Femur Fractures: Antegrade Intramedullary Nailing
Bruce D. Browner
Andrew E. Caputo
Augustus D. Mazzocca
Donald A. Wiss
Indications/Contraindication
Intramedullary nailing is the treatment of choice for all diaphyseal femoral fractures in adults. Locked intramedullary nailing can be static and dynamic. Static locking involves placement of proximal and distal locking screws, which prevent malrotation and shortening. Dynamic nailing is done with locking screws placed on either the proximal or distal side of the fracture. Because static interlocking does not inhibit fracture healing, all diaphyseal femoral fractures should be statically locked. Occasionally, dynamic locking is indicated for short oblique or transverse mid-diaphyseal fractures without comminution.
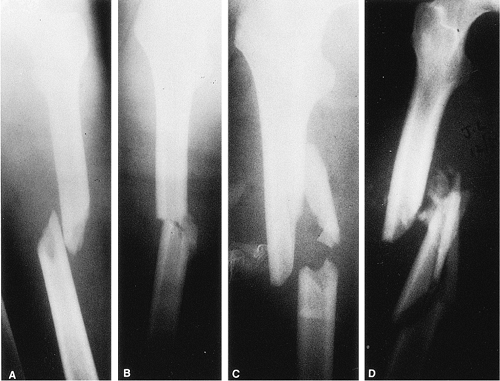
Many classification systems have been described for femur fractures. Winquist and Hansen developed a classification based on the amount of comminution (Fig. 21.1). Type I and II fractures are characterized by stable bone contact between the proximal and distal fragments and are considered length stable. Type III and IV comminution results in limited or no contact between the proximal and distal fragments, and static interlocking is required to maintain correct limb length and rotation.
Indications for intramedullary nailing of the femur include simple or comminuted fractures presenting below the lesser trochanter and extending distally to within 7 cm of the knee. Most grade I and II open femoral-shaft fractures can be treated with reamed intramedullary nails. Isolated grade III fractures may be better treated with aggressive wound management, temporary external fixation, and delayed intramedullary fixation. Patients with multiple injuries, including open femur fractures, require early skeletal stabilization to prevent pulmonary compromise. In these circumstances, a nonreamed intramedullary nailing or external fixation may be biologically attractive. However, the mechanical benefits of reaming with insertion of a larger nail, which provides more stability and strength, are sacrificed.
Contraindications to intramedullary nailing include active local or systemic infections. Antegrade nailing in adolescents with open growth plates can damage the blood supply to the femoral head, causing osteonecrosis. These fractures may be better treated through use of flexible intramedullary nails, which are inserted retrograde proximal to the distal femoral-growth plate. Due to a higher incidence of infection when reamed nailing is performed after a prolonged period of initial external fixation, nailing should be used with caution. Other contraindications to nailing include patients with very narrow medullary canals or those with preexisting deformities that would preclude closed nailing.
Preoperative Planning
All patients with femur fractures resulting from blunt trauma should be evaluated for other injuries. Trauma evaluation and resuscitation via a multidisciplinary approach is necessary in patients with multiple injuries. High-quality, full-length anteroposterior (AP) and lateral radiographs of the femur should be obtained to evaluate the fracture (Fig. 21.2). The fracture location and the degree of comminution should be assessed on plain films. Ipsilateral fractures of the hip or femoral condyles must be ruled out before nailing is undertaken. Specific hip or knee films are often necessary for visualizing these fractures. Unrecognized nondisplaced fractures in these areas may displace during nailing. Once recognized, these fractures may be amenable to fixation with percutaneous screws. Osteoarthritis of the hip joint with a flexion contracture may limit hip motion on the traction table and make nailing difficult when the patient is in the supine position. When severe comminution or segmental defects exist, full-length films of the opposite femur may be helpful in determining appropriate length.
Contralateral radiographs also may be used to assess the medullary canal diameter and the degree of curvature of the intact femur. Patients with extremely small intramedullary canals
may require specially sized implants; the size should be determined preoperatively to ensure implant availability. The remodeling process associated with aging and osteoporosis often leads to an increase in the diameter of the medullary canal. In these patients, insertion of very-large-diameter nails is not necessary because stability is better achieved with 12- to 14-mm nails that are statically locked. The increased stiffness of large-diameter nails can cause iatrogenic comminution during insertion into brittle osteoporotic bone. Also, the curve of the implant must match the curve of the femur.
may require specially sized implants; the size should be determined preoperatively to ensure implant availability. The remodeling process associated with aging and osteoporosis often leads to an increase in the diameter of the medullary canal. In these patients, insertion of very-large-diameter nails is not necessary because stability is better achieved with 12- to 14-mm nails that are statically locked. The increased stiffness of large-diameter nails can cause iatrogenic comminution during insertion into brittle osteoporotic bone. Also, the curve of the implant must match the curve of the femur.
 Figure 21.2. AP radiograph of the right femur showing a transverse mid-diaphyseal fracture with minimal comminution. |
Reestablishing the correct limb length and choosing the nail of appropriate length requires a reference length. We use the distance between the tip of the greater trochanter and the adductor tubercle to determine length. A radiograph of the intact femur with a radiopaque ruler placed along the thigh (Fig. 21.3) should be obtained.
Surgery
Patient Positioning
Nailing can be performed with the patient in the lateral decubitus (Fig. 21.4) or supine position (Fig. 21.5) with or without a fracture table. The lateral decubitus position allows improved access to the piriformis fossa, especially in large patients or those with ipsilateral hip disease and concomitant decreased range of motion. However, patients with multiple injuries who are placed in the lateral position may experience respiratory compromise. In addition, valgus angulation of the fracture, difficulty determining proper rotation, venous congestion caused by pressure of the perineal post, and greater difficulty inserting distal locking screws are disadvantages to lateral positioning.
