Femoral Neck Fractures: Arthroplasty
Jeffrey O. Anglen
Fractures of the hip occur in two distinct anatomic locations in the proximal femur. Intertrochanteric (or pertrochanteric) fractures involve the area of the bone that is mostly or entirely outside the hip joint capsule, where the soft-tissue attachments provide good blood supply for healing and for ligamentotaxis. Fractures of the femoral neck occur through bone inside the capsule, where sparse soft-tissue attachments and the synovial fluid environment make healing slower and less reliable. Intertrochanteric fractures are routinely and successfully treated with reduction and internal fixation, and nondisplaced or impacted femoral-neck fractures are reliably handled with fixation in situ. However, the treatment of displaced femoral-neck fractures involves several controversies.
The first controversy regards whether to reduce and fix the fracture or to excise and replace the femoral head. Reduction and fixation of a displaced femoral-neck fracture is a technically demanding surgical procedure. It allows the patient to retain his/her own femoral head, and thereby avoid problems specific to prosthetic replacement such as dislocation, loosening, wear, or breakage, which may necessitate revision surgery. This has led some authors to propose an age-based protocol: younger patients (<50 years) are treated with reduction and fixation, elderly patients (>70 years) get arthroplasty, and those in between get individualized decisions based on general health, activity level, and bone quality (1). A wide range of implant failure, displacement, and re-operation rates for internal fixation have been reported in the literature (2,3). A meta-analysis of 13 studies in the Cochrane database concluded that internal fixation was associated with less operative trauma than replacement (decreased operative time, blood loss, transfusion, and infection) but a higher need for re-operation. No clear differences in hospital stay, mortality, or functional outcome were found (4). A more recent meta-analysis of 14 studies showed that those treated with arthroplasty had a significantly reduced risk of re-operation, blood loss, long operative times, and infection. However, this study, in contradistinction to the previous review, found that patients who had received arthroplasty had a slightly higher early-mortality rate than those who were treated with fixation (5). A study using cost-analysis methodology
suggested that arthroplasty was the most cost-effective treatment when complications, mortality, and re-operation rate are evaluated at 2 years postoperation, but the best functional results are achieved with a healed femoral neck that does not have concomitant osteonecrosis (6).
suggested that arthroplasty was the most cost-effective treatment when complications, mortality, and re-operation rate are evaluated at 2 years postoperation, but the best functional results are achieved with a healed femoral neck that does not have concomitant osteonecrosis (6).
There are different options with regard to the type of arthroplasty to be performed for femoral neck fracture. Total hip replacement (THR) can be performed for patients with acetabular damage, preexisting degenerative arthritis, or a systemic arthritic disease such as rheumatoid arthritis. Although some authors (7,8,9) have suggested that THR has better functional results with lower complications than hemi-arthroplasty, others have found that THR after acute fracture has significantly poorer outcomes, in terms of dislocation and revision rates, than primary THR (5,10,11). Those reports are retrospective, uncontrolled, and based on few cases. Two, prospective, randomized studies have compared THR with hemi-arthroplasty, and showed conflicting results. One study (12) revealed no difference between the two procedures, while the other (13) suggested that THR had a lower revision rate and higher hip scores. The study showing differences in acetabular replacement also demonstrated differences in stem fixation between the two groups.
Hemi-arthroplasty can be performed with either a modular unipolar or bipolar endoprosthesis. The bipolar design was developed to reduce metal on cartilage motion and friction, and thereby decrease acetabular wear and erosion, a postulated cause of postoperative pain. At the same time as the bipolar head design, modern modular-stem designs were introduced, complicating analysis. Several studies have shown good results for bipolar endoprostheses, particularly when they were cemented in place (14,15,16). However, cadaveric and radiographic studies revealed that motion occurs primarily at the outer bearing, particularly when the prosthesis is loaded (as in walking), reducing the likelihood for protection of the acetabular cartilage (17,18). In addition, multiple-prospective comparison studies have failed to show any significant difference in outcome between the bipolar and the unipolar designs (2,19,20,21,22). A prospective study reporting outcomes of 270 patients found significantly higher hospitalization costs (30%) for patients receiving a bipolar prosthesis compared to those receiving a unipolar implant (23). The type of implant was chosen by the surgeon, and there were some differences in the two patient populations.
A large number of hip arthroplasty systems are commercially available in the United States, and many offer hemi-arthroplasty components. Femoral stems come in many designs, made of a variety of different metals, and with a variety of surfaces and coating. Many of these stems are substantially more expensive than the basic Austin-Moore (fenestrated) or Thompson (nonfenestrated) design that has been in use for decades, and none has been proven superior.
Another controversy concerns the use of cement fixation for the stem. While operation without cement is faster, avoids the cardiovascular morbidity related to methylmethacrylate, and may make subsequent revision of the stem (if needed) easier, stability is decreased and the patient is slower in returning to activity. A retrospective study of 451 cases comparing the Bateman bipolar prosthesis inserted with or without cement found less thigh pain (13% vs. 46%) and higher Harris hip scores (86% vs. 79%) in the cemented group, with no difference in mortality (16). In a prospective, randomized, trial in which bipolar heads were used, the group whose hips were not cemented had significantly more pain and need for walking aids (24). A recent analysis of 18 published studies found that the use of cement resulted in longer operative times and more blood loss, but better postoperative mobility and less pain; no differences in mortality or general complications were found (25). Sixteen of the 18 studies reviewed concluded that cement should be used routinely, and the authors of the review agreed. A meta-analysis in the Cochrane Library found that there was “limited” evidence that cementing the stem of a hemi-arthroplasty would lead to less pain and improved mobility, but concluded that the data was insufficient to determine whether that advantage was offset by other disadvantages of cementing, such as increased mortality (20). If the stem is inserted without cement, use of an intramedullary corticocancellous bone plug, prepared for the head of the femur, may decrease the rate of subsidence and subsequent thigh pain (26).
Indications
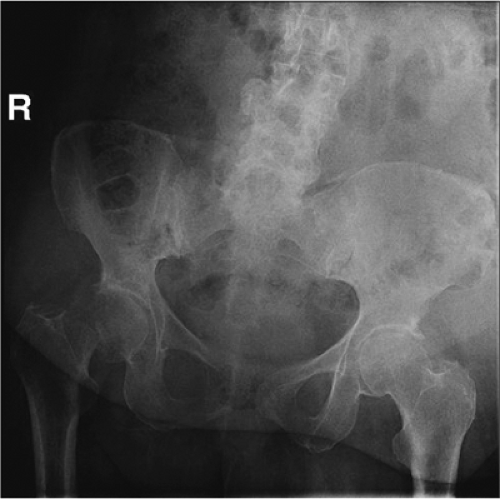
Hemi-arthroplasty is indicated for displaced femoral-neck fractures in physiologically older adult patients (some have suggested approximately 70 years of age), or in younger patients with limited life span due to systemic disease, impaired ability to heal fractures, or irreparably damaged femoral heads (Fig. 15.1). Nondisplaced or impacted fractures are better treated with fixation in situ using cannulated screws. Fractures with preexisting arthritic changes or insufficient acetabular structure should be treated with total hip arthroplasty. Fractures in moribund, severely demented, or nonambulatory patients with limited life expectancy may be treated nonoperatively with analgesia.
Preoperative Planning
Patient evaluation includes a thorough history and physical exam, which may be difficult in many elderly, debilitated patients. The circumstances surrounding the fall should be elicited, seeking evidence of a syncopal episode, medication error, or exacerbation of a chronic medical condition that would require further workup. Evidence of an unsafe environment or elder abuse may require social work evaluation. A complete medical history and review of systems may reveal information that impacts the timing of surgery or the choice of anesthetic technique. On physical examination, the injured leg is typically shortened, externally rotated and painful with motion. The examination should include evaluation for other typical insufficiency fractures, such as the distal radius, pelvis, or spine and for fall-associated traumatic conditions such as subdural hematoma. The involvement of a medical consultant, particularly one who knows the patient, is useful. Laboratory studies should include a complete blood count, analysis of serum electrolytes, a blood sample for type and cross match, chest radiograph, and electrocardiogram.
