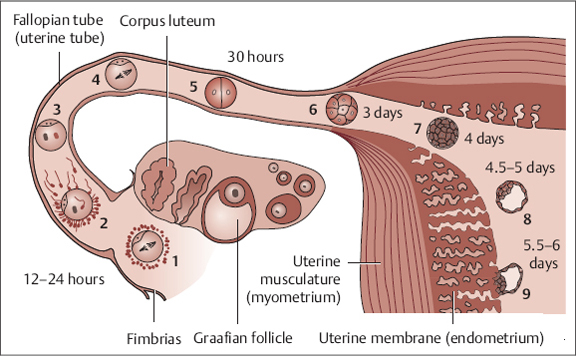
2 Fertility Treatment and Pregnancy— Reproductive Medicine and TCM in Meaningful Cooperation When we consider the modern options of reproductive medicine in the holistic care of couples, the question arises whether Western scientific medicine and TCM might not be able to complement and approach each other with regard to the different medical theories underlying both systems. By now, solid scientific studies exist that indicate the successful results of such cooperation. The necessity of combining biomedical reproductive medicine and TCM makes sense even on the most basic level since the principle of individualized treatment in TCM complements the normative approach of biomedical treatment. The following paragraphs therefore shed light on the one hand on those areas where the strengths and therefore indications of the biomedical approach are situated, and on the other hand on those areas where TCM offers advantages to couples in regard to diagnosis and treatment of reproductive disorders. The goal of a successful pregnancy requires a whole series of preliminary conditions: In biomedicine, the “quality” of the gametes (reproductive cells with half the set of chromosomes) is seen as being of paramount significance. We now know that a hormonal disturbance with an elevated level of male sex hormones (hyperandrogenism, often so-called polycystic ovary syndrome [PCOS]) in women drastically reduces the quality of eggs and therefore the likelihood of pregnancy. Such hormonal disturbance is partly related to the patient’s state of being considerably overweight. The quality of a woman’s eggs is furthermore limited—as we know well—particularly by increasing age. The loss of quality is primarily because a woman’s supply of eggs is limited. This supply peaks during the woman’s own fetal stage. At the time of birth, it consists of approximately 500 000 primordial follicles (immature egg cells in the ovaries). With the exception of the 400–500 oocytes that reach ovulation during the course of a woman’s fertile years, all others will spontaneously perish throughout her life. Furthermore, the development from primordial follicle to pre-ovulatory follicle takes almost a year (see Fig. 6.1); it is only in approximately the last 4 weeks before ovulation itself that the follicle is controlled by hormones via the female cycle.29 In a process called meiosis (reduction division of reproductive cells), the set of chromosomes in the cells is cut in half, into a single chromosome set. It is significant here that the oocytes remain arrested in this so-called first meiotic division during the entire time (longest period of cell division in humans up to ca. 50 years). This makes the oocytes particularly susceptible to damaging factors such as: As such, the rate of aneuploidy in oocytes increases with advancing age (> 50% of oocytes). As we know today, genetic disposition is also particularly significant in that it determines the number of initiated oocytes in the ovaries and influences the spontaneous decrease of eggs in the course of the woman’s life. Additional factors that affect egg quality in women from a biomedical perspective are inflammations of the ovaries or autoimmune diseases (thyroid glands, the so-called antiphospholipid syndrome, autoimmune disorders, hereditary coagulation disorders). In this short and obviously incomplete presentation of biomedical notions regarding the significance of oocyte quality, we can already see the importance of bodyweight (especially at the time of puberty!) and lifestyle. In this context, TCM and biomedical strategies can be used together preventatively, in which case TCM surely offers more varied and individual treatment concepts: from lifestyle advice, nutritional therapy, and qi gong to medicinal therapy, a multiplicity of options exist for influencing gamete quality and quantity. For the man, the situation is more complicated. We know today that excess weight and smoking have a considerable influence on sperm quality. In addition, biomedicine recognizes a multitude of factors that are said with more or less certainty to contribute to a decrease in semen quality. For some of these factors, the influence on sperm quality is only temporary; hence it makes sense to have a control spermiogram done after a so-called completed sperm cycle of 3 months or possibly even later (e. g., in cases of low sperm quality due to anabolic therapy related to bodybuilding). It has become apparent that spermiogenesis is characterized by considerable inter-individual sensitivities that may be genetically determined. There is also a connection here to undescended testes as a cause of reduced sperm cell formation (testicular dysgenesis). Biomedicine recognizes that after puberty, viral infections in particular can gravely affect spermiogenesis, with a possible complete destruction of the sperm-forming tissue. Many of these different factors have in common that they ultimately harm spermiogenesis by elevating the level of extra- and intracellular free oxygen radicals and can thereby even trigger point mutations. Biomedicine attempts to counteract this action with high dosages of vitamin E and zinc. In this area, TCM also offers options. For successful fertilization, the ratio between egg cells and sperm cells is also decisive. At the site of natural fertilization, namely the ampulla of the fallopian tubes, an estimated ratio of one ovum (still encapsulated by the surrounding tissue) (Fig. 6.1) and ca. 100 000–150 000 motile spermatozoa is needed. It is only in the woman’s inner genitalia that the spermatozoa reach their full functionality, that is, the penetration of the surrounding tissue to reach the ovum itself, the penetration of the zona pellucida that encases the ovum, and the fusion of the cell membranes of the sperm and egg. This process is called capacitation. Success is possible only for quickly moving and normally formed spermatozoa. We can assume a normal probability of fertilization when a man’s sperms exceed the minimum values (Table 6.1). Fig. 6.1 Fertilization, fallopian tube transport, and implantation. Schematic presentation of the developmental processes in humans in the first week: 1 ovum directly after ovulation; 2 fertilization within 12–24 hours; 3 stage with male and female pronucleus; 4 zygote, 1st cleavage; 5 two-cell stage; 6 morula stage; 7 entry into the uterine cavity; 8 blastocyst with blastocyst cavity; 9 early stage of nidation (implantation).
6 Fertility Treatment and Pregnancy—Reproductive Medicine and TCM in Meaningful Cooperation
Karin Kielwein, Fransiscus X. Sulistyo-Winarto, Kerstin Friol, and Christian Gnoth
Introduction
Requirements for a Successful Pregnancy
Requirements in the Woman
Requirements in the Man
| Criteria | Values |
| Ejaculate volume per ejaculation | > 2.0 mL |
| pH | 7.2–8.0 |
| Sperm concentration | > 20 million spermatozoa/mL |
| Total sperm count | > 40 million spermatozoa |
| Motility (mobility) | > 25% rapidly progressing sperm of category a, or > 50% forwardly motile sperm of category a + b |
| Morphology | > 30% normally formed sperm |
| Viability (proportion of living sperm) | > 75% vital spermatozoa (eosin test) |
| MAR test (spermatozoa—autoantibody determination) | < 10% spermatozoa with particles |
| Leucocytes | < 0.5 million/mL |
| Round cells | < 1 million/mL |
| Alpha-glucosidase | > 11mU/ejaculate |
| Fructose | > 13 μmol/ejaculate |
| Zinc | > 2.4 μmol/ejaculate |
Requirements During Fertilization
If these requirements are met and a mature oocyte has emerged in the cycle (i. e., the first maturation division of meiosis is completed all the way), the gametes must come together. From the sperm deposit in the back of the vaginal cavity, rapid periovulatory penetration into the highly fertile cervical mucus occurs.
The sperm cells reach their full fertilizing capacity in this cervical mucus; a selection process takes place that effectively separates highly motile, normally formed sperm cells from less motile, morphologically conspicuous cells. The sperm do not swim into the fallopian tube completely on their own accord; rather, we now have proof of a targeted, uterotubal transport to the site of ovulation. Precondition for a normal transport of spermatozoa to the oocyte in the ampulla of the fallopian tube is, of course, that the woman’s inner genitals are anatomically normal. Uterine deformities (partitions, complete bisection of the uterus) that disrupt this transport and can be responsible for repeated miscarriages later are not rare. In addition, myomas, polyps, and a dispersed uterine lining (endometriosis) can also disrupt this process considerably. Much more common in previous times than today were completely blocked fallopian tubes after inflammation (adnexitis). Nowadays, especially chlamydial infections play an important role: they are often overlooked as the source of inflammation and remain undiagnosed and untreated because they produce few if any symptoms. In cases of uterine deformity or complete fallopian tube blockage, biomedical methods with microsurgical operations and, if necessary, subsequent assisted fertilization (in vitro fertilization) are certainly superior to the options of TCM.