Supine positioning of the patient has advantages: ease of setup, less respiratory compromise, better fracture alignment, and easier distal-screw insertion. However, the surgeon will have greater difficulty establishing the correct starting point in the piriformis fossa. With the recent introduction of trochanteric entry nails, this determination has become less of a problem.
In the classic procedure, intramedullary nailing is done on a fracture table through which fracture reduction is achieved via sustained longitudinal traction with or without a skeletal pin. A perineal post provides a fulcrum against which traction is applied. The design of most fracture tables allows circumferential access to the extremity for manipulation, surgical exposure, and imaging. The decision to use either a fracture table or a radiolucent table in patients who have experienced multiple traumas and who require simultaneous or sequential surgical procedures should be made on a case-by-case basis.
In an alternative approach, intramedullary nailing can be performed on a radiolucent table. Traction can be applied manually or with the use of a femoral distractor. Nailing can be performed through an antegrade or retrograde approach. The technique works best when nailing is done less than 24 hours after injury. Set up time is minimal, and access to the proximal femur is improved by adducting the limb. Disadvantages with this technique include difficulty visualizing the hip and proximal femur in the lateral projection, difficulty reducing and holding the fracture alignment, risk to the femoral neurovascular structures, and blockage of the operative field by the femoral distractor (Fig. 21.6).
Closed Reduction
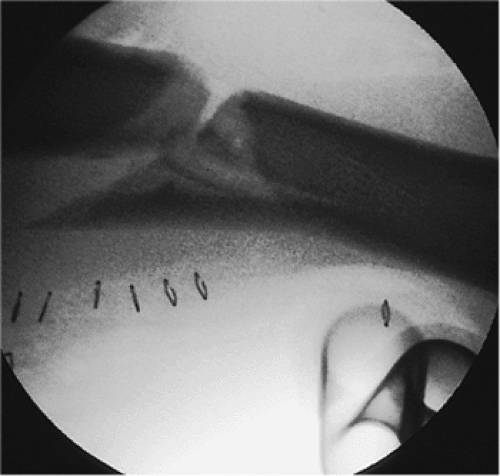
Closed reduction is performed via traction through the fracture table and external manipulation. An in-line boot or a proximal-tibial or distal-femoral pin traction is utilized, and
the fracture alignment is checked with the image intensifier (Fig. 21.7). Occasionally leg manipulation by the surgeon or a crutch may be useful for reduction of an angulated fracture (Figs. 21.8 and 21.9). To minimize the risk of a pudendal nerve palsy, the traction is decreased during the prep, drape, and proximal exposure. Frequently a small-diameter nail may be used in the proximal fragment to reduce a flexed and externally rotated proximal
fragment. In addition, most implant manufacturers include a small-diameter intramedullary manipulation rod in the nailing sets for this purpose.
the fracture alignment is checked with the image intensifier (Fig. 21.7). Occasionally leg manipulation by the surgeon or a crutch may be useful for reduction of an angulated fracture (Figs. 21.8 and 21.9). To minimize the risk of a pudendal nerve palsy, the traction is decreased during the prep, drape, and proximal exposure. Frequently a small-diameter nail may be used in the proximal fragment to reduce a flexed and externally rotated proximal
fragment. In addition, most implant manufacturers include a small-diameter intramedullary manipulation rod in the nailing sets for this purpose.
 Figure 21.7. Fracture alignment. Once the patient is positioned on the fracture table, the distal fragment is posteriorly displaced. |
Entry Point
To facilitate supine nailing, most implant manufacturers have developed nails designed to enter through the tip of the greater trochanter. While technically easier to use than the classic piriformis entry nails, concerns exist about compromise of the hip abductor mechanism in patients undergoing trochanteric-entry nailing. To date, no long-term outcome studies have been completed on hip function following trochanteric nailing. We are hesitant to recommend its routine use, particularly in young trauma patients, until evidence-based medical studies support its widespread use. For this reason, we still advocate the use of a piriformis entry point for the majority of antegrade nailing procedures.
For a piriformis nailing, the entry point is critical for proper nail placement and fracture reduction. A longitudinal incision 6 to 10 cm is made over the greater trochanter and in-line with the femur (Fig. 21.10). The fascia overlying the abductors is incised, and the muscle is split in-line with its fibers down to the piriformis fossa (Fig. 21.11). A guide pin is placed in the piriformis fossa, and its position is confirmed with fluoroscopy. The tip should be centered directly in-line with the medullary canal as seen in both the AP and lateral views. Medial portal placement should be avoided because it may cause a femoral-neck fracture. Portal placement laterally may lead to comminution and varus alignment in proximal fractures. Once the pin is properly positioned in the piriformis fossa and is confirmed fluoroscopically, the femur is opened with a cannulated drill. In an alternative, an awl may be placed in the piriformis fossa and the proximal femur opened by hand (Figs. 21.12,21.13,21.14,21.15,21.16,21.17,21.17,21.18,21.19,21.20)
Guide-Wire Insertion, Fracture Reduction, and Reaming
A flexible ball-tipped guide wire is placed down the canal under fluoroscopic control. A ball tip is essential to prevent complications while reaming. The distal 2 cm of the tip is typically bent and used to direct the wire into the displaced distal fragment. The guide wire should be placed centrally in the distal fragment because eccentric placement may cause
comminution or mal-alignment (Figs. 21.21,21.22,21.23,21.24,21.25,21.26,21.27,21.28,21.29,21.30,21.31,21.32



comminution or mal-alignment (Figs. 21.21,21.22,21.23,21.24,21.25,21.26,21.27,21.28,21.29,21.30,21.31,21.32
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree