Fig. 5.1
a, b, c Fingertip arterial, venous, and nerve anatomy by Tamai and Ishikawa zones (with permission by Alexander B. Dagum)
Surgical Anatomy
A thorough knowledge of the vascular anatomy of the fingertip is necessary for successful fingertip replantation . The arterial anatomy is relatively constant and has been well described in the classic paper by Strauch and de Moura and others [17–19]. The ulnar digital artery is dominant in the thumb, index, and long fingers and the radial digital artery is dominant in the ring and small fingers. The ulnar and radial arteries are connected by three transverse palmar arches in the finger: two Gothic-like (pointed) arches at the level of the C1 and C3 cruciate pulleys and a rounded (Romanesque) arch just distal to the insertion of the flexor digitorum profundus (FDP) tendon . At the level of the distal transverse palmar arch (DTPA), the digital arteries measure 0.85 ± 0.1 mm in diameter. There are approximately three or more arteries that takeoff from the distal arch measuring 0.58 ± 0.1 mm with the center one being dominant and known as the terminal central artery (Fig. 5.1). These terminal arteries are in close proximity to the periosteum, travel longitudinally before turning dorsally, and communicate with the distal matrix arch. There is some tortuosity to these distal pulp arteries which allows for some extra length to be gained with dissection [19, 20].
The venous anatomy is more variable and consists of a dorsal and palmar system [21, 22] (Fig. 5.1). The dorsal system is dominant and commences in the paronychial area as one or two venules on each side of the nail fold measuring approximately 0.2 mm distally and 0.4 mm proximally. They unite at the level of the nail bed in the middle forming a central vein known as the dorsal terminal vein measuring (0.5–0.8 mm). This dorsal vein increases slightly in size before dividing into two or three veins at the level of the DIPJ.
The palmar venous network commences at the tip and forms multiple anastomosing veins in the subcutaneous tissue with no consistent pattern. They converge at the level of the base of the distal phalanx into one to three veins, with the central vein measuring 0.4–0.6 mm in diameter and lateral veins 0.3–0.5 mm in diameter. The palmar and dorsal systems are connected by the lateral commissural veins which measure 0.5–0.8 mm at the level of the DIPJ.
The digital nerve trifurcates 60 % of the time just distal to the DIPJ crease in 78 % of digit [23]. There may be anywhere from two to five branches in the digits and as many as seven in the thumb [23]. In the thumb, they consist of the proximal dorsal, distal medial, and lateral ungal branches [24]. There is an extensive crossover distal to this of the territory supplied by each nerve branch.
Indications and Contraindications
The decision to replant a part should be made at a replantation center . A careful evaluation of the patient and the part needs to be made. The patient needs to be aware of the limitations of replantation surgery. In patients with serious life-threatening conditions or illnesses, replantation is contraindicated [1, 2]. In fingertip amputations , the part needs to be evaluated with the operating microscope as surgical loop magnification is usually insufficient to assess the vessels.
In general, fingertip replantation is indicated in all children because of their great regenerative potential, in musicians or patients in whom digital length is very important for their employment or hobbies, or where esthetic concerns are paramount. Replantation is contraindicated in crush avulsion injuries where there has been significant soft tissue injury or contamination or injury at multiple levels. Nevertheless, the part should be scrutinized for their salvage potential and the spare part’s concept used. A nonmicrovascular replantable distal fingertip amputation can sometimes be reattached as a composite graft after appropriate debridement, yielding a reasonable result (Fig. 5.2). The results of composite fingertip grafts , Tamai zone I for adults, are in the order of 20 versus 50 % for children and depend on various factors [25–27]. Several techniques have been proposed to improve survival of composite grafts including hyperbaric oxygen, cooling, and the pocket principle.


Fig. 5.2
Fifty-one-year-old male with a Tamai zone II fingertip amputation. a The part consisted of skin, pulp germinal matrix, and sterile matrix and contained a small amount of tuft distally. No suitable vessels were available for arterial anastomosis as it was superficial to the digital artery and terminal arteries. b, c The part was carefully debrided and the small piece of tuft removed and then the remaining part was reattached as a composite graft. d Three months post injury, showing a healed composite graft with a new nail growing in
In the pocket method, the part is de-epithelialized, reattached, and then buried into a subcutaneous pocket in the abdomen, axilla, chest, and more recently the palm. This increases the surface area contact and thus blood supply. At 2–3 weeks, the part is detached from the pocket and allows to re-epithelialize over a 3-week period or a thin split thickness skin graft applied. The pocket principle has not gained widespread acceptance despite being first described by Brent in 1979, and subsequently modified by several authors with reported success rates from 14 to 90 %. It would appear to be best suited for nonreplantable fingertip amputations distal to the lunula [28–31].
Care of the Amputation Part and Patient
Appropriate care of the amputated part is extremely important. Cooling of the part to 4 °C lowers the metabolic rate and doubles the allowable ischemia time. The part should be gently cleaned with saline, then wrapped in saline-soaked gauze and placed in a bag and into a container consisting of ice slurry, which will be at approximately 4 °C. The part can also be placed in a container of saline, which is then placed in an ice bucket. The part must not rest on pure ice because this can lead to a frostbite injury making the part no longer replantable. Although there have been isolated reports of longer ischemia times with successful outcomes, in general, digits will tolerate 12 h of warm ischemia and up to 24 h of cold ischemia time [1, 2, 32].
The overall management of the patient takes precedence. This mandates a thorough history and physical examination. The tetanus status should be checked and given as per protocol if needed. Antibiotics are given. This usually consists of cefazolin except in farm injuries for which Gram-negative coverage with gentamicin is usually added. The appropriate laboratory workup is performed and radiographs of the part and amputation stump are obtained. An axillary block is used to provide for pain relief and vasodilation.
The part is carefully assessed for the type and extent of injury, presence of a second level of injury, and contamination. Red streaks or bruising along the skin in the course of the digital arteries, the so-called Chinese red lines, represent the tearing of the small side branches of the digital arteries and signify extensive digital vessel injury. If the digital artery is elongated, twisted, and curled up like a pigtail (the ribbon sign), this signifies extensive intimal damage to the vessel. Both of these signs usually preclude successful replantation unless the zone of injury can be bypassed with a vein graft.
Technique
The use of two teams is optimal when multiple fingertips/digits have been amputated. One team works on the amputated part and the other on the amputation stumps . In isolated fingertip amputations, one team suffices, as in general the part can be assessed and prepared in under an hour. This in general is less than the time it takes to prepare the patient and bring him from the emergency room to the operating room. At our institution, we have performed fingertip replantations under local anesthesia with IV sedation, regional anesthesia, and general anesthesia.
The part is carefully assessed for its replant potential. In fingertip amputations, a significant crush or avulsion component will usually preclude successful replantation , as once one is out of the zone injury, very little fingertip will be left to work with. A clean-cut injury with at most a limited crush component will yield best results.
Ishikawa subzone I amputations, i.e., distal to the midpoint of the nail, are extremely challenging, but good reconstructive options are available for fingernail preservation such as composite graft, V–Y advancement flaps, etc. Subzone II amputations from the nail base to midpoint of the nail are very challenging as well, but reconstructive options diminish as the injury proceeds proximally (Fig. 5.3). A similar approach is used in Ishikawa subzones I and II or Tamai zone I injuries. The part is examined for its replant potential under the microscope. The part can be stabilized by suturing the nail plate to a suture package; the suture package can then be held by an assistant [33]. We have modified this technique and held the suture package with a lead hand, thus freeing up the assistant. A search for the terminal central artery which runs close to the midline just superficial to the periosteum is carried out in both the part and the stump by gently dissecting and elevating the soft tissue. The stump is assessed for any area of pulsation which, if seen, will indicate the location of the proximal artery . Matching the part to the stump can then facilitate locating the terminal artery if one is having difficulties. Although, in general, the distal artery is very consistent in its location and not difficult to find, the central artery has a certain amount of tortuosity which provides for added length when dissected distally [19, 20]. Occasionally, at subzone II, a palmar vein of suitable quality or lateral commissural vein will be found. Pressure on the pulp will sometimes lead to a small venous ooze facilitating the location of the vein. In the author’s experience, a suitable vein is often not found at these levels and the strategies delineated below will need to be applied for venous drainage. The vascular structures are tagged with 10–0 nylon. A 028 K-wire or just sutures are used to secure the part. A dorsal-to-volar sequence of repair is used. Care is taken to repair the sterile matrix with 6–0 chromic gut. It is not always feasible or necessary to apply a microvascular clamp. The repair starts with the back wall first as one may not be able to easily flip the vessel. A small nylon suture can be used to stent the vessel and facilitate repair [34]. The anastomoses are performed with four to five 11–0 nylon sutures around the vessel wall; care is taken during the anastomosis as the vessel walls are thin and can easily tear. No nerve anastomosis is performed at this level, as the branches will have arborized with no suitable size branch available for repair. Nevertheless, good sensory recovery occurs at this level probably through spontaneous neurotization from the multiple branches [12].
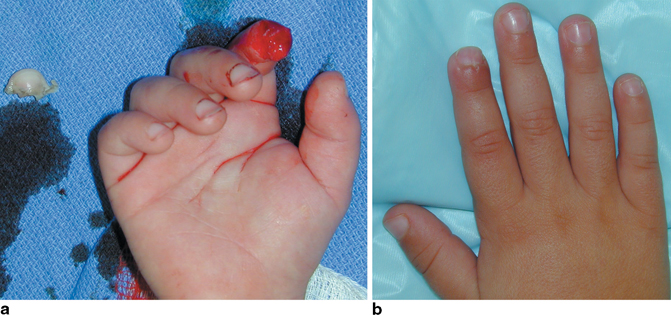
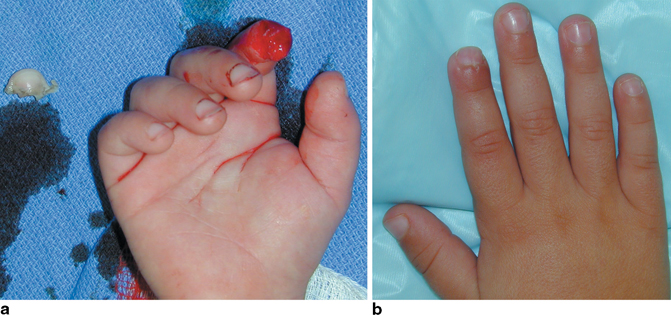
Fig. 5.3
a A child sustained a Tamai zone I, Ishikawa subzone II fingertip amputation. b Three months post replantation, showing some mild pulp atrophy, but otherwise a good result
Tamai zone II or Ishikawa subzones III and IV are amputations between the DIPJ and nail base (Figs. 5.4, 5.5 and 5.6). At these levels, no good option exists for fingertip and nail reconstruction, but the vessels are larger and replantation easier. Adequate debridement is performed with appropriate bone shortening (Fig. 5.4). If the repair is through the germinal matrix, meticulous repair is essential to avoid late fingernail deformities. Injuries through the DIPJ level or in very close proximity are arthrodesed (Figs. 5.5 and 5.6). One or two K-wires are used for bony osteosynthesis, occasionally a circlage wire with one K-wire is used for more proximal injuries. The FDP tendon, if lacerated, is repaired if adequate distal tendon is available for repair. At the level of the DIPJ, curvilinear midlateral incisions both in the part and in the stump are adequate to expose the distal digital vessels, digital nerve branches, and dorsal veins. Distal to the DIPJ, a thin oblique flap is preferred for exposure of the vessels as described by Tsai et al. [35]. The oblique flap is made very thin to avoid injuring the palmar veins in case these are necessary for venous anastomosis. It is important to keep in mind that in the fingers the DTPA was found on average at 13.7 mm from tip or at the level of germinal matrix [19]. In a distal subzone III amputation, the repair will be at the level of the distal digital artery as it is forming the arch. Attention is then turned to isolating the terminal dorsal vein which is found along the dorsal midline from the DIPJ to the level of the germinal matrix [21]. Usually, one large vein, a few millimeters proximal to the nail fold, greater than 5 mm distally and more often 8 mm proximally will be found. We also look laterally and search for a lateral commissural vein and palmar for palmar veins. All structures are tagged with 10–0 nylon. In proximal subzone III and subzone IV, we look laterally to isolate a nerve branch for repair. Usually, one nerve branch is found without too much effort radially and ulnarly and tagged. At these more proximal levels, repair of one branch will lead to good sensory recovery and is better than no repair in the author’s experience.