Requirements During Nidation
Once the embryo has arrived in the uterus, it requires an endometrium prepared for implantation in the early secretory stage in order to implant there. Influencing uterine conditions to prepare for implantation is possible in both systems: on the part of TCM, by nourishing blood and yin, and on the part of Western biomedicine, by hormonally supporting the luteal stage. The options of modern reproductive medicine in this context consist specifically of supporting a synchronous proliferation of endometrial cells, mainly procured by estrogen. After ovulation, a marked increase in progesterone causes the so-called secretory transformation of the mucus and opens the implantation window. In humans, we can assume that the implantation window opens by about the second day of the progesterone increase and closes again about 7–9 days thereafter. Synchronization with embryonic development is essential. In humans, the embryo reaches the uterine cavity about 6 or 7 days post-conception. Strictly speaking, this is a capillary gap in which the embryo continues to move around in a layer of fluid due to peristaltic movements of the uterine muscles. Shortly before implantation, however, the human embryo must slip out of its cover (zona pellucida) when it reaches the uterine cavity (so-called “hatching”).
We still do not understand the details of the process of implantation with all its contributing factors because the situation is completely different in other mammals. Of foremost importance is the viability of the embryo, as a result of which implantation is possible also in the periphery of the implantation window. Even implantation completely without endometrium (fallopian or abdominal pregnancy) is possible in humans, in contrast to the situation in animals. As we know from reproductive medicine, the human embryo (again, in contrast to the animal kingdom) can “wait” for the implantation window to open. This is of the greatest significance for the question on which day after oocyte punction the embryo transfer should take place. We know that vital embryos secrete typical patterns of growth factors for blood vessels and protein-splitting enzymes (so-called metalloproteinases) for optimal implantation. Apparently, implantation does not follow the rule of “all or nothing”; on the contrary, we nowadays assume that qualitative differences exist. Later pregnancy complications such as high blood pressure, retarded growth, premature detachment of the placenta, and intrauterine fetal death are sometimes attributed to early implantation problems. Some miscarriages are also caused by implantation mistakes, as we know, for example, in serious corpus luteum insufficiency with progesterone deficiency.
As a rule, highly targeted intervention, as is often desired by Western medicine, is very difficult in this complex event; at the same time, therapeutic effects are therefore also difficult to evaluate or prove. Herein lies the strength of TCM.
Causes of Subfertility and Infertility in Women and Men
The Four Phases of the Menstrual Cycle from the Western and TCM Perspective
The first phase, the menstrual period (day 1–5), is defined by a sharp drop in estrogen and progesterone levels, as a result of which the endometrium is deprived of nourishment, becomes necrotic, and is expelled with the blood. In TCM, we have to ensure in this phase that qi and blood flow freely, to guarantee the gentle shedding of old blood (Fig. 6.2).
In the second phase, the follicular phase (around day 6–11) the follicle grows under the influence of the follicle-stimulating hormone (FSH), the estrogen level rises, and the lining of the uterus is rebuilt. After blood and yin have been lost in the first phase, they must be nourished in this phase to allow the egg cells to mature and to build a well-nourished endometrium.
In the third phase, the ovulatory phase (around day 11–17), the release of luteinizing hormone (LH) causes the follicle to rupture and release the ovum. The corpus luteum is formed from the ruptured follicle. The chong mai and ren mai gradually fill up in this phase, and ovulation takes place. This dynamic process corresponds to the transition from the yin to the yang stage of the cycle.
In the fourth phase, the luteal phase (around day 18–28), the corpus luteum grows and secretes progesterone. The yang qi increases and liver qi is mobilized, in order to then be able to move the blood during menstruation. Treatment strategies should be designed in accordance with these phases.
Probabilities of Pregnancy
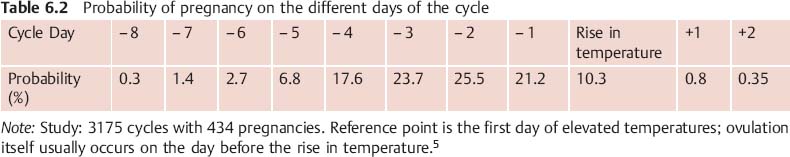
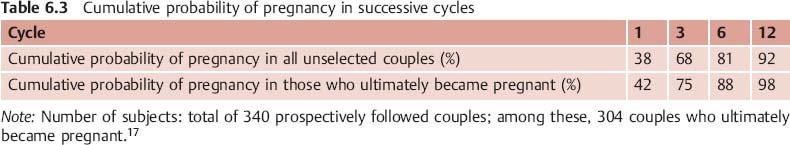
These days, it is not uncommon that women and men practice birth control sometimes for 20 years before they think of realizing their wish for children. The remaining 20% of the woman’s fertile years are unfortunately also the ones that are least fertile. Thus, the biological clock begins to tick sooner or later. Today, about every sixth couple suffers—at least temporarily—from the problem of unwanted childlessness. Table 6.2 shows that the probability for a pregnancy is greatest 1–2 days before ovulation.
