Excision of Physeal Bar
Anthony A. Stans
DEFINITION
A physeal bar, or partial premature physeal arrest, is an osseous connection that forms across a physis and has the potential to affect physeal growth.7
Partial physeal arrest may result in three clinically significant consequences:
Angular deformity
Limb length discrepancy
Bone length discrepancy in a two-bone limb segment such as the forearm or leg
When evaluating a patient with a physeal bar, one must critically consider whether there is sufficient growth remaining to cause a clinically significant length discrepancy or angular deformity.
One should consider the linear magnitude of anticipated growth remaining as well as the years of remaining growth.
ANATOMY
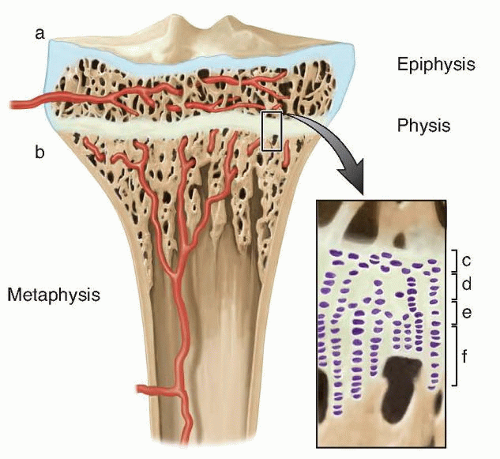
The normal physis acts as a physical cartilage barrier separating the trabecular bone of the epiphysis from the metaphysis (FIG 1).
Blood vessels typically do not traverse the physis, necessitating an independent blood supply for the epiphysis and metaphysis.1
The physis consists of four cell layers: resting zone, proliferative zone, hypertrophic zone, and endochondral ossification zone.
PATHOGENESIS
Physeal bars form when the cartilage barrier is breached as the result of trauma, infection, or cell death, and trabecular bone heals in continuity between the epiphysis and the metaphysis across the physis.9
Variation in physeal anatomy may predispose certain physes to physeal bar formation. For example, the distal radius physis is relatively two-dimensional and uniplanar, whereas the distal femoral physis has a more complex three-dimensional biconcave configuration.
Distal radius physeal fractures are quite common, yet subsequent premature physeal bar formation is relatively rare. In contrast, distal femoral physeal fractures are uncommon but distal femoral physeal bar formation is much more prone to occur after injury.
The three-dimensional configuration of the distal femoral physis contributes to the considerable energy required to fracture through the distal femoral physis, and the complex geometry increases the likelihood for violation of the physeal cartilage barrier between epiphyseal and metaphyseal bone, thereby increasing the risk of partial physeal bar formation after injury.
Breach of the physeal cartilage barrier is most frequently caused by fracture, followed by infection.
Less common pathogenesis for partial physeal bar formation may occur when the germinal or proliferating cells on the epiphyseal side of the physeal plate are injured by ischemia, infection, heat, laser, electricity, or other insult. As the germinal cells die and cell division in this region of the physis stops, partial physeal bar formation may occur.6
NATURAL HISTORY
In almost all situations, once a physeal bar has formed, length discrepancy, angular deformity, or both will continue to increase so long as the patient is skeletally immature and the affected physis (or its contralateral counterpart) continues to grow.
PATIENT HISTORY AND PHYSICAL FINDINGS
Questioning the patient quickly reveals the cause for physeal bar formation in most cases. The most common causes of physeal bar formation, fracture and infection, are typically memorable events that the patient can quickly recall.
The examiner should ask the patient and family if they have noticed a progressive limb length discrepancy, limp, angular deformity, or bony prominence; this may confirm the presence of a physeal bar.
Ideally, the orthopaedist is aware of the physeal injury, is anticipating possible physeal bar formation after injury, and is monitoring the patient at 6-month intervals with clinical examination and radiographs.
The patient is examined for lower extremity limb length discrepancy using blocks of known height under the shorter limb until the pelvis is level.
The patient is also examined for lower extremity angular deformity. The alignment at knee and ankle is assessed and compared to the contralateral limb.
The patient is also examined for upper extremity limb length deformity. Length of the affected limb is compared to that of the contralateral limb.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Appropriate imaging is critical for the evaluation of a potential physeal bar. Initial imaging is performed to determine whether the patient has sustained a clinically significant physeal injury and therefore should demonstrate limb length discrepancy and angular deformity.
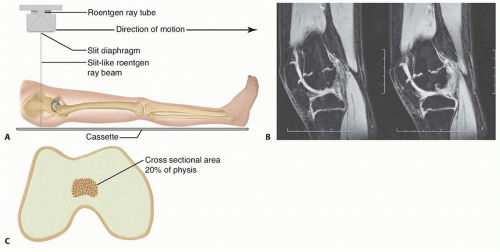
True scanograms use a slit beam that is perpendicular to the patient that scans the length of the limb and therefore has no magnification. The scanogram provides limb length and angular information with a single image (FIG 2A).
A teleoroentgenogram, or full-length, standing, hip-to-ankle radiograph taken at a distance, does result in some magnification of the limb.
By placing blocks of known height beneath the shorter limb, a teleoroentgenogram can also provide information about length and angular deformity with a single radiograph.
A ruler or magnification markers can also be placed next to the limb to allow more accurate measurement of limb length.
Orthoroentgenograms (separate exposures of the hip, knee, and ankle on a single film with a ruler) or computed tomography (CT) scout images can be used to determine limb length.
These must be supplemented by a full-length image of the limb to assess angular deformity.
If the distal tibial physis is the injured physis in question, standing anteroposterior (AP) and lateral ankle radiographs are indicated to assess angular deformity.
If limb length discrepancy or angular deformity is confirmed, additional imaging is indicated to determine the size and location of the physeal bar.
Either fine-cut CT or magnetic resonance imaging (MRI) may be used, and axial, coronal, and sagittal plane images are obtained.
The CT or MRI images are used to create a map that illustrates the location and approximate cross-sectional area of the physeal bar (FIG 2B,C).
The relative cross-sectional area of the bar is important because physeal bars occupying greater than 50% of the cross-sectional area of the physis have a less favorable result after resection. Excision of bars greater than 50% of the physeal cross-sectional area may still be indicated in young patients, such as a 5-year-old patient with a 65% bar of the distal femoral physis.
A skeletal age radiograph of the hand and wrist may be helpful in older patients if one is trying to determine if there is sufficient growth remaining for physeal bar resection to be indicated.
DIFFERENTIAL DIAGNOSIS
Physeal injury without growth abnormality
Idiopathic limb length discrepancy
Developmental cause for limb length discrepancy or angular deformity
Blount disease
Madelung deformity of the distal radius
NONOPERATIVE MANAGEMENT
Anticipated lower extremity limb length discrepancy of less than 1 cm requires no treatment.
The simplest means of correcting a lower extremity limb length discrepancy is to place a lift either inside or on the bottom of the shoe on the shorter limb.
Anticipated lower extremity discrepancy of 1 or 2 cm is most easily treated with a shoe lift inside the shoe.
Discrepancy greater than 2 cm treated nonoperatively is typically managed by a lift placed on the shoe sole.
There is no effective nonoperative treatment to correct clinically significant angular deformity caused by a physeal bar.
SURGICAL MANAGEMENT
Lower extremity physeal arrest resection should be considered in patients with an anticipated growth remaining from the affected physis of about 2 years or 2 cm.
Pure length discrepancy in the upper extremity caused by a physeal bar in the proximal humerus causes little functional problem, and anticipated discrepancy of up to 5 cm may be observed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree