented according to the degree of neurologic strength. Peripheral neuropathies such as are seen indiabetes, Charcot–Marie–Tooth disease, Friedreich’s ataxia, disorders of the spinal cord, tabes dorsalis, and other neurologic disorders are often initially identified in an examination of the foot.
Mild, undiagnosed cerebral palsy occasionally causes spastic flatfoot syndrome in one or both feet. In this case, the spasm can be associated with a positive Babinski reflex.
Specific Examination of Individual Regions of the Foot
Heel and Achilles Tendon
Examine the heel for varus or valgus deviation with the patient standing. Normally the heel will have a strong, uniformly rounded heel pad that may be atrophied in older patients, causing plantar heel pain.
Pain and sensitivity in the anterior portion of the medial tubercle of the calcaneus is a classic finding in heel spur syndrome. Pressure in this anatomic region can elicit pain (Fig. 7.23).
Less frequently, these symptoms may be located further posterior in the middle of the plantar aspect of the heel, particularly in association with heel pad atrophy.
Sensitivity in the plantar heel can occur in rheumatoid arthritis. Painful swelling of the heel pad may occur. Laboratory studies and other clinical signs of rheumatoid arthritis will confirm the diagnosis.
As has been mentioned, tenderness 2 cm distal to the medial calcaneal tubercle can be a sign of tenosynovitis of the flexor hallucis longus tendon. With the hallux in extreme passive dorsiflexion, the course of the tendon will be more readily palpable under the plantar fascia. The pain will be more superficial than in a heel spur syndrome and can be localized distally along the longitudinal arch (Fig. 7.24). In distance runners, one should consider plantar fascitis as the more probable caused of the discomfort (Fig. 7.25).

Fig. 7.23 Palpation of a heel spur.

Fig. 7.24 Palpation of the flexor hallucis longus tendon.

Fig. 7.25 Palpation of the plantar fascia.
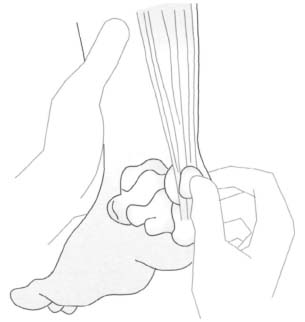
Fig. 7.26 Palpation of the Achilles tendon bursa.
Examine the Achilles tendon for shortening or elongation. A torn Achilles tendon, whether spontaneous or chronic, usually results in elongation. Significant pain will not necessarily be present, although the patient will usually be unable to stand on tiptoe. Soft swelling in the region of the Achilles tendon will confirm the diagnosis. In contrast, soft-tissue swelling in the bursa of the Achilles tendon usually suggests bursitis. This should be distinguished from synovial thickening of the posterior ankle (Fig. 7.26).
Subtalar Joint
Diagnosis and treatment of disorders of the subtalar joint are difficult and time-consuming. With injuries and diseases of the subtalar joint, the patient will frequently have a history of pain anterior and distal to the lateral malleolus. The range of motion of the talocalcaneonavicular joint should be evaluated in inversion and eversion according to the axis of motion. Grasp the heel with one hand and the forefoot with the other to evaluate range of motion. This grip technique is also used to evaluate the range of motion in the talocalcaneal joint and in the Chopart joint.