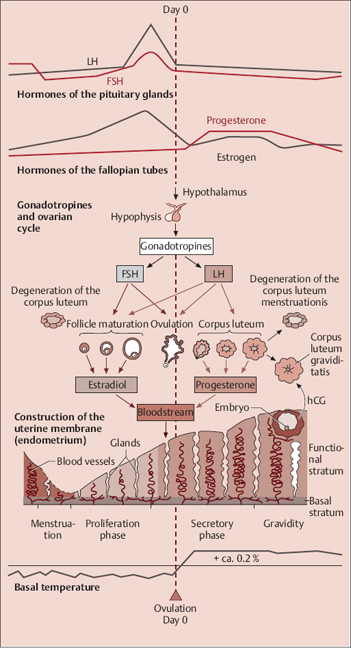
Fig. 6.2 Synchronized processes in the menstrual cycle (modified based on Faller).
The maximum probability of pregnancy in a cycle with intercourse on every fertile day lies around 27%. For the definition of subfertility and sterility, the question of pregnancy probability is, of course, more interesting in a series of cycles (cumulative probability of pregnancy). Here, Table 6.3 shows that after three cycles approximately 70%, and after six cycles approximately 80% of all couples who had intercourse in the highly fertile time became pregnant. Of the successful couples, as much as almost 90% became pregnant within the first six cycles. In only 2% of couples, it took more than 12 cycles.
We can thus assume after six unsuccessful cycles with intercourse in the most fertile time that a mild impairment of fertility is already present and that in such cases every second couple could even suffer from an impairment of fertility. On the other hand, though, chances of a natural pregnancy are not bad either for couples who have not had success after 1 year. The reason for this is that approximately half of those couples can count on a child in the next 36 months. After 4 years of unsuccessfully trying to get pregnant at the latest, we can speak of a definitely sterile partnership. After that, only sporadic chances exist for a natural pregnancy (Table 6.4).
We know that the woman’s age plays a significant role. With increasing age, the risk of fertility problems clearly increases. Nevertheless, differences between women increase with increasing age, that is, a growing percentage of women suffer from considerable fertility problems on the one hand, but there are still some women with very high fertility on the other. For this reason, it is very important for women over 30 and especially for women over 35 to know whether they can wait longer after six unsuccessful cycles or whether a personal fertility problem is reducing their chance for a natural pregnancy.
Causes of Subfertility and Infertility in Women and Men
Modern medicine by now possesses easily performed and dependable diagnostic methods for identifying couples with a possibly bad prognosis for a spontaneous pregnancy. This is very important because in cases with a fertility problem, enough time must remain for utilizing the tools of reproductive medicine. For a woman past the age of 40, the chance of becoming pregnant with the assistance of reproductive medicine is only about 10–20% of that of a woman aged 30–35. The most important factor is here the declining function of the ovaries.
| Of All Couples Desiring Children | ||
| After six unsuccessful cycles | ca. 20% at least mildly subfertile couples | i. e., 50% of these couples will conceive in the next six cycles; the other half is considerably subfertile or infertile |
| After 12 unsuccessful cycles | ca. 10% considerably subfertile couples (old clinical definition of sterility) | i. e., ca. 50% of these couples still have a chance of spontaneously conceiving in the next 36 months (!); the other half is infertile |
| After 48 unsuccessful months | ca. 5% definitely infertile couples | i. e., with only sporadic chances of conceiving |
There are many reasons why a pregnancy does not occur. In the woman, we have to check for:
- hormonal disorders (disturbed hypothalamic regulation, hypophysic insufficiency, polycystic ovary syndrome, premature ovarian exhaustion, disturbed thyroid function, hyperprolactinemia)
- a declining reserve of ovarian function (age, previous surgery)
- anatomical changes in the female genital organs (e. g., tubal occlusion, uterine deformity, cervical sterility, e. g., after surgical intervention in conization or after inflammation)
- endometriosis
In the man, we have to check for:
- damage to the testicles resulting in insufficient semen production
- congenital or acquired blockage of the vas deferens
- ejaculatory disorders
The cause is also often found in both partners, such as, for example, in compatibility disorders (immunological sterility, often as a result of inflammation in the area of the inner genitals). Mild disturbances in both partners frequently add up, to the point where nature is no longer able to compensate. Western medicine nowadays fails in every fifth to 10th case to find the precise cause for infertility (so-called idiopathic sterility).
