This article describes the normal anatomy of the brachial plexus and its major terminal branches, as well as the major causes and clinical presentations of lesions of these structures. An approach to electrodiagnosis of brachial plexopathies and proximal upper extremity neuropathies is provided, with an emphasis on those nerve conduction studies and portions of the needle examination, which permit localization of lesions to specific trunks, cords, and terminal branches. The importance of specific sensory nerve conduction studies for differentiating plexopathies from radiculopathies and mononeuropathies is emphasized.
Key points
- •
The brachial plexus provides all motor and sensory innervation of the upper extremity.
- •
The plexus is usually derived from the C5 through T1 anterior primary rami, which divide in various ways to form the upper, middle, and lower trunks; the lateral, posterior, and medial cords; and multiple terminal branches.
- •
Traction is the most common cause of brachial plexopathy, although compression, lacerations, ischemia, neoplasms, radiation, thoracic outlet syndrome, and neuralgic amyotrophy may all produce brachial plexus lesions.
- •
Upper extremity mononeuropathies affecting the musculocutaneous, axillary, and suprascapular motor nerves and the medial and lateral antebrachial cutaneous sensory nerves often occur in the context of more widespread brachial plexus damage, often from trauma or neuralgic amyotrophy but may occur in isolation.
- •
Extensive electrodiagnostic testing often is needed to properly localize lesions of the brachial plexus, frequently requiring testing of sensory nerves, which are not commonly used in the assessment of other types of lesions.
Introduction
Few anatomic structures are as daunting to medical students, residents, and practicing physicians as the brachial plexus. Yet, detailed understanding of brachial plexus anatomy is central to electrodiagnosis because of the plexus’ role in supplying all motor and sensory innervation of the upper extremity and shoulder girdle. There also are several proximal upper extremity nerves, derived from the brachial plexus, which are not commonly tested in most electrodiagnostic evaluations but knowledge of which is important to any electromyographer involved in brachial plexus studies.
Patients commonly are referred to the electromyographer because of weakness, pain, or numbness of an upper limb, with a request to assess for brachial plexopathy. A properly trained electromyographer can combine sensory and motor nerve conduction studies with a detailed needle electromyographic examination to differentiate brachial plexopathy from radiculopathy, mononeuropathy, or mononeuropathy multiplex and then to localize the lesion within the brachial plexus. In this way, the electromyographer provides essential input, which the referring clinician can use for diagnosis, treatment, and prognosis.
Introduction
Few anatomic structures are as daunting to medical students, residents, and practicing physicians as the brachial plexus. Yet, detailed understanding of brachial plexus anatomy is central to electrodiagnosis because of the plexus’ role in supplying all motor and sensory innervation of the upper extremity and shoulder girdle. There also are several proximal upper extremity nerves, derived from the brachial plexus, which are not commonly tested in most electrodiagnostic evaluations but knowledge of which is important to any electromyographer involved in brachial plexus studies.
Patients commonly are referred to the electromyographer because of weakness, pain, or numbness of an upper limb, with a request to assess for brachial plexopathy. A properly trained electromyographer can combine sensory and motor nerve conduction studies with a detailed needle electromyographic examination to differentiate brachial plexopathy from radiculopathy, mononeuropathy, or mononeuropathy multiplex and then to localize the lesion within the brachial plexus. In this way, the electromyographer provides essential input, which the referring clinician can use for diagnosis, treatment, and prognosis.
Anatomy of the brachial plexus and its major branches
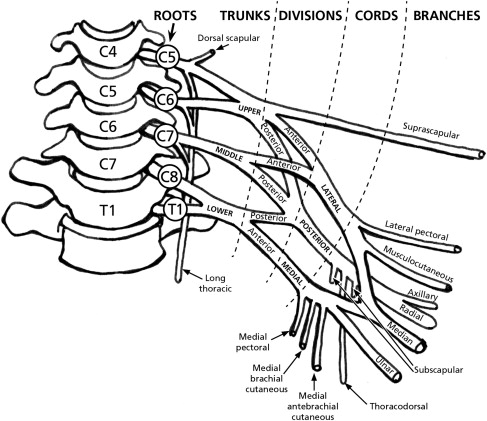
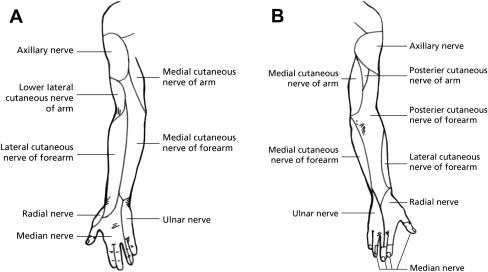
The brachial plexus has 5 components: roots, trunks, divisions, cords, and terminal branches ( Fig. 1 ). It runs behind the scalene muscles proximally and then behind the clavicle and pectoral muscles more distally as it courses from the neck into the shoulder girdle and arm. Proximal to the clavicle are the roots and trunks. Beneath it are the divisions. Distal to it are the cords and terminal nerve branches. In addition to providing the motor nerve supply to all muscles of the upper extremities and shoulder girdle, the brachial plexus supplies upper extremity cutaneous sensation ( Fig. 2 ). The major clinically significant terminal branches of the brachial plexus and their origins from the plexus are summarized in Table 1 . The components of the brachial plexus each have specific anatomic details with which the electromyographer should become familiar:
| Nerve | Origin |
|---|---|
| Dorsal scapular | C5 (±C4) root |
| Long thoracic | C5, C6 (±C7) roots |
| Suprascapular | Upper trunk |
| Lateral pectoral | Lateral cord |
| Musculocutaneous/lateral antebrachial cutaneous | Lateral cord |
| Medial pectoral | Medial cord |
| Medial brachial cutaneous | Medial cord |
| Medial antebrachial cutaneous | Medial cord |
| Ulnar | Medial cord |
| Median | Lateral and medial cords |
| Upper subscapular | Posterior cord |
| Lower subscapular | Posterior cord |
| Thoracodorsal | Posterior cord |
| Axillary | Posterior cord |
| Radial | Posterior cord |
Roots
The brachial plexus arises from the spinal cord at the C5 through T1 levels. Each of these levels gives rise to dorsal (sensory) and ventral (motor) rootlets, which then merge to form a short spinal nerve. This in turn divides into anterior and posterior primary rami ( Fig. 3 ). The anterior primary rami are often referred to as the roots of the brachial plexus and are located immediately external to the intervertebral foramina. There is anatomic variation. The term “prefixed plexus” is used when there is a contribution from C4 and the T1 contribution is minimal. In such cases, all the nerve contributions to the brachial plexus are shifted one level superiorly. In a postfixed plexus, there is a minimal contribution from C5 and a more substantial contribution from T2, resulting in the plexus being shifted one root level inferiorly. At times, the plexus may be expanded, with contributions from C4 through T2. Two branches originate directly at the root level: (1) the dorsal scapular nerve is derived from the C5 root, sometimes with a contribution from C4, and provides innervation to the major and minor rhomboid muscles and (2) the long thoracic nerve comes directly off the C5, C6, and sometimes the C7 anterior primary rami, innervating the serratus anterior muscle. Electromyographers should bear in mind that the cervical paraspinal muscles are innervated by the posterior primary rami and, therefore, can also be considered to have their innervation arise directly at the root level.
Trunks
There are 3 trunks. The upper trunk is formed by merger of the C5 and C6 roots. The middle trunk is the continuation of the C7 root. The C8 and T1 roots merge to form the lower trunk. One major branch and one minor one arise from the upper trunk. The suprascapular nerve, derived from the C5 and C6 roots, is the major terminal branch originating at the trunk level, coming off the upper trunk to provide innervation to the supraspinatus and infraspinatus muscles. It passes through the suprascapular notch of the scapula, an area covered by the transverse scapular ligament, and supplies motor branches to the supraspinatus muscle. Then, it continues around the spinoglenoid notch of the scapular spine (bounded by the scapula spine medially and the spinoglenoid ligament [inferior transverse scapular ligament] laterally) to supply motor branches to the infraspinatus muscle. The nerve to the subclavius is the minor branch of the upper trunk, which cannot be tested easily by physical examination or electrodiagnosis. There are no significant terminal branches arising directly from the middle or lower trunk.
