Extensor Tendon Repair
Introduction
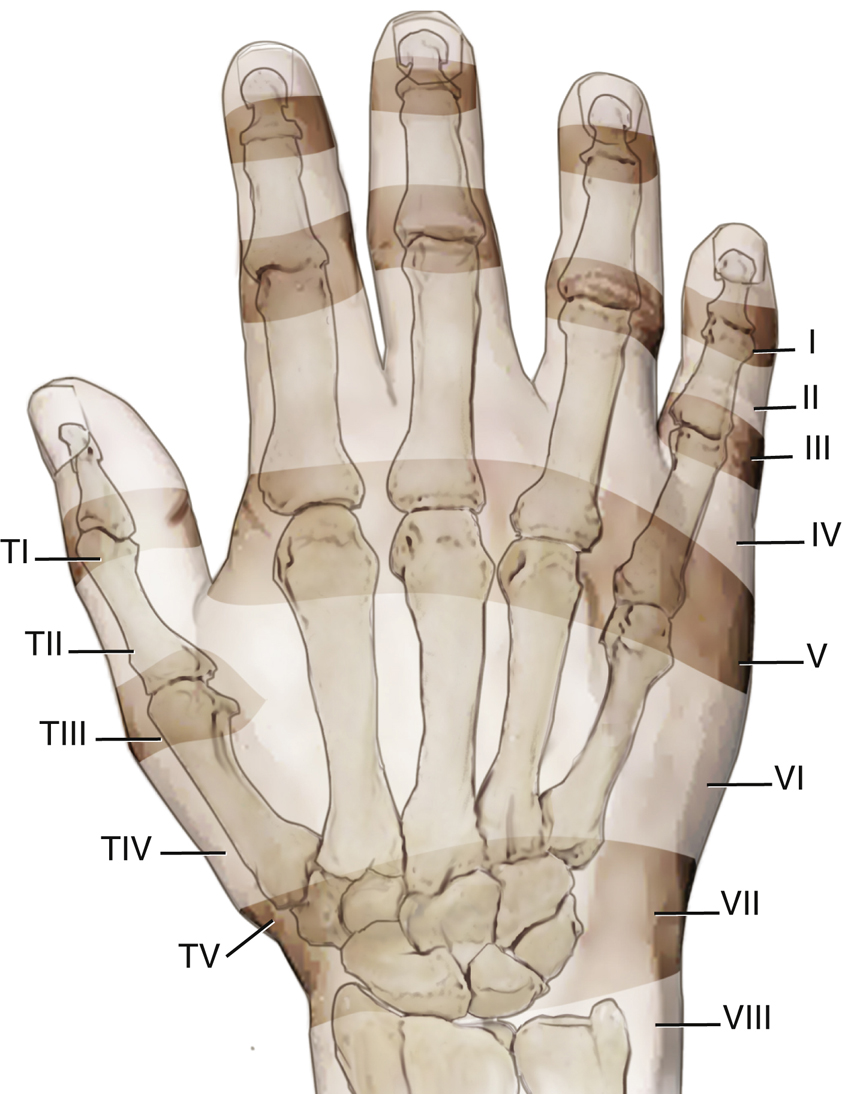
Figure 1Illustration of the eight extensor tendon zones. T = thumb.
(Reproduced with permission from Hunt TR, Wiesel SW : Operative Techniques in Hand, Wrist, and Forearm Surgery, ed 1. Philadelphia, PA, Wolters Kluwer Health, 2010.)