Diagnosis of Subfertility, Infertility, and Sterility
The diagnostic tools of reproductive medicine in subfertility, infertility, and sterility of men and women consist of:
- hormonal tests: especially gonadotropin (LH and FSH), examinations of the androgen meta bolism, anti-Mullerian hormone, endometriosis activity parameter (CA 125), thyroid hormones, prolactin
- ultrasound
- hysteroscopy and laparoscopy
- screening for infections
For TCM practitioners the so-called cervix factors (especially cervical mucus quality and quantity, opening of the uterine orifice, position and consistency of the portio uteri) and the basal temperature curve carry a high diagnostic value.
In contemporary scientific literature, the term “basic infertility workup” after six unsuccessful cycles has gained acceptance. In this basic examination, the levels of the gonadotropins LH and FSH, AMH, TSH, prolactin, testosterone, androstenedione, and DHEAS (dehydroepiandrosterone) are determined on the third to fifth day of the cycle to clarify the endocrinological environment, and a basic ultrasound is performed to count the number of small antral follicles (6–8 mm diameter) in both ovaries. In addition, a further ultrasound examination can be carried out around the time of ovulation at the peak of mucus secretion (see p. 49) as evidence for the development of a dominant follicle and synchronous development of the endometrium. At the same time, this examination can also determine simple uterine anomalies like an adenomyosis uteri. The basic ultrasound exam also serves to purposely eliminate the possibility of myomas, polyps, a hydrosalpinx, and uterine deformities. Also on the day of maximum mucus level, a postcoital test can be carried out to exclude the possibility of interaction disorders and of cervical sterility. This test has a high prognostic value in cases of idiopathic sterility (spontaneous conception probability). In cases of suspected uterotubal pathology, a hysteroscopy and hysterocontrastsonography, possibly also a laparoscopy with chro-mopertubation, can be performed in the first half of the cycle. Due to its invasive nature, though, the indication for a laparoscopy with chromopertubation should be given only under strict parameters and has on the whole declined in significance.
Six to 8 days after the rise in temperature, determining the level of estradiol and progesterone can prove the sufficient luteinization of the dominant follicle and eliminate a latent weakness of the corpus luteum.
Of course, the beginning of any check-up on subfertility and infertility also includes an examination of the man. After 3–5 days of rest, a basic spermiogram in accordance with WHO criteria should be carried out (see Table 6.1). In addition, in cases of suspected limited male potency (condition after undescended testicles, condition after infections, absence of male gametes in the sperm, ejaculatory disorders, condition after varicocele surgery, condition after surgery in the groins), an andrological examination should be carried out that includes determining testicular volume, checking testicular circulation, and a testicular sonography.
Due to the special significance in TCM, the examination of the uterine cervix is presented here in greater detail. The cervical mucus changes in quality in relation to the phases of the cycle (Fig. 6.3). Under the influence of estrogen, it becomes increasingly clear and stretchable (spinnbarkeit), which is an important precondition for the capacitation of the sperm.
In addition, the portio uteri becomes deeper and the external os of the uterus widens. This stage signifies the optimal point for conception. At the same time, scientific research has shown that the quality of the cervical mucus on the day of intercourse is more important for maintaining optimal conception chances than the distance in time between intercourse and ovulation itself.
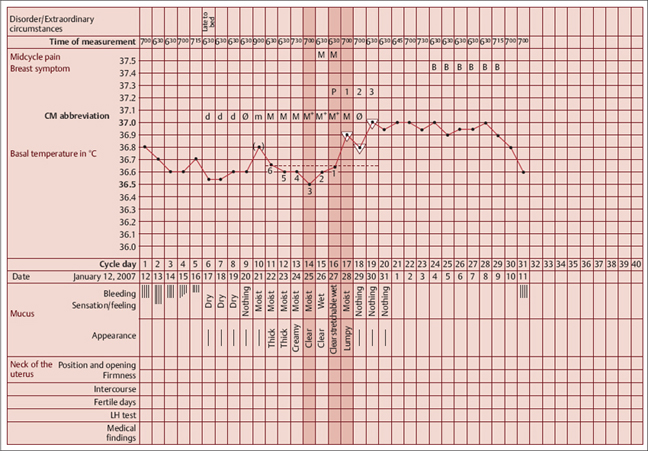
An additional method of infertility diagnosis is the course of the basal temperature curve. The basal temperature is the body temperature measured in the morning after waking up. At the time of ovulation or shortly thereafter, the core body temperature rises slightly (basal temperature curve, BT), due to the effect of progesterone on the hypothalamus and the slowing down of skin circulation; the temperature does not drop back down until the end of the cycle. The rise in temperature is often relatively small, sometimes only 0.2°C (0.4°F). This rise is proof for the luteinization of the mature follicle, hence almost always also for ovulation itself. For measuring the basal temperature curve, the following is important:
- Measure in the morning: immediately after waking, before getting up, before any other activity.
