Various anatomic, electric, and physiologic tests are used in evaluation of the heart. The exercise test (ET), formerly the exercise stress test (EST), endures as one of the few valuable and practical physiologic tools to evaluate cardiac perfusion and function under controlled conditions. With the advent of newer cardiovascular imaging techniques, many physicians have moved away from this traditional physiologic test, but numerous evidence-based guidelines as established by the American College of Cardiology (ACC)/American Heart Association (AHA), as well as the American College of Sports Medicine® (ACSM), have shown that many of the new technologies do not necessarily have better diagnostic characteristics than the standard ET (21).
ET is useful for diagnosis of ischemia (sensitivity of 50%-70%, specificity of 80%-90%), prognosis of known cardiac disease, and exercise prescription (21,24).
When performing an ET, one should understand its physiology, indications, contraindications, and interpretation, with special consideration given to athletes whose abnormal responses may, in fact, be normal variations.
It is essential to understand the basic ET terminology prior to performing the test:
PR segment: The isoelectric line from which the ST segment and the J point are measured at rest. With exercise, the PR segment slopes downward and shortens in duration, at which point the PQ junction becomes the point of reference for determining the ST segment.
J point: The point that distinguishes the QRS complex from the ST segment; the point at which the slope changes; the point against which the ST segment deviation (depression or elevation) is measured.
ST segment: ST segment level is measured relative to the PQ junction. If the baseline is depressed, the deviation from that level to the level during exercise or recovery is measured. The ST segment is measured at 60 or 80 milliseconds after the J point. (At ventricular rates > 145 bpm, it is measured at 60 milliseconds after the J point) (20,25).
[V with dot above]O2max: The greatest amount of oxygen a person can use while performing dynamic exercise involving a large part of their muscle mass. This is a function of a person’s functional aerobic capacity and defines the limits of the cardiopulmonary system. It is defined by the Fick equation, which incorporates both heart rate (HR) and stroke volume (SV):
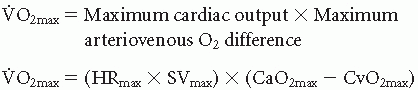
[V with dot above]O2max is defined by a central component (cardiac output), which describes the capacity of the heart to function as a pump, and by peripheral factors (arteriovenous-oxygen difference), which describe the capacity of the lungs to oxygenate the blood delivered to it and the capacity of the working muscles to extract this oxygenated blood (39). Many factors affect each of these variables.
□ HR is affected most importantly by age and (220 – age) ±12 beats (1 standard deviation [SD]) gives a good estimate of maximum HR (HRmax). However, in medicine, we use 2 SDs, which renders an extremely wide range. The scientific method for determining the individual HRmax is to perform an ET on the individual. HR is also affected by activity type, body position, fitness level, presence of heart disease, medications, blood volume, and environment (27).
□ SV is affected by factors such as genetics, conditioning (heart size), and cardiac disease. In normal subjects, an increase in both end-diastolic and end-systolic volume occurs in response to moving from an upright, at rest position to a moderate level of exercise. End-systolic volume decreases progressively as exercise intensifies in order to maintain SV. At peak exercise, end-diastolic volume may even decline.
□ Arterial oxygen content is related to the partial pressure of arterial oxygen, which is determined in the lung by alveolar ventilation and pulmonary diffusion capacity and in the blood by hemoglobin content. In the absence of pulmonary disease, arterial oxygen content and saturation generally remain similar to resting values throughout exercise, even at high levels (39).
□ Venous oxygen content is determined by the amount of blood flow directed to the muscle and by capillary density. Muscle blood flow increases with exercise not only because of increased cardiac output, but also because of the preferential redistribution of the cardiac output (> 85% of total cardiac output) to the exercising muscle. A decrease in local and systemic vascular resistance also facilitates greater skeletal muscle flow. Finally, there is an increase in the overall number of capillaries with ongoing physical training (39).
Metabolic equivalents (METs): A convenient measure for expressing oxygen uptake. One MET is a unit of sitting, resting oxygen requirements (3.5 mL O2 · kg body weight/min).
□ 1 MET = Basal O2 requirements (e.g., sitting, lying)
□ 5 METs = Energy cost for activities of daily living; poor prognosis for anginal patients; consider catheterization
□ 10 METs = Similar prognosis with medical treatment versus interventional therapy in coronary artery disease (CAD)
□ 13 METs = Excellent prognosis regardless of other exercise responses
□ 18 METs = Elite athletes
Myocardial oxygen consumption: The “double product,” an indirect measurement of myocardial oxygen consumption, measures the product of maximum or peak HR and systolic blood pressure (32). Angina normally occurs at the same double product rather than at same external workload. A normal value is considered greater than 25,000.
