Peroneal or fibular neuropathy is the most frequent mononeuropathy encountered in the lower limb. In this article, the causes, clinical features, electrodiagnostic assessment, and the treatment of peroneal neuropathies are described. Numerous causes have been reported to result in peroneal neuropathies, with mechanisms including compression, stretch, surgery, or trauma. Electrodiagnostics have been used to distinguish peroneal neuropathy from other disorders presenting with ankle dorsiflexor weakness. In addition, their use may aid in identifying the potential for recovery of functional movement.
Key points
- •
Fibular (peroneal) neuropathy is the most common mononeuropathy encountered in the lower limbs.
- •
Clinically, sciatic mononeuropathies, radiculopathies of the 5th lumbar root, and lumbosacral plexopathies may present with similar findings of ankle dorsiflexor weakness, thus evaluation is needed to distinguish these disorders.
- •
The most common site of injury to the fibular nerve is at the fibular head.
- •
The deep fibular branch is more frequently abnormal than the superficial branch.
- •
Electrodiagnostic studies are useful to determine the level and type (axonal, demyelinating) of injury.
- •
The presence of any compound muscle action potential response on motor nerve conduction studies, recorded from either the tibialis anterior or extensor digitorum brevis, is associated with good long-term outcome.
Introduction
Fibular or peroneal neuropathy is the most frequent mononeuropathy encountered in the lower limb and the third most common focal neuropathy encountered overall, after median and ulnar neuropathies. Following revised anatomic terminology published in 1998, the peroneal nerve is also now known as the fibular nerve, to prevent confusion of this nerve with those regions with similar names. Perone is another term for the fibula and, thus, this revised terminology for this nerve, its branches, and related musculature is based on language describing the location. While both fibular and peroneal are considered acceptable terms, “fibular” and it related terminology is preferred and therefore will be used throughout this article.
Weakness of ankle dorsiflexion and the resultant foot drop are common presentations of fibular neuropathy, but may also be seen in a wide variety of other clinical conditions, including sciatic mononeuropathy, lumbosacral plexopathy, or a lumbar (L) 5 radiculopathy. Additionally, ankle dorsiflexion weakness may be the initial presentation of generalized disorders, such as amyotrophic lateral sclerosis, or a hereditary neuropathy. In a retrospective series of 217 patients presenting with paresis or paralysis of foot dorsiflexors, of whom 68% had peripheral nerve abnormalities as the cause of their weakness, 31% had weakness related to a common fibular nerve lesion, 30% an L5 radiculopathy, and 18% due to a polyneuropathy. Fibular neuropathies may also present with predominantly sensory symptoms limited to the distribution of the deep or superficial fibular nerve or its branches. In addition to documenting fibular nerve abnormalities and the level of the injury, electrodiagnostic techniques have also been used to assess the potential for recovery of nerve function.
Introduction
Fibular or peroneal neuropathy is the most frequent mononeuropathy encountered in the lower limb and the third most common focal neuropathy encountered overall, after median and ulnar neuropathies. Following revised anatomic terminology published in 1998, the peroneal nerve is also now known as the fibular nerve, to prevent confusion of this nerve with those regions with similar names. Perone is another term for the fibula and, thus, this revised terminology for this nerve, its branches, and related musculature is based on language describing the location. While both fibular and peroneal are considered acceptable terms, “fibular” and it related terminology is preferred and therefore will be used throughout this article.
Weakness of ankle dorsiflexion and the resultant foot drop are common presentations of fibular neuropathy, but may also be seen in a wide variety of other clinical conditions, including sciatic mononeuropathy, lumbosacral plexopathy, or a lumbar (L) 5 radiculopathy. Additionally, ankle dorsiflexion weakness may be the initial presentation of generalized disorders, such as amyotrophic lateral sclerosis, or a hereditary neuropathy. In a retrospective series of 217 patients presenting with paresis or paralysis of foot dorsiflexors, of whom 68% had peripheral nerve abnormalities as the cause of their weakness, 31% had weakness related to a common fibular nerve lesion, 30% an L5 radiculopathy, and 18% due to a polyneuropathy. Fibular neuropathies may also present with predominantly sensory symptoms limited to the distribution of the deep or superficial fibular nerve or its branches. In addition to documenting fibular nerve abnormalities and the level of the injury, electrodiagnostic techniques have also been used to assess the potential for recovery of nerve function.
Anatomy
Common Fibular (Peroneal) Nerve
The common fibular (peroneal) nerve is derived from the lateral division of the sciatic nerve. Fibers from the dorsal fourth and fifth lumbar, as well as the first and second sacral nerve roots, join with tibial axons to form the sciatic nerve ( Fig. 1 ). Though bound in the nerve sheath with the tibial nerve in the thigh, the fibular and tibial axons are separate even within the sciatic nerve at this level. In the thigh, a branch arises from the fibular division of the sciatic nerve to innervate the short head of the biceps femoris. Following bifurcation of the sciatic nerve in the distal thigh at the superior popliteal fossa, the common fibular nerve travels along the lateral side of the fossa at the border of the biceps femoris muscle to the lateral knee. At this level, the nerve gives off a branch, the lateral cutaneous nerve of the calf, which supplies sensation to the upper third of the anterolateral leg. The sural communicating branch of the lateral sural cutaneous nerve joins with the medial sural cutaneous nerve to form the sural nerve. The common fibular nerve then travels superficially at the lateral fibula and is located about 1 to 2 cm distal to the fibular head before entering the anterior compartment of the leg where it divides into deep and superficial branches at the fibular head ( Fig. 2 ).
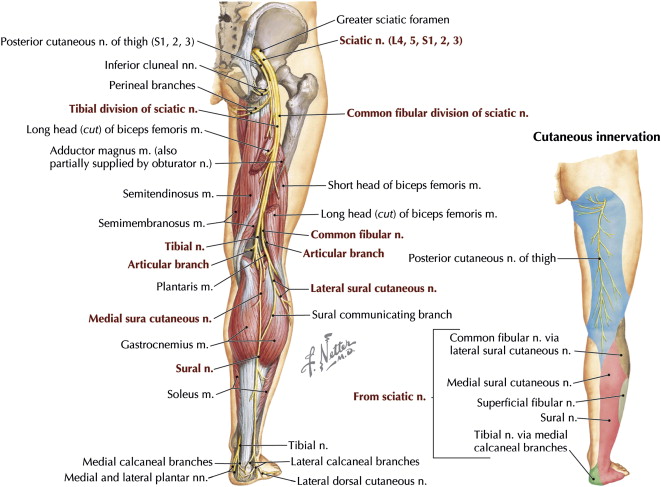

Deep Fibular (Peroneal) Nerve
The deep fibular (peroneal) nerve supplies motor innervation to all anterior compartment muscles (the tibialis anterior, the extensor digitorum longus, and extensor hallucis longus) and the fibularis tertius, also known as the peroneus tertius. The anterior tibialis is the strongest foot dorsiflexor, although the extensor digitorum longus and the fibularis tertius assist with this movement. The deep fibular nerve travels distally in the calf and at the level of the ankle joint, fascia overlying the talus and the navicular bind the deep fibular nerve dorsally. Ventrally, the extensor hallucis longus muscle fibers and tendon and the inferior extensor retinaculum overlay the nerve. The inferior extensor retinaculum is a Y-shaped band anterior to the ankle; the anterior tarsal tunnel is considered the space located between the inferior extensor retinaculum and the fascia overlying the talus and navicular. Just rostral or under the inferior extensor retinaculum, the deep fibular nerve branches into medial and lateral branches. The lateral branch of the deep fibular nerve travels under the extensor retinaculum, as well as the extensor digitorum and hallucis brevis muscles to innervate these muscles and nearby joints. The medial branch travels under the extensor hallucis brevis tendon to supply sensation to the skin between the first and second toes.
Superficial Fibular (Peroneal) Nerve
The superficial fibular (or peroneal) nerve arises from the common fibular nerve in the proximal leg and travels distally in the leg through the lateral compartment. After providing muscular innervation to the fibularis (peroneus) longus and brevis muscles in the lateral compartment of the leg, the terminal sensory branch supplies sensation to the lower two-thirds of the anterolateral leg and the dorsum of the foot, except for the first web space. It becomes superficial within the muscular compartment about 5 cm above the ankle joint where it pierces the fascia to become subcutaneous. It divides into its two terminal sensory branches, the intermediate and medial dorsal cutaneous nerves. The intermediate dorsal cutaneous nerve travels to the third metatarsal space and then divides into the dorsal digital branches to supply sensation to the lateral two digits. The medial dorsal cutaneous branch passes over the anterior aspect of the ankle overlying the common extensor tendons, runs parallel to the extensor hallucis longus tendon, and divides distal to the inferior retinaculum into three dorsal digital branches.