- Measure for 5 minutes, orally or vaginally, not under the arm.
- Do not change the method of measuring within one cycle.
- After disturbed nightrest: sleep or relax in bed for about an hour before measuring.
- Begin measuring after the menstrual period when cervical mucus production starts.*
- You can stop measuring after the rise in temperature.
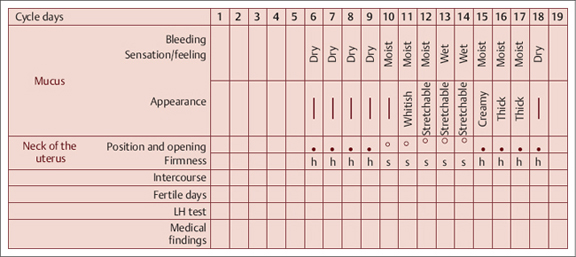
Fig. 6.3 Typical change in cervical mucus and portio uteri in the course of the cycle.
___________
Possible factors that interfere with the temperature are:
- unusually late measuring time
- going to bed unusually late
- unusual alcohol consumption
- late partying
- stress
- emotional strain
- traveling
- climatic change
- short or interrupted night’s sleep
Ideally, the temperature values are entered in a cycle sheet with 0.1 °C (0.2 °F) gradation. The temperature values are connected to each other. In addition, you should also enter symptomatic information on the cervical mucus and the pattern of bleeding.
Ignore any abnormal elevated temperature values that jut out upward from the usual range of variation among the low temperature values before ovulation and that can be explained by a potential interference factor; disregard these in the analysis of the curve in accordance with the rules of the symptothermal method of natural family planning. It is important to recognize the rise in temperature because this indicates whether and when ovulation has taken place.
Symptothermal Method of Natural Family Planning
The rules of the symptothermal method of natural family planning (STM of NFP) serve to identify the correct rise in temperature instead of wrongly identifying another elevation in temperature as the temperature rise. A temperature rise (Fig. 6.4) has taken place when three successive readings are higher than the six previous readings (the so-called “three-over-six rule”).
In addition, the third higher reading must be at least 0.2 °C (0.4 °F) higher than the highest of the preceding six low temperature readings.
Note the following two exceptions:
- If the third temperature reading is not 0.2 °C (0.4 °F) higher, you have to wait for a fourth reading, which merely has to lie above the six low values (Fig. 6.5).
- In between the three higher values, a reading can fall below or on the imagined line through the preceding six low temperature readings. This value is then ignored in the analysis of the temperature rise (Fig. 6.6).
The rules of the STM of NFP have been validated in numerous studies; additional information on the rules of the STM of NFP can be found in the literature.1
Ovulation usually takes place 1–2 days before the first higher reading, occasionally also on the first day of the higher reading itself. For diagnostic purposes in biomedicine as well as in TCM, additional symptoms can be entered on the cycle sheet, such as mid-cycle pain, mastodynia (pain in the breasts), ovulation bleeding, as well as consistency and position of the vaginal portion of the cervix.
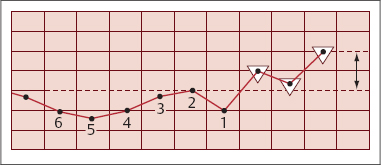
Fig. 6.4 Determining the rise in temperature.
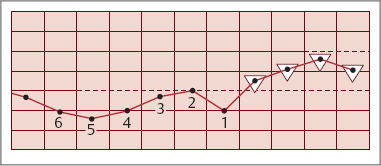
Fig. 6.5 Determining the rise in temperature; exception 1.
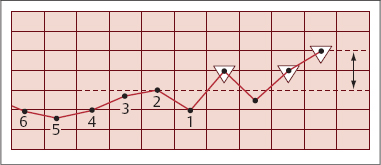
Fig. 6.6 Determining the rise in temperature; exception 2.
