Fig. 9.1
Image of electrical burn to left hand immediately following debridement of nonviable tissue and escharotomy on the day of injury
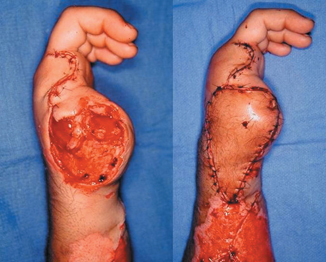
Fig. 9.2
Post injury day five following amputation of nonviable thumb and index finger with microvascular free tissue transfer for wound coverage

Fig. 9.3
3 months post injury demonstrating excellent wound healing

Fig. 9.4
Immediate postoperative images following transfer of second toe for thumb reconstruction
Chemical Burns
According to the American Burn Association National Burn Repository (2013 report), chemical burns account for 3 % of admissions to burn centers [21]. Chemicals cause from 2 to 11 % of all burns and contribute to as many as 30 % of burn-related deaths [22]. Improper handling of materials and/or use of exposure protection clothing in both the industrial workplace and residential environment are associated with these injuries. The hand and fingers are particularly at risk when proper protection is not employed. One review showed that the hands and upper extremities are the most frequently injured areas from chemical burns exceeding all other sites combined [23]. Fingertips are at no greater risk than the hand in general to chemical injury. However, as in other burns, chemical burns of the fingertips may result in a longer functional recovery due to the interference with tactile sensation and prehension.
The ability of a chemical to produce a burn injury is dependent on its concentration, amount exposed to the tissue, and the duration of contact. Chemical burns can be caused by numerous substances most of which are a strong base, a strong acid, or a halogenated hydrocarbon. Prolonged exposure to less noxious substances can also lead to a significant chemical burn. All chemicals capable of producing a burn do so by specific chemical reactions with tissue. In general, exposure to acids results in coagulation necrosis of the tissue while alkalis produce tissue liquefaction. Other chemicals are vesicants that result in necrosis from ischemia due to release of inflammatory mediators. The burn injury from exposure to a chemical continues until it is washed off, neutralized, or exhausted by the interaction with tissues [24]. For the majority of chemical burns, immediate and continuous water irrigation is the most critical initial treatment. The hands and fingers can easily be positioned under a water tap. The continuous flow of water not only dilutes the chemical but also dissipates any heat from a chemical reaction. Studies have shown that chemical burns not receiving irrigation within 10 min of exposure have a greater incidence of full-thickness injury. The only exception to water irrigation is exposure to elemental sodium, potassium, or lithium which will ignite with exposure to water [25].
Acid Burns
The appearance of an acid burn ranges from mild erythema of a superficial injury to the leathery appearance of a full-thickness skin loss. Acid burns are typically severely painful. As noted above, the most important step to mitigate injury is to begin copious irrigation of the affected part within 10 min of exposure. Additionally, a dilute solution of sodium bicarbonate may be used with the irrigation. After irrigation, the wounds are treated similarly to other burn wounds [24].
Hydrofluoric (HF) acid is an inorganic acid with multiple uses in industry. This acid is highly corrosive, injuring tissue by two different mechanisms. First, the high hydrogen ion concentration typical for all acid burns erodes the cutaneous barrier. Second, soluble free fluoride ions penetrate the damaged skin barrier causing liquefaction necrosis of the soft tissue, desiccation of the wound, and if deep enough will erode the bone. The free fluoride ion binds with intracellular calcium and magnesium producing cell death with rerelease of the fluoride ion. Death has been reported from exposure of 1 % of total body surface area to HF acid, secondary to a rapid and severe hypocalcemia. Cutaneous exposure to a dilute concentration of HF acid may have delayed onset of symptoms but will ultimately produce tissue necrosis with severe pain. A more concentrated solution may produce a painful lesion with a minimal apparent initial injury. Once a HF acid exposure is diagnosed, treatment must be initiated early. Prompt irrigation with water is the first modality. Fingernails should be trimmed to remove the possibility of acid being trapped beneath them. The next line of treatment is aimed at binding the free fluoride ions. Application of calcium gluconate burn gel is the only effective topical agent for HF acid burns. Massaging the gel into more superficial exposures will mitigate the pain of the burn as well as progression of the injury. Injection of a 10 % calcium gluconate solution into the affected area is the most often used method to stop the progression of injury, mitigate pain, and prevent systemic fluoride toxicity. Small-volume injections are given using a 30-gauge needle. Pain relief is dramatic and guides both the number of injections and need for repeat treatment. Injection into pulp spaces of the fingertips should be done cautiously to avoid vascular embarrassment from pressure in a closed space. For more extensive HF acid burns of the hands, intra-arterial calcium gluconate infusion can be used. Pain relief is usually quite rapid and the infusion stops systemic effect of HF acid burns. Injections of calcium gluconate are also avoided [24, 26] .