Accessory Fibular (Peroneal) Nerve
A common anatomic variant, the accessory fibular (peroneal) nerve, may be identified in the performance of studies to the extensor digitorum brevis. It generally arises from the superficial fibular nerve as it courses under the fibularis brevis muscle, traveling distally to the foot posterior to the lateral malleolus. It subsequently branches to innervate ligaments, joints, and the extensor digitorum brevis muscle. Prevalence as a normal anatomic variant has been reported to be 17% to 28% in anatomic studies and 12% and 22% electrophysiologically.
Causes
Fibular neuropathies are most often traumatic in origin; stretch or compression is a common feature in the history ( Box 1 ). Recurring external pressure at the fibular head may result in this complication, such as that seen in patients at bed rest or in individuals who habitually cross their legs. Intrinsic compression of the superficial and/or deep fibular nerves has also been described, such as that occurring from fascial bands or intraneural ganglia.
Knee or fibular head
- •
Anaphylactoid purpura
- •
Arthroplasty (knee)
- •
Arthroscopy (Knee)
- •
Baker cyst
- •
Bed rest
- •
Birth trauma
- •
Boney exostoses
- •
Casts
- •
Crossed-leg sitting
- •
Cryotherapy
- •
Fractures (femur, tibia, fibular)
- •
Fibrous arch
- •
Foot boards
- •
Ganglion
- •
Gun shot wounds
- •
Heterotopic ossification
- •
Hematoma
- •
Hemangiomas
- •
Intravenous infiltration or injections
- •
Knee dislocation
- •
Knee stabilization by helicopter pilots
- •
Kneepads
- •
Kneeling
- •
Lacerations
- •
Lipoma
- •
Knee surgery
- •
Schwannoma
- •
Sequential compression devices
- •
Sesamoid bone of the lateral head of gastrocnemius
- •
Severe valgus or varus deformity at the knee
- •
Splints
- •
Squatting (childbirth, strawberry picking, farm workers)
- •
Synovial cysts
- •
Traction
- •
Varicose vein surgery
- •
Venous thrombosis
- •
Water ski kneeboards
- •
Weight loss
Ankle or distal leg
- •
Ankle sprain
- •
Arthroscopy
- •
Boots
- •
Burn scar
- •
Edema
- •
Exertional compartment syndrome
- •
External fixator
- •
Fasciotomy for compartment syndrome
- •
Fascia
- •
Fracture
- •
Ganglion cyst
- •
Inferior extensor retinaculum
- •
Kneeling in prayer position
- •
Tightly fitting shoes
Acute fibular neuropathies located at the fibular head may be found in the setting of recent weight loss, frequently in conjunction with a history of leg crossing. Fibular nerve palsies were reported in prisoners of war during World War II who lost from 5 to 11 kg. In another case series, it was noted that 20% of 150 cases of fibular mononeuropathy were associated with dieting and weight loss. The mean weight decrease in these patients was 10.9 kg, with most patients having moderate to severe weakness of foot dorsiflexion and eversion. It has been theorized that loss of subcutaneous fat leads to increased susceptibility of the nerve to compression at this level. Fibular neuropathy associated with weight loss most often demonstrates conduction block on electrodiagnostic testing, with the severity correlating with clinical weakness. More recently fibular neuropathy has been described following bariatric surgery.
Significant trauma around the knee or ankle may result in fibular nerve injuries due to the nerve’s proximate and superficial locations at the level of these joints. Lacerations from saws, boat propellers, or lawn mowers have all been described. Not surprisingly, those with nerve in continuity have better recovery of function. Knee dislocations, particularly open, rotatory, or posterolateral corner injuries can results in proximal fibular nerve involvement. Deep fibular nerve abnormalities may be localized following spiral fibular fractures. Fractures requiring external fixation of the ankle may result in more distal injury. However, in the case of fractures, it has been noted that fibular neuropathy may be localized to the fibular head electrodiagnostically, though the fracture is an alternative location.