Conditions for which there is general consensus that ET is justified:
To assist in the diagnosis of CAD in those adult patients with an intermediate (20%-80%) pretest probability of disease
To assess functional capacity and to aid in the prognosis of patients with known CAD
To evaluate the prognosis and functional capacity of patients with known CAD soon after an uncomplicated myocardial infarction (MI)
To evaluate patients with symptoms consistent with recurrent, exercise-induced cardiac arrhythmias
Conditions for which ET is frequently used but in which there is a divergence of opinion regarding medical effectiveness of ET:
To evaluate asymptomatic males > 45 years (females > 55 years) with special occupations
To evaluate asymptomatic males > 45 years (females > 55 years) with two or more cardiac risk factors
To evaluate asymptomatic males > 45 years (females > 55 years) who plan to enter a vigorous exercise program
To assist in the diagnosis of CAD in adult patients with a high or low pretest probability of disease
To evaluate patients with a class I indication who have baseline electrocardiogram (ECG) changes
Conditions for which there is general agreement that ET is of little or no value, inappropriate, or contraindicated:
To assist in the diagnosis of CAD in patients with left bundle branch block (LBBB) or Wolff-Parkinson-White (W-P-W) syndrome on a resting ECG
To evaluate patients with simple premature ventricular contractions (PVCs) on a resting ECG with no other evidence for CAD
To evaluate men or women with chest discomfort not thought to be cardiac in origin
The above classes group the indications based on risk according to ACSM guidelines. Patients are categorized into low-, moderate-, and high-risk groups prior to beginning an exercise program. Risk stratification is based on age, sex, presence of CAD risk factors, major symptoms of disease, or known heart disease (1,19) (Tables 21.1 and 21.2).
Low risk: Asymptomatic younger individuals (men < age 45 years; women < age 55 years) and no more than one risk factor from Table 21.1.
Moderate risk: Older individuals (men age ≥ 45 years; women age ≥ 55 years) or those individuals with ≥ two risk factors from Table 21.1.
High risk: Individuals with one or more signs or symptoms from Table 21.2 or known cardiovascular, pulmonary, or metabolic disease.
In addition, level of activity is divided into low, moderate (3-6 METS or 40%-60% of [V with dot above]O2max), and vigorous (> 6 METS or > 60% of [V with dot above]O2max) exercise. Clinicians use these factors to recommend which patients need an ET (1):
Low-risk individuals do not need an ET regardless of level of activity.
Table 21.1 Atherosclerotic Cardiovascular Disease (CVD) Risk Factor Thresholds for Use with ACSM Risk Stratification
Positive Risk Factors
Defining Criteria
Age
Men > 45 years; women > 55 years
Family history
Myocardial infarction, coronary revascularization, or sudden death before 55 years of age in father or other male first-degree relative, or before 65 years of age in mother or other female first-degree relative
Cigarette smoking
Current cigarette smoker or those who quit within the previous 6 months or exposure to environmental tobacco smoke
Sedentary lifestyle
Not participating in at least 30 minutes of moderate-intensity exercise (40%-60% [V with dot above]O2R) physical activity on at least 3 days of the week for at least 3 months
Obesity
Body mass index ≥ 30 kg · m2 or waist girth > 102 cm (40 inches) for men and ≥ 88 cm (35 inches) for women
Hypertension
Systolic blood pressure > 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg, confirmed by measurements on at least two separate occasions, or on hypertensive medication
Dyslipidemia
Low-density lipoprotein cholesterol ≥ 130 mL · kg−1 · min−1) or high-density lipoprotein (HDL) cholesterol < 40 mL · kg−1 · min−1 or on lipid-lowering medication. If total serum cholesterol is all that is available, use ≥ 200 mL · kg−1 · min−1.
Prediabetes
Impaired fasting glucose = fasting plasma glucose > 100 mL · kg−1 · min−1 but < 126 mL · kg−1 · min−1 or impaired glucose tolerance = 2-hour values in oral glucose tolerance test > 140 mL · kg−1 · min−1 but less than 200 mL · kg−1 · min−1 confirmed by measurements on at least two separate occasions
Negative Risk Factor
Defining Criteria
High-serum HDL cholesterol
≥ 60 mL ≥ kg−1 · min−1
SOURCE: American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 8th ed. Baltimore (MD): Lippincott Williams & Wilkins; 2010. p. 28.
Moderate-risk individuals should have an ET prior to beginning vigorous exercise only.
High-risk individuals need an ET before any moderate or vigorous activity.
Risk stratification of patients for diagnosis of CAD divides patients into those with typical angina, atypical angina, non-anginal chest pain, or no chest pain. There are also special disease groups (e.g., diabetes mellitus) that have specific indications for testing (6,7,29,41). The Duke Treadmill Score has been validated in persons with diabetes (34).
Table 21.2 Major Signs or Symptoms Suggestive of Cardiovascular, Pulmonary, or Metabolic Disease | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
In some individuals, there may be contraindications to performing the procedure.