Divisions
Each of the 3 trunks divides into an anterior and a posterior division, situated behind the clavicle. No terminal branches arise directly from the divisions.
Cords
The 3 cords are formed from the 6 divisions. The anterior divisions of the upper and middle trunks form the lateral cord, whereas the anterior division of the lower trunk continues as the medial cord. All 3 posterior divisions merge to form the posterior cord. Several terminal branches arise at the cord level.
Branches of the lateral cord: (1) The lateral pectoral nerve is derived from the C5-C7 spinal nerve levels and innervates the pectoralis major muscle. (2) The musculocutaneous nerve is derived from the C5-C6 spinal levels, sometimes with a contribution from C7. It innervates the coracobrachialis, biceps brachii, and brachialis muscles and gives rise to the lateral antebrachial cutaneous nerve (lateral cutaneous nerve of the forearm), which provides cutaneous sensation to the lateral forearm from wrist to elbow.
Branches of the medial cord: (1) The medial pectoral nerve is formed from C8 and T1 spinal nerves. It innervates the pectoralis minor muscle and the inferior portions of the pectoralis major muscle. (2) The medial brachial cutaneous nerve (medial cutaneous nerve of the arm) provides cutaneous sensation to the medial arm proximal to the elbow. (3) The medial antebrachial cutaneous nerve (medial cutaneous nerve of the forearm) provides cutaneous sensation to the medial forearm between the wrist and elbow. (4) The ulnar nerve arises from spinal levels C8-T1 primarily, usually with a contribution from C7. It supplies many forearm and hand muscles and provides cutaneous sensation over the medial hand, part of the ring finger, and all of the little finger.
Branch of both the lateral and medial cords: The median nerve is derived from spinal levels C6-T1. The motor fibers are derived from all these levels, whereas sensory fibers are derived primarily from C6-C7. Occasionally C5 contributes. Sensory fibers travel through the upper and middle trunks to the lateral cord. Motor fibers travel through all trunks to the lateral and medial cords. The different spinal level origins, and the different trunk and cord pathways, of the motor and sensory fibers, has meaningful clinical and electrodiagnostic implications for localization. The median nerve supplies forearm and hand muscles and cutaneous sensation over part of the hand.
Branches of the posterior cord: (1) The upper subscapular nerve is derived from the C5-C6 spinal levels and innervates the upper portion of the subscapularis muscle. (2) The lower subscapular nerve is derived from the C5-C6 spinal levels and innervates the lower portion of the subscapularis muscle and the teres major muscle. (3) The thoracodorsal nerve arises between the upper and lower subscapular nerves, derives from the C5-C7 spinal levels, and innervates the latissimus dorsi muscle. (4) The axillary nerve is derived from spinal levels C5-C7. It supplies the teres minor muscle and then terminates by innervating the deltoid muscle. It also supplies cutaneous sensation to the lateral aspect of the upper arm overlying the deltoid muscle. (5) The radial nerve arises from spinal levels C5-C8, occasionally with a T1 contribution. It supplies the triceps muscle, anconeus muscle, and muscles of the forearm and hand. It also provides cutaneous sensation to the arm, forearm, and hand as the posterior cutaneous nerve of the arm, lower lateral cutaneous nerve of the arm, posterior cutaneous nerve of the forearm, and superficial radial sensory nerve.
Causes of brachial plexopathy
There are many causes of brachial plexopathy, and these may result in lesions at many levels. A listing of the most common causes is provided in Box 1 . A few of these merit more detailed discussion.
