CHAPTER 24 Failure Modes of Unicompartmental Arthroplasty
 Unicompartmental arthroplasty is a common surgical procedure in the patient with unicompartmental disease.
Unicompartmental arthroplasty is a common surgical procedure in the patient with unicompartmental disease. Midterm and long-term survivorship of unicompartmental arthroplasty is highly variable, and multiple factors contribute to failed procedures.
Midterm and long-term survivorship of unicompartmental arthroplasty is highly variable, and multiple factors contribute to failed procedures.Introduction
Unicompartmental knee arthroplasty (UKA) has become a common surgical procedure for unicompartmental osteoarthritis both nationally and internationally in the middle-aged and older patient. Midterm and long-term survivorship of UKA is highly variable. From 1998 to 2005, the incidence of performance of UKA increased at a rate of 32.5% compared to an increase in the performance of total knee arthroplasty of 9.4% during the same period.1 In the past 30 years, multiple authors have reported on the indications and contraindications for UKA.2–23
Indications
The classic indications for UKA include:
The “one-finger test” has been reported as a useful indicator as to the location of the pain correlative with the patient’s radiographs exhibiting single-compartment osteoarthritis.3
Contraindications
Contraindications have included:
Operating on patients who exhibit contraindications can result in reduced survivorship of UKA.2,3
Etiology of Failures
Furthermore, failures of UKA can occur as a result of:
Some designs that are no longer utilized exhibited exceedingly high failure rates as a result of component design and polyethylene failure.24,25 Furthermore, using all-polyethylene tibial (APT) components in elderly patients with increased posterior tibial slope and removal of significant amounts of tibial bone have resulted in increased medial tibial collapse with subsidence of the tibial component in some patients.26 Despite recent articles indicating that metal backing reduces strains across the cement-bone interface,27 the longest published survivorship has utilized APT components with specific undersurface macrostructure on both the inferior portion of the APT component and its eccentric post. However, it has been emphasized that minimal tibial bone was removed in those cases that exhibited the longest survivorship.19,28
 The Importance of Surgical Technique (see Video 24-1)
The Importance of Surgical Technique (see Video 24-1)
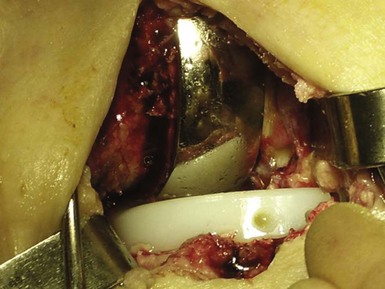
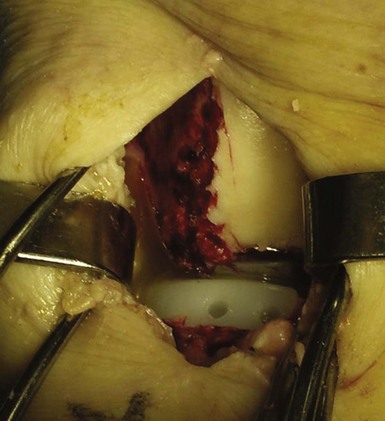
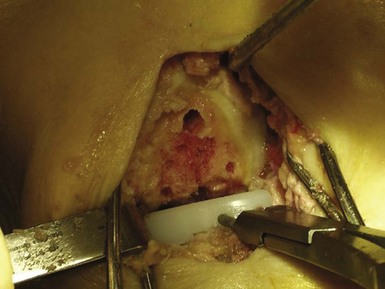
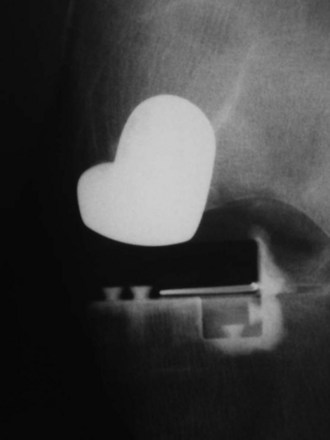
Surgical technique is critical when performing UKA, and accounts for failures regardless of the prosthesis utilized. Surgical recommendations include lateralization of the femoral component when doing medial UKA to account for external rotation during extension of the knee (Fig. 24–1). When using an all-polyethylene component, it is important to implant the widest tibial component possible from the medial tibial cortex to the anterior cruciate ligament, resting on the medial tibial cortex (Fig. 24–2). Using a Steinmann pin through the intercondylar notch to retract the patella and facilitate exposure is helpful. Appropriate cement technique is critical and involves drilling, using pulse lavage, and drying the surfaces prior to applying the cement (Fig. 24–3). The cement should be applied in its doughy stage as well.29 This allows for improved fixation of both the femoral and tibial components.30 When choosing APT components, laboratory studies have confirmed that a dovetail undersurface macrostructure of the tibial component provides the greatest resistance to lift-off and shear stresses (Fig. 24–4). Waffle undersurface patterns tend to result in the worst resistance to lift-off and shear stress application.31,32
Complications of Surgical Technique
It is critical to avoid removal of too much tibial bone in order to prevent fracture and/or subsidence of the tibial component. Fractures have been reported (Figs. 24–5 and 24–6) through the tibial pin sites, resulting in difficult revision scenarios.33–35 Early medial collapse has been reported with significant medial bone removal, and an 11% rate of subsidence of the medially placed APT components has been reported with 2.5-year follow-ups. Upon radiographic review of these patients, the tibial component lacked peripheral support and there was significant bone removal.26 As originally reported by Bloebaum et al.,36 the majority of the proximal tibia, when resecting approximately 6–11 mm below the articular surface, is highly porous cancellous bone consisting predominantly of air. When viewing these resected specimens through the electron microscope, it is apparent that up to 80% of the proximal tibia is cancellous bone at these levels, as demonstrated by polarized (Fig. 24–7A) and nonpolarized (Fig. 24–7B) electron microscopic views of the proximal tibia.36 Furthermore, the posteromedial and posterolateral aspects of the resected proximal tibia have up to 20% more bone than the remainder of the articular surface. This observation would clearly explain why fixation can be an issue and subsidence may occur, especially anteromedially and anterolaterally, if too much tibial bone is resected or an undersized tibial component is placed without medial tibial cortex contact and support.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree