Chapter 9 Femoral Varus Osteotomy
Introduction
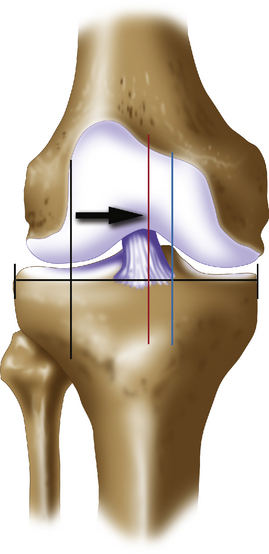
The valgus knee (Figure 9–1) is usually secondary to hypoplasia of the lateral femoral condyle resulting in a superior lateral directed joint line. Corrective osteotomy is most appropriately performed at the level of the deformity to restore a joint line that will be parallel to the floor. For this reason, correction of valgus malalignment is performed through the femur. As in tibial corrective osteotomies, osteotomies may be closing wedge, opening wedge, or reverse dome. Each has advantages and disadvantages. The clinical outcomes following femoral osteotomies parallel those of tibial osteotomies; however, femoral osteotomies are much less common, as is the literature on them.1,2 One possible reason is that the disease pattern frequently involves the patellofemoral joint when the knee is in valgus, and correction of both arthritic conditions is technically more demanding and less predictable.
Indications
The supracondylar reverse dome osteotomy remains a powerful osteotomy for large angular corrections and is my choice for corrections greater than 15 degrees.3 It requires the use of an angled blade plate to obtain stable fixation or use of another fixed-angle device.
Planning
The goal of femoral osteotomy correction is similar to that of tibial valgus-producing osteotomy. If weight-bearing x-ray films demonstrate intact joint spaces and valgus malalignment is present with mechanical axis forces through the lateral compartment, then correction of the mechanical axis is made to the midline if an articular cartilage defect is being unloaded (Figure 9–2). This normalizes the forces across the joint. If joint space narrowing is present or a large articular cartilage defect is undergoing repair, then the aim is to unload the lateral compartment by only 2 degrees, which corresponds to the medial tibial spine. In this way, premature wear of the medial compartment is less likely.
Long alignment x-ray films in a double-stance anteroposterior phase are required for calculating angular correction (Figures 9–3 and 9–4). A line from the center of the femoral head is projected to the desired mechanical axis of either the center of the knee or the medial tibial spine to the proposed position of the foot. An angular correction then goes from the existing center of the ankle to the proposed mechanical axis point at the knee and then to the new ankle position. This acute angle is the angular correction. This angular correction is converted to opening or closing millimeters using digital x-ray templates to plan for an opening wedge osteotomy on the lateral side of the distal femur or a closing wedge osteotomy on the medial side of the femur above the adductor tubercle and trochlea. This angle also allows planning for placement of a chisel for use of an angled blade plate relative to the tibial femoral joint line (see Figure 9–4).
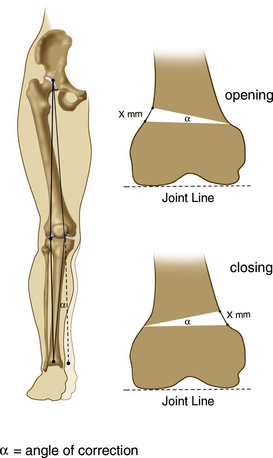
Figure 9–3 The angle of correction for a varus-producing femoral osteotomy is measured on a long alignment x-ray film. The angle from the existing center of the ankle to the proposed mechanical axis at the knee (see Figure 9–2) and back to the new position of the ankle represents the angular correction. This angle is applied to the level of the opening or closing wedge osteotomy on the distal femoral metaphyseal–diaphyseal junction. The measurements in millimeters, x, is the correct opening or closing osteotomy. Opening wedge systems generally have spacer plates in millimeters that correspond to the preoperative planning. Closing wedge systems usually have angular increments on the osteotomy jigs that accurately measure in degrees the angular correction. Digitized x-ray systems with built-in software, calibrated for magnification error, make the planning very straightforward (General Electric web-based Centricity software [GE Healthcare, Waukesha, WI]).
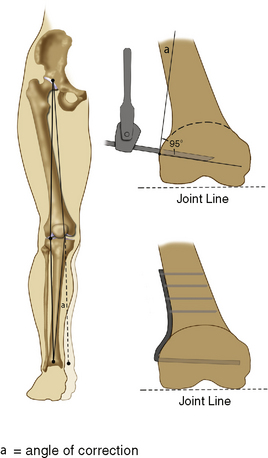
Figure 9–4 The angular correction is calculated and identical to obtained in Figure 9–3. A 95-degree blade plate is used for fixation of a supracondylar reverse dome varus femoral osteotomy, although other fixed-angle devices, such as a locking plate, may be used. The corrective angle α is measured from the lateral cortex of the femur to the intersection of the proposed position of the 95-degree angled blade plate. Generally, angled metallic triangles that have the angle α are placed along the plate portion of the angled blade plate. This allows placement of a guidewire along the plane of the entry blade. The seating chisel then passes along the guidewire prior to the supracondylar femoral dome osteotomy. Once the osteotomy is completed, the 95-degree blade plate is placed along the tract of the seating chisel, and the alignment of the leg is corrected with a varus force until the plate portion fits flush to the lateral femoral cortex. An articulated compression device is applied, the osteotomy site is compressed, and screw fixation completes the stabilization of the osteotomy.