Adequate anteroposterior (AP) radiographs of the hip and proximal femur are necessary to plan for the procedure. Lateral films are difficult to obtain due to patient discomfort and are often of poor quality. Obesity and osteopenia frequently combine to thwart adequate
visualization, and repeat films with less penetration may be helpful. Traction and/or rotation films may be helpful to evaluate the fracture line, although traction and internal rotation may restore the position of the femur and make the orientation look normal. Sizing templates for the prosthetic system can be used to estimate the size of the prosthesis necessary. Particular attention should be paid to the level of the neck cut and the size of the femoral head because length discrepancies and size mismatch are associated with poor outcomes (27).
visualization, and repeat films with less penetration may be helpful. Traction and/or rotation films may be helpful to evaluate the fracture line, although traction and internal rotation may restore the position of the femur and make the orientation look normal. Sizing templates for the prosthetic system can be used to estimate the size of the prosthesis necessary. Particular attention should be paid to the level of the neck cut and the size of the femoral head because length discrepancies and size mismatch are associated with poor outcomes (27).
Operative Procedure
The procedure can be performed under general or spinal anesthesia. Regional technique may offer less risk of some anesthetic complications, but several large retrospective, nonrandomized studies of hip fracture surgery have failed to show any difference in mortality, morbidity, or functional outcome (28,29,30,31).
Preoperative intravenous antibiotics are given at least 30 minutes, but less than 120 minutes, prior to incision. Usually 2 g of a broad spectrum cephalosporin (e.g., cefazolin) are given, unless the patient is allergic or there is another specific reason to give a different drug.
The operation can be performed through anterior, lateral, or posterior approaches to the hip. One study of relatively poor methodological quality compared anterior to posterior approaches and found (for unexplained reasons) significantly increased mortality in the posterior group (32), and some older studies suggested a higher dislocation rate with posterior approach (33,34). More recent meta-analysis for comparison of lateral and posterior approaches for total hip arthroplasty has yielded no major differences in function or complication rates (35). The surgeon should use the surgical approach with which she/he feels most comfortable.
For the posterior approach to the hip, the patient is placed in the lateral decubitus position after induction of anesthetic. Padding is placed on all bony prominences (Fig. 15.2). A bean bag is used to maintain position, and the down-side arm is placed out in front of the body. An axillary roll may be used. The down-side leg is padded and secured to the bed with straps or tape. The chest may be secured in like fashion, but care should be taken not to make the chest strap too tight. Efforts are made to orient the pelvis directly lateral.
The hip and leg is scrubbed and painted with antiseptic circumferentially from above the iliac crest to the toes, and the draping is applied to allow adequate exposure posteriorly and proximally. The leg is covered with a stockinette to the mid thigh and secured with Coban (Fig. 15.3).
The incision is marked on the skin and then adherent antiseptic-impregnated plastic drapes may be applied to cover the exposed skin completely, including the medial thigh and groin.
The incision is marked on the skin and then adherent antiseptic-impregnated plastic drapes may be applied to cover the exposed skin completely, including the medial thigh and groin.
 Figure 15.2. The patient is positioned in the lateral decubitis position on a bean bag with care taken to pad all boney prominences. A pillow is placed between the arms and the legs. |
 Figure 15.3. The entire leg and hip are draped free, as shown in this image from a patient other than the one in Figure 15.1. A stockinette is used to the mid thigh. |
 Figure 15.4. The position used by the assistant to support the leg and retract the tissues. It is important to be careful not to contaminate the patient’s leg against the assistant’s face or mask. |
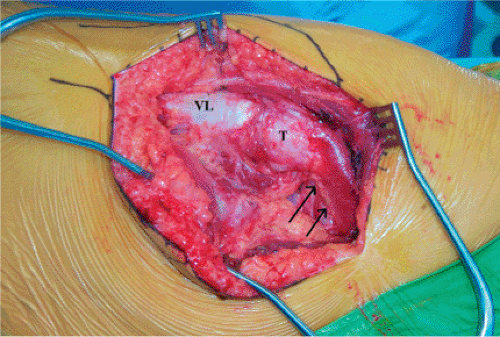
The surgeon stands behind the patient while the assistant stands on the opposite side. This allows the assistant to keep his/her hands free while supporting the leg with the hip extended, knee flexed, and the femur externally rotated (Fig. 15.4). The incision is centered on the greater trochanter and extends distally along the lateral aspect of the femur for approximately 10 cm. Proximally the incision extends approximately 45 degrees toward the posterior, superior, iliac spine for approximately 10 cm (Fig. 15.5). With an obese patient, larger incisions will be necessary. The subcutaneous tissue is divided in line with the incision, and hemostasis is accomplished with electrocautery. The fascial level is identified and opened sharply with knife or Bovie, and the incision is extended distally in the fascia posterior to the iliotibial band and proximally, splitting the gluteus fascia and muscle bluntly. The trochanter is exposed (Fig. 15.6).