- •
Traction
- ○
Fall from a height, particularly onto shoulder
- ○
Trauma in which the arm is pulled down, damaging the upper plexus
- ○
Trauma in which the arm is pulled up, damaging the lower plexus
- ○
Sports injuries, especially football
- ○
Motor vehicle accidents and other trauma
- ○
Obstetric paralysis
- ○
Surgery, particularly during median sternotomy
- ○
- •
Compression
- ○
Supraclavicular plexopathy from pack straps
- ○
Infraclavicular plexopathy from crutches
- ○
Hematoma, aneurysm, arteriovenous malformations
- ○
- •
Lacerations from penetrating injuries
- ○
Gunshot or other missile
- ○
Knife or other penetrating sharp object
- ○
Neurovascular injury, particularly during trauma
- ○
- •
Ischemia
- •
Neoplastic infiltration
- •
Radiation therapy
- •
Thoracic outlet syndrome
- •
Neuralgic amyotrophy (Parsonage-Turner syndrome)
- •
Iatrogenic injury
- ○
Direct injury during surgery
- ○
Traction
Traction injuries are common. There are many causes, including a fall onto the shoulder from a height, traction to a limb when it is pulled severely, sports injuries (particularly in football), and closed traction during motor vehicle accidents. Traction during surgery may result in postoperative brachial plexopathy. This plexopathy most commonly occurs after chest surgeries due to stretch injuries to the plexus from chest wall retraction. The lower trunk or medial cord usually is involved, with the expected clinical presentation as described later in this article. Recovery depends on the severity of axonal injury. Obstetric paralysis typically has been attributed to traction on the neck by the clinician during passage in the birth canal. However, it now appears that some of these injuries develop prenatally or are due to propulsive forces over which the birth attendant does not have control. Upper or upper and middle plexus involvement are most common, although about 23% of infants sustain panplexus injuries.
Neoplastic and Radiation-induced Brachial Plexopathy
Radiation-induced brachial plexopathy is most commonly a delayed syndrome, occurring from a few weeks to many years after radiation. The higher the radiation dose, the higher the risk of developing a radiation-induced brachial plexopathy. The electromyographer is most often called on to distinguish a radiation-induced plexopathy from one due to neoplastic infiltration. Radiation-induced plexopathy is less likely to be painful, and more likely to be characterized by progressively evolving sensory disturbances. Electrodiagnostically, myokymic discharges and fasciculation potentials are more likely to be present in radiation-induced plexopathy. In contrast, neoplastic brachial plexopathy usually is characterized by prominent pain, more rapidly developing symptoms, often accompanied by a Horner syndrome, and rarely associated with fasciculation potentials or myokymia. Tumors at the lung apex (Pancoast tumors) most commonly invade the lower portion of the plexus, but metastases from other types of malignancies or direct infiltration of the nerves or nerve sheaths can also occur at any level of the plexus.
Thoracic Outlet Syndrome
This syndrome has been the subject of extensive review, to which the interested reader is referred. True neurogenic thoracic outlet syndrome is rare. Most are caused by a fibrous band from a rudimentary cervical rib to the first thoracic rib, which entraps the lower trunk of the brachial plexus. Thus, the clinical presentation and the electrodiagnostic findings are those of a lower trunk brachial plexopathy, the exception being that the T1 fibers usually are preferentially affected, resulting in greater atrophy of the thenar than hypothenar mucles. Sensory loss parallels that seen in lower trunk plexopathies.
Neuralgic Amyotrophy (Parsonage-Turner Syndrome)
Also termed immune brachial plexus neuropathy, this condition is most commonly sporadic, although it may be familial. First described in detail in the modern era by Parsonage and Turner in 1948 and then described in detail with respect to its natural history more than 20 years later, this condition is now well recognized by most neurologists, but often unknown to nonneurologists and confused with cervical radiculopathy. Individuals of all ages may be affected, and there is a male predominance. The symptoms are widely varied, as has been well described. Most commonly, the initial symptom is pain of abrupt onset, often severe, usually in the shoulder or periscapular region. Pain generally begins to improve in 2 to 3 weeks, in association with the development of weakness. The weakness may involve the brachial plexus in a patchy fashion, for example affecting one or more trunks or single peripheral nerves, most commonly the long thoracic, suprascapular, or axillary nerves. Bilateral involvement occurs in about one-third of patients, usually asymmetrically. It may be preceded by a flulike or other febrile illness. Reports of this syndrome following a variety of conditions (immune, infectious, neoplastic, traumatic, etc) have been reported, suggesting that a variety of events can trigger an immune-mediated attack on the brachial plexus. Electrodiagnostic studies may reveal a pattern of brachial plexus involvement not readily localizable to one or more specific trunks, divisions, cords, or peripheral nerves. This patchy or multifocal involvement is common and is a hallmark of this syndrome. Pathogenetically, this condition appears to be an inflammatory, immune-mediated process.