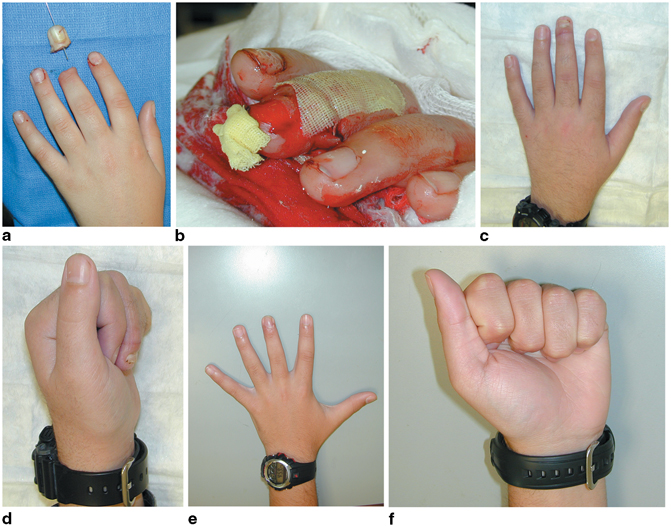
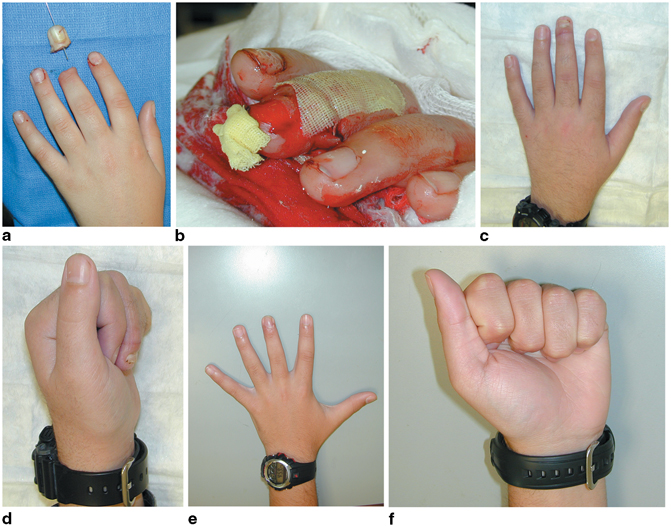
Fig. 5.4
a, b Fourteen-year-old boy with a clean-cut Ishikawa Sub-zone III fingertip amputation through the growth plate from a zip line. c, d Three months later and e, f 5 years post operation, the digit was slightly shorter than the contralateral side from premature closure of the growth plate; he recovered normal two-point discrimination and 30° of DIPJ motion. (From: [2]. Used with permission from Alexander B. Dagum and The American Society for Surgery of the Hand). DIPJ distal interphalangeal joint
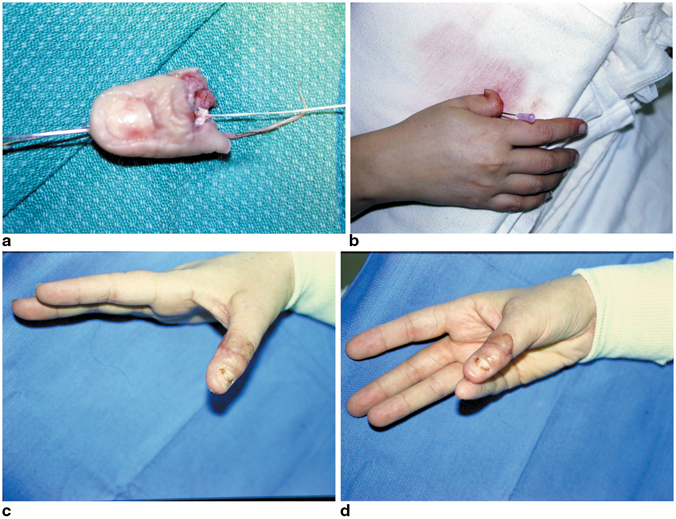
Fig. 5.5




a, b A watch jeweler sustained a thumb avulsion injury at the IPJ level Tamai zone II from a rein on a horse that was spooked. c, d Replantation was successful in restoring good hand function and 12 mm of two-point discrimination. However, the sensation was not good enough for her to return to her prior occupation. (From: [2]. Used with permission from Alexander B. Dagum and The American Society for Surgery of the Hand). IPJ interphalangeal joint
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