Extensor tendon injuries are more common than flexor tendon injuries because of the subcutaneous location and the vulnerability of the hand to penetrating trauma
Extrinsic system originates proximal at the elbow or forearm and tendons cross the dorsal wrist through six fibro-osseous tunnels which hold the tendons in close apposition to the radius
Extensor tendon injuries classified into eight zones by Kleinert and Verdan
Odd numbers describe injuries at the joint level beginning with zone 1 at the DIP joint
Thumb extensor injuries are similarly classified into five zones (Figure 1)
Patient Selection
Contraindications
Closed extensor tendon injury amenable to splint treatment
Extensive comorbid conditions or neurologic dysfunction
Preoperative Imaging
Plain radiographs to assess bony avulsion type disruptions, joint subluxation, or other associated injuries
MRI or CT rarely indicated
Occasionally ultrasonography may be helpful
Physical examination remains the mainstay of diagnosis
Procedure
Zone I—Type 1 Mallet Injuries
Terminal extensor tendon disruption is common that can occur with an open laceration or closed injury from a flexion force to an extended finger
Treat with full-time extension splinting for 6 to 8 weeks followed by weaning period of part-time splinting for additional 4 to 6 weeks
Surgical pinning may rarely be indicated for patients who are unable to comply with splinting
Surgical Technique: Closed Pin Fixation of the DIPJ
Perform under local anesthesia with fluoroscopy
K-wires (0.045 ″ or 0.035 ″ diameter) in an axial or oblique direction across the joint
For axial direction, start wire at the distal tuft, just under nail plate
Wire should be in the intramedullary canal and stop just at the subchondral bone of the base of the middle phalanx to avoid PIP joint penetration
Withdraw wire a few millimeters and cut at the skin level; tap into position just below the skin
Zone I—Type II Open Mallet Injury
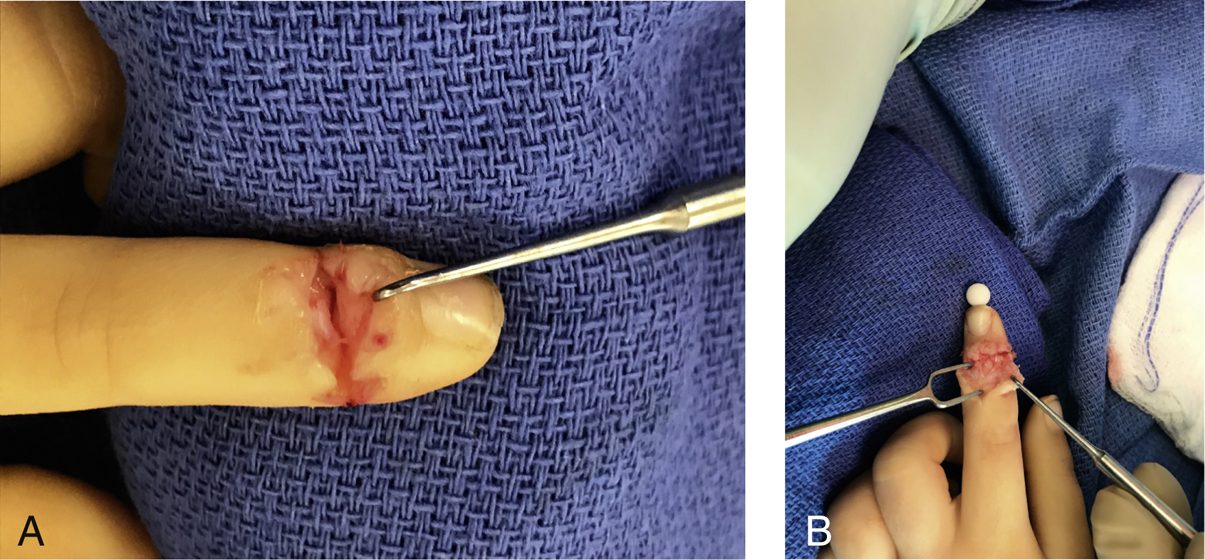
Figure 2 A, Photograph showing open mallet injury in a child. B, Photograph showing suture repair and pin fixation.
Sharp or crushing laceration to the dorsal distal joint frequently injures the terminal tendon
Débride joint and repair extensor tendon with direct suturing or dermatotenodesis technique suturing skin and tendon as one layer
Use 4-0 or 5-0 suture with a small taper needle that will not cut through thin tendon such as Supramid that is not dyed
Immobilize with K-wire across the joint in a buried fashion as described above or cut outside finger with a pin protector
Apply Mallet-type splint with pin removal at 6 weeks (Figure 2)
Surgical Technique: Suture Techniques
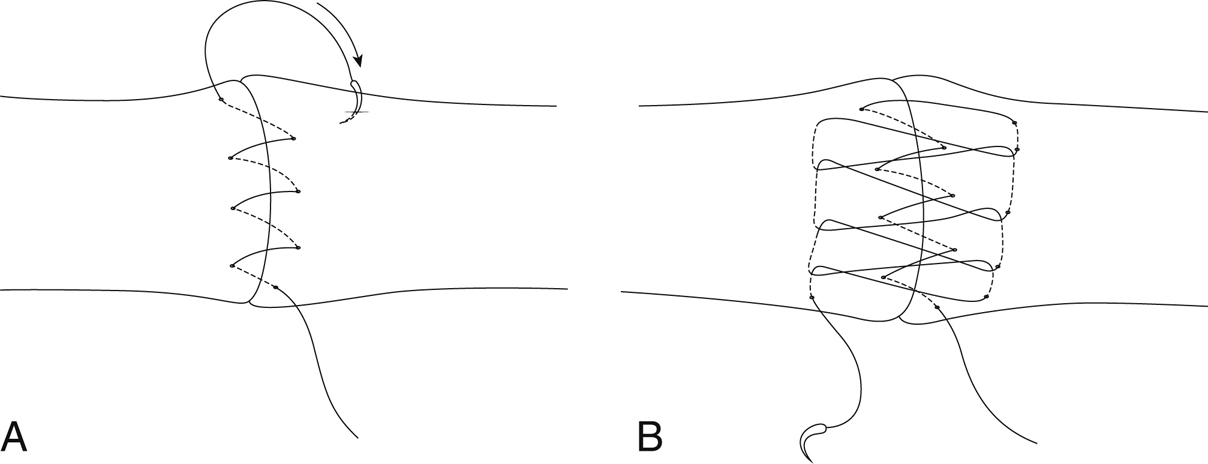
Figure 3Illustration of RIHM (running-interlocking horizontal mattress) technique. A, How to perform the new extensor tendon running-interlocking horizontal mattress repair technique: Begin the simple running suture at the near end. B, How to perform the new extensor tendon running-interlocking horizontal mattress repair technique: Run the interlocking horizontal mattress suture by starting at the far end. The suture needle passes underneath the prior crossing suture to lock each throw. Finish the suture and tie at the near end.
(Reproduced with permission from Lee SK, Dubey A, Kim BH, et al: A biomechanical study of extensor tendon repair methods: Introduction to the running-interlocking horizontal mattress extensor tendon repair technique. J Hand Surg Am2010;35[1]:19-23.)
Extensor mechanism is thin and does not tolerate shortening or lengthening
Recent evidence supports use of dorsal epitendinous suture called the running-interlocking horizontal mattress (RIHM) suture technique (Figure 3)
Core sutures techniques such as modified Kessler and Bunnell are appropriate for tubular and substantial extensor anatomy in Zone V-VII
Zone I—Type III Open Mallet Injury With Soft Tissues Loss
More complex open injury with multiple structure damaged
May require tendon graft, or if the joint is significantly injured, an arthrodesis may be required
Zone I—Type IV B Mallet Injury
Injury involves <50% of joint surface
No volar subluxation
Mallet splint or a closed pin fixation will result in satisfactory result in most cases
Recommend radiograph of the finger if a volar splint is applied, because this can produce distal phalanx subluxation dorsally
Zone I–Type IV C Mallet Injury With Subluxation
Management is controversial
Small study suggested that these patients with subluxated DIPJ can be treated satisfactorily with splinting only
Results of closed pin techniques have been satisfactory such as extension block pinning with low rates of complication
Open reduction techniques have a higher complication rate and should be reserved for painful nonunions or young patients with chronic injury
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