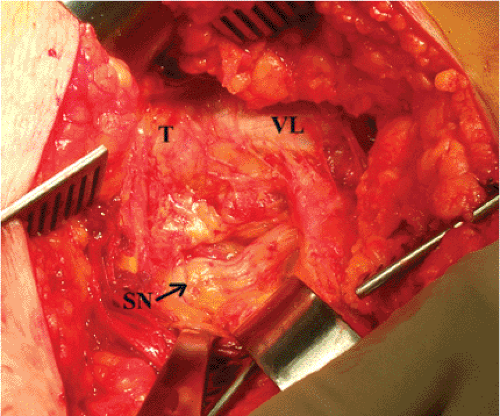
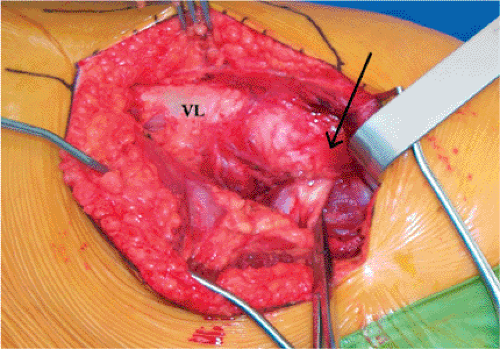
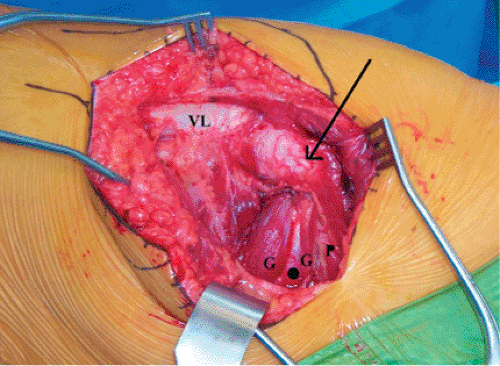
The sciatic nerve is palpated posterior to the quadratus femoris and its position clearly noted (Fig. 15.7). Awareness of the nerve position is maintained throughout the operation, and it is protected from tension by extension of the hip and flexion of the knee. The piriformis tendon is identified by palpation posterior to and underneath the edge of the gluteus medius, which is attached to the trochanter (Figs. 15.8 and 15.9). The tendon is separated from the underlying capsule by gentle spreading the right angled clamp and by passing a soft tissue elevator between the short rotators and the capsule surface (Fig. 15.10). A tag suture is passed through the tendon approximately 1.0 cm from its insertion and looped around the tendon to grasp it. The tendon is divided with the Bovie near the insertion. As an alternative, and to increase postoperative hip stability, the tendon can be retracted and attempts made to preserve it throughout the procedure (36). The conjoined tendon of the obturator internus
and the gemelli muscles (see Fig. 15.9) is identified in like fashion, tagged, and divided. Note that this tendon is frequently on the undersurface of the musculature and must be located by palpation rather than by direct vision. When these two tendons are reflected, the sciatic nerve usually passes behind the conjoined tendon and attached muscles, and is in front of the piriformis tendon/muscle. However, there is substantial variation among patients and one must be on the lookout for a split sciatic nerve on either side of either tendon.
and the gemelli muscles (see Fig. 15.9) is identified in like fashion, tagged, and divided. Note that this tendon is frequently on the undersurface of the musculature and must be located by palpation rather than by direct vision. When these two tendons are reflected, the sciatic nerve usually passes behind the conjoined tendon and attached muscles, and is in front of the piriformis tendon/muscle. However, there is substantial variation among patients and one must be on the lookout for a split sciatic nerve on either side of either tendon.
 Get Clinical Tree app for offline access 
|