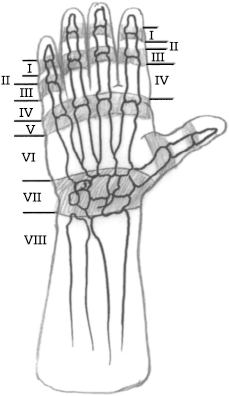
CHAPTER 17 Michael S. Bednar 1. Extensor tendon laceration in zones 1 through 8 (Figs. 17–1 and 17–2) 2. Following incision of extensor tendon for exposure of proximal phalanx (Chamay approach) 1. Lacerations in zone 6 proximal to the raffe and lacerations in zones 7 and 8 greater than 10 to 14 days old (myostatic contracture of the muscle will keep the tendon from being pulled out to its normal length; if a repair is attempted with excessive tension, the repair will be too tight) 2. Closed rupture of extensor tendon in zone 1 (mallet finger) or zone 3 (acute boutonniere deformity) 3. Crush injury with loss of tendon (requires primary or delayed grafting, depending on status of skin) 4. Infected wound (need to debride prior to placing sutures in tendon) 1. Document status of preoperative neurovascular examination. 2. If a delayed primary repair is to be performed (within 10 to 14 days), the wound is initially irrigated and closed. The extremity is splinted with the wrist in 20 degrees of extension and the fingers fully extended. 1. The patient is positioned supine on the operating table. The arm is positioned on an arm board. 2. An upper arm tourniquet is applied with cast padding. 3. The procedure may be done with general or regional anesthesia (regional is preferred to help protect he repair while the patient awakens from anesthesia). 4. Routine small joint orthopaedic surgical instruments are required. A Bunnell tendon retriever or #8 pediatric feeding tube may be required if the tendon has retracted proximally. 1. Extensor tendons are thin. The average thickness is 0.5 to 0.8 mm over the phalanges and 1.5 to 1.8 mm over the metacarpals. Care must be taken in handling the tissue to avoid shredding it. 2. Distal to the raffe, the extensor tendon will not gap more than a few millimeters. Rather than pulling the ends of the tendon toward each other, hyper-extend the joints slightly to create a tension-free repair. Because the tendon ends are easily visualized in zones 1 through 5, most of these repairs can be done in the emergency room. 3. Proximal to the raffe (zones 6 through 8), the proximal tendon may retract. Because of this retraction and the requirement to make a proximal incision, most repairs in this location are done in the operating room. Figure 17–1 Extensor tendon zones. Note that odd numbered zones overly the joints.
Extensor Tendon Repair
Indications
Contraindications
Preoperative Preparation
Special Instruments, Position, and Anesthesia
Tips and Pearls
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