Causes of proximal upper extremity neuropathies
Medial Antebrachial Cutaneous (MAC) Nerve
Lesions generally arise from lesions that affect the lower trunk or medial cord of the brachial plexus. Several causes of brachial plexopathy are particularly likely to affect the lower trunk or medial cord and thus the MAC nerve: (1) trauma in which the arm and shoulder are pulled up; (2) invasion of the plexus by a Pancoast tumor at the lung apex; (3) stretch injuries of the lower plexus during chest surgery such as coronary artery bypass surgery; and (4) thoracic outlet syndrome entrapping the lower trunk of the plexus.
Musculocutaneous Nerve
Lesions are most commonly caused by trauma to the shoulder and upper arm, especially factures of the proximal humerus from falls or sports injuries. In such cases, other nerves usually are damaged as well. For example, primary shoulder dislocations or fractures of the humeral neck may result in injuries to several nerves, including the axillary, suprascapular, radial, and musculocutaneous nerves. Other forms of trauma, including gunshot wounds and lacerations, also may produce musculocutaneous nerve lesions. Isolated nontraumatic lesions of the musculocutaneous nerve are rare, usually occurring as it passes through the coracobrachialis muscle. Causes include weightlifting or other vigorous physical exercises, as well as surgery, pressure during sleep, and malpositioning during anesthesia. Rare cases of musculocutaneous nerve compression have included repeated carrying of items on the shoulder with the arm curled around the item, or osteochondroma of the humerus compressing the musculocutaneous nerve. The musculocutaneous nerve may also be involved in neuralgic amyotrophy.
Lateral Antebrachial Cutaneous (LAC) Nerve
Injuries can occur in isolation without involvement of the main portion of the musculocutaneous nerves. The LAC nerve may be entrapped, usually at the elbow, where it is compressed by the biceps aponeurosis and tendon against the brachialis muscle. Other causes of isolated LAC injury include hyperextension injury of the elbow, such as during sports, and antecubital phlebotomy.
Axillary Nerve
This is most commonly damaged by trauma, including shoulder dislocations, fractures of the humeral neck, blunt trauma to the shoulder in contact sports, gunshot wounds, and injections. Compression may produce an axillary neuropathy during general anesthesia or by sleeping with the arms above the head. The nerve may be entrapped within the quadrilateral space (formed by the humerus, teres minor muscle, teres major muscle, and long head of the triceps muscle) by muscular hypertrophy and repetitive trauma in athletes such as tennis players and baseball pitchers. As for other upper extremity neuropathies, neuralgic amyotrophy may be a cause.
Suprascapular Nerve
This may be entrapped as it passes through the suprascapular notch, or, less commonly, as it passes through the spinoglenoid notch. Causes of suprascapular nerve entrapment also include mass lesions such as ganglion cysts, sarcomas, and metastatic carcinomas. Traumatic causes of suprascapular neuropathy include shoulder dislocation or protraction or scapular fracture, as well as injuries that generally produce more widespread damage to the brachial plexus such as stretch, gunshot, and penetrating injuries. Weightlifters may suffer suprascapular neuropathies, probably due to repetitive movement of the scapula. Other athletic activities involving overhand activities can predispose individuals to suprascapular entrapment, particularly at the spinoglenoid notch. Such injuries are particularly common in professional volleyball players but also are seen in baseball pitchers and dancers. As with many other upper extremity neuropathies, the suprascapular nerve also may be affected in neuralgic amyotrophy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