Due to its special significance in TCM diagnostics, we discuss the interpretation of the basal temperature curve in more detail below (see pp. 59 ff). Fig. 6.7 shows a typical BT curve of a healthy woman.
Biomedical Methods for the Treatment of Infertility and Sterility
The therapeutic strategies of TCM must be synchronized with those of biomedicine. In order to accomplish this, it is necessary to acquire a basic knowledge of modern reproductive medicine in addition to the suitable treatment strategies and principles of TCM. In this section, we explain the basic terms of reproductive medicine and its therapeutic techniques.
Depending on the cause of infertility, different therapeutic approaches are utilized. Here, we present a hierarchy of the various options for intervention by means of reproductive medicine—from less invasive to highly invasive methods. These are selected in accordance with the type of disorder:
- Hormone therapy for cycle optimization (supporting follicular maturation and optimizing the luteal phase for intercourse at the optimal point in time):
- oligomenorrhea
- luteal insufficiency
- for the timing of ovulation
- oligomenorrhea
- Intrauterine insemination (IUI):
- mildly deficient sperm quality
- interactive disorders in the area of the cervix (so-called immunological sterility)
- cervical sterility
- idiopathic sterility
- impotentia coeundi (inability to complete intercourse)
- uterotubal transport disorders (adenomyosis uteri)
- mildly deficient sperm quality
- In vitro fertilization (IVF):
- functional disorders of the fallopian tubes
- mildly deficient semen quality
- endometriosis
- idiopathic sterility (infertility without known cause)
- after hormone treatment and polyfollicular development to prevent multiple pregnancies
- immunological sterility
- functional disorders of the fallopian tubes
- Intracytoplasmatic sperm injection (ICSI):
- severely deficient semen quality
- when fertilization fails in conventional in vitro fertilization
- severely deficient semen quality
Hormone Therapy for Cycle Optimization
Provided that the woman has passable tubes and a partner with acceptable fertility, cycle-optimizing hormone therapy can be the first step (optimizing follicular maturation and supporting the luteal phase). In cases with delayed follicular maturation or luteal weakness but with an intact hypothalamus-hypophysis-ovarian axis, follicular maturation can be stimulated with Clomifen or subcutaneous injection of the gonadotropin FSH (folliclestimulating hormone). Clomifen is an estrogen antagonist that blocks the hypothalamic and hypophysic estrogen receptors without triggering the following signal cascade. This simulates a peripheral estrogen deficiency. The body reacts by increasing the secretion of FSH, which stimulates follicle formation in the ovaries. The success of follicular recruitment and maturation can be evaluated by ultrasound. From a follicle diameter of about 18 mm upwards, administering human chorionic gonadotropin (hCG) will trigger ovulation. This process takes advantage of the fact that human chorionic gonadotropin has a strong LH effect. Especially due to its long half-life, 80% of all ovulations occur 36–48 hours after administering hCG. Shortly before the expected ovulation, the couple should engage in sexual intercourse.
When Clomifen is taken, insufficient proliferation of the endometrium is observed occasionally, due to its estrogen-antagonistic effect. This antiestrogen effect can also change the cervical mucus so that it becomes more difficult for the sperm to pass. The negative effect on the endometrium is regarded as one cause for the low pregnancy rate in Clomifen-stimulated cycles. In addition, it is suspected to thereby cause a higher rate of miscarriage. Therefore, follicular stimulation with gonadotropines (controlled ovarian hyperstimulation) is a commonly used option. Disadvantages are the high costs and the danger of polyovulation (also possible with Clomifen) with increased risk of multiple pregnancies. Because of the higher success rate, gonadotropine stimulation should if possible be combined with intrauterine insemination (IUI).
Intrauterine Insemination
In deficient sperm quality, compatibility disorders, or as the first therapeutic step in unexplained sterility, intrauterine insemination (IUI) is indicated. After ovarian stimulation, prepared sperm are injected with a thin catheter into the fundus of the uterus and both tubes at the ideal point in time. Scientific data proves that especially intrauterine insemination after gonadotropine stimulation increases the chances of pregnancy by four as compared with the approach of simply waiting. Extensive analysis of the records shows, however, that pregnancy rates by means of intrauterine insemination are still disappointingly low with a total of 9–12%. Above the age of 35, they clearly drop even further. It is, however, essential that the indication for insemination is given correctly. Moreover, no more than three to four insemination cycles should be performed since further attempts hardly offer additional chances for a pregnancy. Modified insemination techniques like double insemination in the cycle or intratubal microinsemination do not offer advantages either, since they do not make the method more effective. In combination with hormone treatment, on the other hand, intrauterine insemination also carries the risk of multiple pregnancies. Almost all highgrade multiple pregnancies (triplets and especially quadruplets) come from insemination cycles! One advantage of this treatment strategy that is important in our times is the low costs to insurance companies and patients.
In Vitro Fertilization
For in vitro fertilization (IVF), the woman should ideally be under 40 years of age; in addition, at least one ovary and the uterus have to be functioning properly. The typical IVF procedure looks like this:
In a pretreatment cycle, the follicle cohort ready for stimulation is synchronized by means of a special antibaby pill. Overlapping with this, the so-called down-regulation (long protocol) begins with the desensitization and complete emptying of the pituitary gland, as a result of which it no longer discharges any FSH and LH. This prevents premature ovulation and—for example, in women with hormonal disorders—improves the quality of the maturing egg cells. The retrieval of egg cells (follicle punction) can be planned in a relatively large window for the possible administration of hCG.
A new, additional option for suppressing premature ovulation consists of administering so-called GnRH antagonists, which competitively antagonize the effect of the hypothalamic regulatory hormone of the hypophysis. The specific selection of one or the other stimulation protocol must be reserved for the specialist and clinical experience.
Stimulation aims at bringing several eggs (around 5–20) to maturity. Nowadays, a variety of drugs are administered to stimulate the granulosa cells of the follicles (cells that surround the oocyte). These include:
- highly purified hMG (human menopausal gonadotropin, contains equal parts of FSH, LH, and some hCG)
- genetically produced recombinant FSH and LH
If the follicles have been able to mature long enough (at least 6 days), hCG injection induces ovulation. Of main biological significance is hereby the fact that this signal causes the oocyte to complete its first meiotic division and to halve its chromosome set (expulsion of the so-called polar body). It becomes clear that inducing ovulation and timing are of great significance for the quality of the oocyte and the success of the performed treatment.
After about 35 hours, the egg cells are sucked out of the follicles shortly before spontaneous ovulation in a minor surgery by transvaginal, ultrasound-guided punction (follicle punction). After a short period of incubation in special cell culture mediums, the egg cells are fertilized with the processed semen fluid. The fertilized eggs are first cultured for 16–18 hours and then examined to determine whether fertilization has taken place. But before this, the egg cells must be extricated from the surrounding tissue. At this time, a first quality check of the fertilized eggs (the so-called zygotes) can take place (Fig. 6.8).
Assessments about developmental potential and chromosomal integrity are possible. The most suitable two or at most three fertilized oocytes are cultured for an additional 2–3, sometimes 5 days. Surplus fertilized oocytes in which the nuclei are not yet melted together (syngamy) can be frozen for later cycles. For various reasons, transferring the embryo on day 2–3 has proven to be most favorable. At this point in time, the embryos are in the four- or eight-cell stage (Fig. 6.9). Very carefully, they are then transferred to the lower part of the uterus by means of a thin catheter. The following luteal phase must be supported hormonally (especially with progesterone), otherwise pregnancy is unlikely to occur. A pregnancy test can be performed reliably 11–12 days after the embryo transfer.
A complete IVF cycle from day 1 of the antibaby pill to the pregnancy test hence takes about 6–7 weeks (Table 6.5). The chances of pregnancy are, depending on age, 25–40% per initiated IVF cycle. Data from the German IVF Registry clearly indicates a marked decrease in chances of pregnancy by IVF treatment for women from the age of 35 on. From 40 years on, the chances are only 10–20% of those of a woman between 30 and 35.
Intracytoplasmatic Sperm Injection
The method of intracytoplasmatic sperm injection (ICSI, first introduced in 1992) has revolutionized modern reproductive medicine and has since given a child to many couples who would never have become parents otherwise. This method of microinjecting individual sperm cells into the mature egg cell is an additional measure within the framework of in vitro fertilization. It is indicated particularly in cases when very bad semen quality makes fertilization by means of conventional IVF doubtful. It is also used when a previous IVF resulted in no or only very few fertilizations. All steps—with the exception of inseminating the egg cells—are identical with the conventional IVF procedure. Under a special microscope, a single sperm is drawn up into a thin injection needle by means of micromanipulators and injected directly into the egg cell (Fig. 6.10). But the egg cell must previously have been extricated from the surrounding tissue (cumulus cells).

Fig. 6.8 Pronucleus stage. Sixteen hours after insemination and removal from the surrounding granulosa cells.