Opening wedge varus femoral osteotomy
Technique and Aftercare
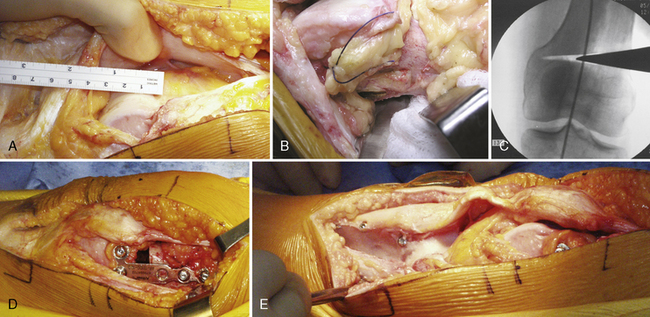
An opening wedge femoral varus-producing osteotomy is performed through a midline incision. Figure 9–5 shows an appropriate case example, and Figure 9–6 outlines the surgery in stepwise fashion. The deep exposure can be performed through a lateral subvastus approach to approach the lateral distal femur for an extraarticular surgery. The lateral subvastus approach can be combined with a tibial tubercle osteotomy to expose the entire distal femur and joint without a muscle split. I usually use a lateral parapatellar arthrotomy to expose the distal lateral femur as well as the patellofemoral articulation.
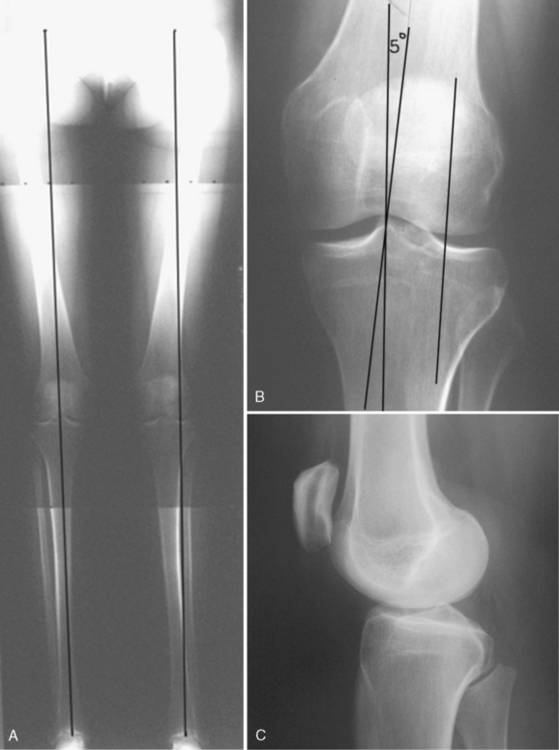
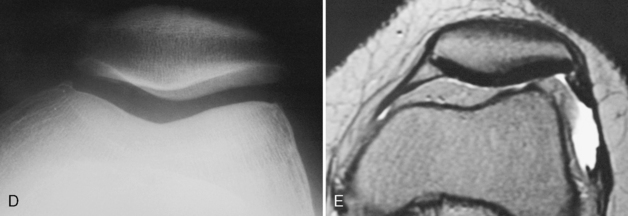
Figure 9–5 A, Long alignment x-ray films of a 6-foot 1-inch, 23-year-old woman who has experienced disabling anterior and lateral knee pain for 9 months. Her clinical appearance shows that she has valgus malalignment to her left leg with equal leg lengths, patellofemoral lateral maltracking with subluxation and tilt of the patella, and a positive J-sign as she flexes her knee from a fully extended position. She has a positive patellar compression test, mild crepitus, lateral joint line tenderness, and a stable knee to collateral and anteroposterior testing. B, Mechanical axis to the left knee falls through the center of the lateral tibiofemoral compartment. A 5-degree angular correction is required to place her mechanical axis to the medial tibial spine. C, D, Lateral and skyline x-ray films demonstrate mild patella alta with a well-centered patella on a 45-degree tangential skyline x-ray film with intact joint spaces. E, Corresponding axial magnetic resonance scan demonstrates intact articular surfaces to the patella and trochlea with lateral patella subluxation. A combined varus femoral osteotomy in addition to anteromedialization of the tibial tubercle (see Figure 9–6) is planned to unload and normalize the joint forces and thereby alleviate the patient’s symptoms.