Alkali Burns
In addition to being used in industrial settings, alkali chemicals are prevalent in the residential setting, being an ingredient in drain cleaners, oven cleaners, fertilizers, and cement products. In general, alkali exposures have less immediately apparent tissue damage but ultimately result in a deeper injury. The high pH of alkalis results in saponification of tissue fats resulting in necrosis. Alkali molecules are then available to produce the damage to deeper tissues. The pH change in tissue associated with an alkali injury is more dramatic and prolonged than seen with acid burns and requires longer irrigation (an hour or more) to mitigate injury.
Cement burns are common, particularly in individuals not familiar with the caustic quality of wet cement. “Do-it-yourselfers” are more prone to handle wet cement without appropriate skin protection, particularly impermeable gloves. Wet cement has a pH greater than 12 and is capable of producing a full-thickness alkali burn. Symptoms may not appear for several hours after exposure. Erythema, pain, and a burning sensation ultimately appear. Prolonged irrigation is the early treatment modality. Mild exposures will lead to superficial desquamation (particularly glabrous skin) followed by a period of skin hypersensitivity until normal epidermal thickness is achieved. More severe exposures can result in full-thickness skin loss [24, 27].
Gasoline/Hydrocarbons
Gasoline, hydrocarbons, and solvents primarily irritate skin but prolonged exposure may result in a cutaneous burn. Treatment is removal of the compound from skin contact and prolonged irrigation. Topical treatment of the resultant cutaneous injury is similar to that of thermal injuries [25].
Phosphorus Burns
While more commonly associated with injury from munitions explosion exposure in military personnel, white phosphorus burns can occur in the civilian sector from exposure to fireworks, insecticides, and fertilizers. Phosphorus ignites with exposure to air and is controlled by wetting. However, re-drying results in the exothermic oxidation of the phosphorus. Until definitive treatment can be delivered, the affected area should be covered with mineral oil to prevent exposure to air. Treatment requires both irrigation of the affected skin and removal of the phosphorus particles. The latter is facilitated by the use of a Wood’s lamp. Alternatively, the affected area may be washed with a 1 % copper sulfate solution that results in black cupric phosphate particles that are more visible. The copper sulfate solution must be washed off to prevent copper toxicity [25].
Cold Injuries
Much of our knowledge of and appreciation for cold injuries is from military experiences in harsh weather environments dating back to the Spartan times and through World War II. Now, these injuries are more frequently seen in nonmilitary populations, specifically those without resources or mental capacity to seek refuge in cold temperatures. Intoxication also plays an important role in cold injuries as the body’s shivering response to keep warm may be blunted and cutaneous vasodilation may result in cold injuries at relatively warmer temperatures. In response to the cold exposure, the body directs blood away from the skin and away from the extremities. This leaves the skin and subcutaneous tissues, particularly of the distal extremities, vulnerable to freezing. Any other factors or conditions that reduce circulation, including cigarette smoking and peripheral vascular disease can increase the effects of cold injury. Hand and feet injuries account for 90 % of the reported episodes of frostbite [28–30].
The presence of wind can accelerate the effect of cold weather. An increase in wind speed from 10 to 20 mph at 0 °F can reduce the time of freeze injuries in exposed skin from 60 to 30 min. A windchill temperature of − 40 °F can lead to a freeze injury of exposed skin in minutes. The extent of the injury is more closely related to the duration of cold exposure, rather than the temperature itself. Cold injuries exist within a spectrum of severity based on the rate of cooling and the presence of ice crystals in the tissues. Frostbite is the result of slow rate of cooling which leads to the formation of ice crystals. These are potentially reversible injuries [31].
There are two potential phases of cellular death in frostbite injuries . The first occurs during the freezing when ice crystals change the osmotic gradient in the tissues resulting in water being drawn out of the cells. This alters the cell’s stability and function. Additionally, capillary blood flow is diminished as the blood viscosity increases and this results in hypoperfusion and hypoxia. Fortunately, the diminished metabolic activity of the tissue in response to the cold temperature may have some protective function for the cells such that the cells may survive the freezing phase. However, when the freezing occurs rapidly intracellular and extracellular ice crystals can cause immediate cell lysis and death. The second phase of the injury occurs during the tissue rewarming. Once the person has been removed from the cold environment, vasospasm lessens and limb perfusion increases. However, the effects of the cold exposure have damaged the microcirculation vasculature and intravascular thrombosis can occur. Prostaglandin and thromboxane are released during this course of freezing and thawing can potentiate vasoconstriction, platelet aggregation, and thrombosis. This process can result in further tissue ischemia in an apparently well-perfused limb with good pulses. Rapid rewarming can lessen this phase of the injury. As tissue reperfusion progresses, blisters form in the skin. Hemorrhagic blisters suggest significant injury to the dermal arterial supply and carry a poor prognosis. Additionally, skin that does not show blistering after rewarming suggests poor blood flow and also carries a poor prognosis. It is important to be aware that as the vasospasm to the cold limb is diminished during the rewarming phase, cold venous blood from the extremities is returned to the chest and can lower the body’s core temperature [3, 32].
Clinically frostbite injuries are graded in terms of severity. First-degree frostbite is a superficial injury that is manifested by hyperemia and no blister formation on rewarming. Sensation is generally preserved and tissue loss is unlikely. Second-degree frostbite injury is a more severe superficial injury. Nonhemorrhagic blistering occurs with potentially significant swelling. Wound care to the ruptured blisters can prevent infection and tissue loss. Third-degree frostbite involves some of the deeper tissues. Hemorrhagic blisters can occur in the deeper dermal layers. The skin is initially insensate but can progress to long-term paresthesias and neuropathic pain. Fourth-degree frostbite involves deeper tissue like bone and muscle. There is no reperfusion of the damaged tissue during rewarming. The involved digits will mummify and require amputation. Classification of these injuries may not be possible acutely. An involved extremity or digit may have multiple degrees of frostbite simultaneously with higher degrees of severity present more distally [3, 32].
Treatment of patients with frostbite injuries includes rapid rewarming in water baths of 104–108 °F. This process can be quite painful and narcotic medications are often necessary. Affected body parts can develop significant edema. Splinting, elevation, and range-of-motion exercises can be effective in reducing the swelling. Patients should receive tetanus prophylaxis if they have not received a booster within 5 years. Nonsteroidal anti-inflammatory medications can augment pain relief and also help with wound healing by diminishing prostaglandin synthesis and the potentially cytotoxic inflammatory response to rewarming, and by preventing the microvascular thrombosis from occurring. Topical aloe vera applied to the wounds has also been shown to improve healing. There is debate regarding the role of blister debridement or blister aspiration to remove the high concentrations of toxic metabolites that have been found in blister fluid that have been shown to potentiate an inflammatory response and dermal ischemia. There is some evidence that administration of tissue plasminogen activator (tPA) during the rewarming phase can reduce the incidence of amputation. Bruen et al. demonstrated that patients with abnormal digital perfusion as seen on digital angiography experienced a reduction in the incidence of digital amputation from 41 to 10 % when tPA was administered following frostbite injury [32, 33].
Hyperbaric oxygen (HBO) therapy for the treatment of frostbite injuries has been reported in several cases, dating back to 1963, with good anecdotal results. HBO increases local tissue oxygen tension and can increase the revascularization and viability of damaged tissue. Favorable results have been reported even when initiating this treatment 2 weeks or more after injury. It has been proposed to initiate this treatment early, during the rewarming phase, to minimize the reperfusion component of the injury. Currently, HBO treatment for frostbite injuries is considered investigational in the USA [34].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