Although the most common site of injury following surgical procedures is at the fibular head, focal fibular neuropathies have also been reported at the level of the calf, ankle, and foot. Following total knee replacements, fibular nerve abnormalities may present with sensory symptoms or decreased range of motion. Following high tibial osteotomies, done in association with fibular osteotomies, fibular nerve abnormalities have been noted in 2% to 27% of cases. The abnormalities of ankle and toe extension and the sensory loss described following these procedures are thought to result from hardware placement, tourniquet effects, or the fibular osteotomy. Nerve abnormalities as the result of surgeries may be subclinical. In 11 cases studied prospectively with electrophysiologic testing, pre- and post-osteotomy surgery, abnormalities were present postoperatively in 27%, though only one patient was clinically symptomatic.
Fibular neuropathy is the most common lower limb mononeuropathy encountered in athletes. Common or proximal deep fibular nerve injuries at or near the level of the fibular head are most often found, particularly in football or soccer players, and may be seen in isolation or in association with severe ligamentous knee injuries or fractures. Some athletes reporting pain and weakness in a fibular nerve distribution have been found to have constriction of the nerve by the fibularis longus muscle. Acute or chronic exertional compartment syndrome may also result in foot drop and should be considered, particularly in athletes with intermittent complaints. Superficial fibular nerve injuries at the ankle have been described in soccer players. Due to excursion of superficial nerve with inversion, injury may be seen in association with ankle inversion sprains. Nerve abnormalities may also occur at the fibular head in the setting of ankle sprains due to traction of the nerve at the posterolateral knee because the patient’s foot is forced into plantar flexion and inversion.
Fibular neuropathies, though more frequently reported in adults, can also be seen in childhood. In a case series of 17 children, findings were similar to those of adults in that the common fibular nerve was most often injured (59%), as opposed to the deep (12%), superficial (5%), or a nonlocalizable level of injury (24%). Compression, trauma, or entrapment were the most common causes encountered.
Clinical features
Patients with fibular neuropathy often present with complaints of “foot drop” or catching their toe with ambulation, which may develop acutely or subacutely depending on the precipitating cause. There may also be complaints of sensory loss over the foot dorsum.
Clinical motor examination demonstrates weakness in ankle dorsiflexion and great toe extension with deep fibular and eversion weakness with superficial fibular involvement. Superficial peroneal nerve abnormalities are rarely present in isolation. Toe flexion and ankle plantar flexion strength should be normal. In the setting of a deep fibular neuropathy in conjunction with an accessory deep fibular nerve supplying complete innervation of the extensor digitorum brevis muscle, foot drop with preserved toe extension can be seen.
Sensory loss may be found over the foot dorsum (superficial branch) and/or in the first web space (deep branch). However, sensory symptoms may also be absent. More proximally, neuropraxia of the poster lateral cutaneous nerve of the calf has been reported with sensory deficits in the posterolateral upper calf. When symptoms are limited to the superficial sensory branches, generally patients complain of tingling, numbness, and/or pain in the distribution of the involved sensory fibers. In patients with entrapment of the superficial fibular nerve in the calf, these symptoms extend proximally or distally from the anterolateral leg. The distribution depends on whether one or both terminal branches of the superficial fibular nerve are involved. Those patients with entrapment in the calf fascia may note aggravation of symptoms with exercise. In these cases, a soft tissue bulge with resisted dorsiflexion of the ankle, and a Tinel sign or tenderness at the bulge has been described. In the case of more distal nerve involvement at the ankle, findings may be limited to the involved branches and isolated sensory loss involving specific superficial fibular nerve branches to digits 2 to 5 has also been documented.
The term anterior tarsal tunnel syndrome refers to compression of the deep fibular nerve under the inferior extensor retinaculum. Although the fibular nerve is a mixed sensorimotor nerve at the ankle, patients with anterior tarsal tunnel syndrome have been reported to describe more sensory symptoms. Primary complaints include numbness and paresthesias in the first dorsal web space that may awaken the patient from sleep.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