Fig. 7.27 Palpation of the tarsal sinus.
Normally, motion in the subtalar joint is uniform and painless.
Painless limitations of motion are usually encountered in older patients. Limited motion associated with pain may be a sign of a subtalar disorder. Often these limitations of motion are associated with tenderness to palpation over the tarsal sinus, inferior and anterior to the lateral malleolus (Fig. 7.27).
Subtalar symptoms can be cause by tarsal coalitions, rheumatoid arthritis, cerebral palsy, posttraumatic arthritis following fractures of the talus or calcaneus, Sudeck atrophy following ankle injuries, arthrofibrosis, prolonged immobilization in a plaster cast or traction through the calcaneus, and degenerative disorders in severe chronic pes pianovalgus. However, the cause of these disorders often remains unclear. Abnormal subtalar findings are frequently overlooked.
Longitudinal Arch
Often the longitudinal arch is flat in children but can reach normal height by puberty. The small cushion of fat above the longitudinal arch combined with the natural flexibility of the foot in children, which tends to flatten when bearing weight, will make the longitudinal arch appear flatter than it actually is.
Pes planus with normal subtalar mobility is a normal finding and does not require special shoes or inserts. On the other hand, pes planus can influence the normal subtalar mobility and biomechanics, and can be the presenting feature in a congenital vertical talus. Usually, further examination of pes planus in children is only necessary when range of motion is limited or other conditions such as poliomyelitis or cerebral palsy are present.
The lack test describes the rise in the longitudinal arch when the great toe is dorsiflexed in the presence of flexible pes planus.
Tarsals
One of the most common diseases of the tarsus is osteoarthritis, which is observed most frequently in older obese people. Involvement of one or more tarsal joints manifests itself as typical localized joint pain, tenderness to palpation, and possibly palpable osteophytes.
Charcot–Marie–Tooth disease of the foot usually begins in the tarsal region with palpable bone thickening. Pain is relatively slight in comparison to the palpable findings. Solid, rounded, and hard ganglia will occasionally be palpable in the tarsals and may be mistaken for bony exostoses. These ganglia typically increase or decrease in size and can be drained by aspiration. The aspirate will be the typical gelatinous fluid of a ganglion.
Metatarsals and Transverse Arch of the Foot
Metatarsalgia is a frequent foot symptom in women. Pain in the region of the metatarsal heads is usually described as burning. Generally there will be local pain directly under the heads of the metatarsals, usually at the second metatarsal.
Normally the anterior transverse arch describes a convex dorsal arc that flattens out with weight bearing. This occurs due to dorsoplantar play in the shafts of the first, fourth, and especially the fifth metatarsals. The second and third metatarsals are rigid in comparison. Plantar keratosis underthe second, third, and fourth metatarsal heads is usually pathologic.
In many cases, the anterior transverse arch describes a rigid dorsal concave arc, especially in splayfoot syndrome. This causes calluses under the second, third, and sometimes fourth metatarsal heads.
Any shortening of the metatarsal shaft, particularly of the first metatarsal, or dorsal displacement of the distal portion of the metatarsal increases the stress on the other metatarsal heads. Plantar flexed toes normally reduce the weight load on the metatarsal heads, whereas hammer toes increase the load. Pain under a metatarsal head adjacent to a healed metatarsal fracture or osteotomy is referred to as a transfer lesion.
Any cavus deformity, talipes equinus, or superior displacement of the heel increases the load on the metatarsal heads. Hallux valgus can produce increased callusing under the second metatarsal head due to the metatarsus varus.
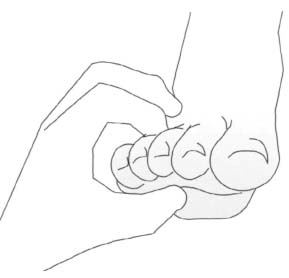
Fig. 7.28 Characteristic pain is elicited by compressing the interdigital space with the thumb and index finger in the presence of a Morton neuroma.
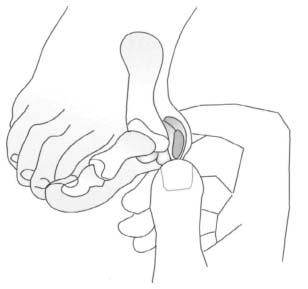
Fig. 7.29 Palpation of the bunion at the medial metatarsophalangeal joint in hallux valgus.
Plantar hyperkeratoses frequently develop in the region of the metatarsal heads as a sequela to scarring, superficial retention of foreign bodies, or plantar warts. They are often found in the vicinity of the metatarsal heads as opposed to directly beneath them. Sometimes plantar warts can simulate skin calluses but they can also rapid development of projecting calluses. Removing the hyperkeratosis exposes the plantar wart beneath it, which can be multilocular. One identifying characteristic of plantar warts is that direct pressure will only cause slight pain, while indirect compression can cause acute pain.
Painful rubbery edema on the dorsal aspect of a metatarsal is frequently a sign of a stress fracture.
Another clinical syndrome encountered in the forefoot is Morton neuroma, usually seen between the third and fourth interdigital space. Pain will typically occur when the metatarsal heads are subjected to transverse compression and during simultaneous dorsal and plantar palpation of the interdigital spaces with the thumb and index finger. Patients will feel tingling pain (Fig. 7.28). Injection of local anesthetic through the intermetatarsal ligament can confirm the diagnosis by anesthetizing this neuroma.
Great Toe
Disorders that involve the great toe include ingrown toenails, hallux valgus, hallux rigidus, and bursitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








