The Flexible Adult Flatfoot
Anatomy and Pathomechanics
Jeremy L. Walters, DPM∗JeremyLWalters@gmail.com and Samuel S. Mendicino, DPM, West Houston Medical and Surgical Residency Program PMSR/RRA, West Houston Medical Center, 12121 Richmond Avenue, Suite 417, Houston, TX 77082, USA
Adult acquired flatfoot deformity is generally associated with a collapsing medial longitudinal arch and progressive loss of strength of the tibialis posterior tendon. It is most commonly associated with posterior tibial tendon dysfunction that can have an arthritic or traumatic cause. With an increasing population of obese patients, the often misdiagnosed and overlooked posterior tibial tendon dysfunction will only continue to present more often in the foot and ankle specialist’s office. This article focuses on the anatomy, classification, and pathomechanics of the flexible adult flatfoot.
Classification
Johnson and Strom
Many classification systems have been described in the literature formulated from clinical findings, radiographic findings, and/or etiology of the pathology. In 1989, Johnson and Strom1 introduced a classification system that was intended to correlate the presentation, physical findings, and radiographic findings that would ultimately guide surgical intervention and still remains the most widely used.
Stage 1, tenosynovitis is predominant. There is an absence of hindfoot valgus, too many toes, and patients are generally able to perform a single heel raise. Tendon length is preserved and patients elicit pain with direct palpation of the tendon distal to the medial malleolus.
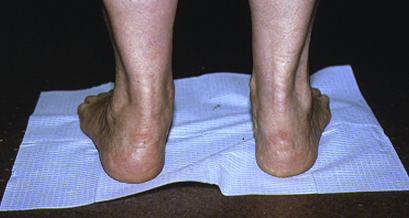
Stage 2 is typically when the first sign of deformity presents. The tendon has developed degeneration and elongation and a hindfoot valgus is appreciated with possible forefoot abduction (Fig. 1). Patients may be able to perform a single heel raise in this stage but as the dysfunction progresses the ability is lost (Fig. 2). It is important to remember that in this stage, the deformity remains flexible. A trend in recent years has been to subdivide this category into “A” and “B,” where the “A” group represents patients with medial pain and the ability to perform a single heel raise. “B” group patients have fibular impingement pain and incompetence of the PTT.
Stage 3 is for the patient that has developed a rigid deformity. The examiner is unable to correct the forefoot abduction or hindfoot valgus on examination, patients typically complain of only lateral pain, and patients are unable to perform single heel raise.
Stage 4 is reserved for the patient that progresses to ankle joint involvement. The dysfunction leads to a valgus talus and eventually attenuation of the deltoid ligament. The once subfibular impingement pain is now pain generally related to ankle arthritis.
Anatomy
PTT
The PTT has origins on the posterior aspect of the tibia, fibula, and interosseous membrane. It was Morimoto2 in 1983 that suggested the fibular origin is the strongest and evolutionarily newer than the tibial side. It is the more lateral origin of the muscle that improves the lever arm and provides greater inversion of the foot. The tendon crosses the medial aspect of the posterior talus, the medial aspect of the talar neck, and the inferior surface of the inferocalcaneonavicular ligament and is located above the sustentaculum tali.3 According to Bloome and colleagues,4 just in front of the navicular tuberosity the PTT splits into three bands: (1) anterior, (2) middle, and (3) posterior. The anterior band is the largest and a direct continuation of the tendon that inserts into the navicular tuberosity, the inferior surface of the navicular-cuneiform joint, and the plantar aspect of the first metatarsal cuneiform joint. The middle component is a very deep band that continues distally into the sole of the foot and inserts into the cuneiforms and cuboid. The posterior component originates before tendon insertion on the tuberosity and courses laterally, inserting onto the anterior aspect of the sustentaculum tali. The width of the tendinous bands as a percentage of the whole is anterior 65%, middle band 15%, and posterior band 20%.3,4 The importance of this tendon cannot be overlooked; Jahss5 noted the normal inversion strength of the calf muscles to be 12 to 15 pounds of torque. With a rupture of the PTT, the torque of the calf muscles decreases to 3 to 6 pounds of torque.
The vascular supply to the PTT remains a controversial topic. The posterior tibial artery is the primary blood supply to the tendon, although Sarrafian3 reports the insertion might receive its blood supply from branches off the dorsalis pedis artery. In 28 cadaveric specimens, Frey and colleagues6 identified a hypovascular zone 40 mm proximal to the PTT insertion that begins at the level of the medial malleolus and, interestingly, there was no mesotenon present at this level. In the study control, the flexor digitorum longus tendon, no such zone existed and a consistent vascularity was noted. Peterson and colleagues7 attempted to replicate the study using a different technique and found an avascular zone rather than a hypovascular zone at the level of the medial malleolus. A third theory proposed by Mosier and colleagues8 stated the PTT actually contained neovasculization of the tendon in the degenerative region caused by the increase in mucin and myxoid degeneration and attributed the degeneration to a collagen disorder in place of a vascular cause of the PTT degeneration.
Plantar Calcaneonavicular Ligament
First known as the ligamentum neglectum and as part of the tibiocalcaneonavicular ligament, the plantar calcaneonavicular ligament was later determined by Lane9 to be a separate ligament. The plantar calcaneonavicular is typically described as consisting of two bundles, superomedial and inferior. Many anatomic descriptions exist in the literature; Sarrafian and colleagues3 and Davis and colleagues10 have each offered their own descriptions but it has generally been accepted that the superomedial bundle is subject to stress at the level of the TNJ and as a result is covered dorsally by fibrocartilage, thus making it the strongest and broadest of the two bundles that form the acetabulum pedis.11 The superomedial bundle is triangular and shaped like a hammock. The ligament originates from the middle facet and sustentaculum tali of the subtalar joint and inserts onto the navicular tuberosity and the superior aspect of the medial side of the navicular articular margin. The inferoplantar bundle is a short and broad ligament. The origin is classically described as between the anterior and middle articular facets of the subtalar joint and inserting into navicular beak laterally. Histologically, there appears to be an absence of elastic fibers within the complex,12,13 thus possibly making reference to the plantar calcaneonavicular ligament as the spring ligament to be inaccurate because no elastic properties exist within it. The dorsal and central third of the superomedial bundle is avascular with the calcaneal branches of the medial plantar artery supplying the proximal aspect of the ligament and the distal third receiving its vascular supply from the navicular branches of the medial plantar artery.10 The ligament complex serves as static support for the head of the talus, provides support to the TNJ, and provides medial longitudinal arch support.14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree