Chapter 12 Evidence-based management of chronic whiplash associated disorders
In this chapter, the evidence for the management of chronic whiplash is first discussed, with a focus on physical interventions. The chapter then focuses on how to interpret this evidence when selecting appropriate interventions for patients with chronic whiplash.
Evidence base for management of chronic whiplash
To date, several attempts have been made at synthesising the evidence for chronic whiplash in a systematic manner. The first published guideline that included treatment options for chronic whiplash based recommendations for treatment on other chronic musculoskeletal conditions rather than on studies in chronic whiplash.1 A UK clinical guideline for whiplash included recommendations for chronic whiplash; however, this was founded on only one trial on patients with chronic whiplash, with the remainder of the recommendations being drawn from the literature on chronic neck pain.2 Recently, the Task Force on Neck Pain and Its Associated Disorders published recommendations on the treatment of whiplash;3 however, their systematic review only reviewed one database (Medline) from 1980, and found only one trial utilising a chronic whiplash population. The most recent published clinical guideline for chronic whiplash made recommendations for treatment based on a wider evidence base,4 with methodology scoring high on the Appraisal of Guidelines for Research Evaluation (AGREE) instrument.5 The evidence for the management of chronic whiplash in this chapter is, therefore, based on the studies selected for inclusion in this recent guideline.4
How studies were included
Studies that formed the basis for the evidence in this chapter were initially selected from those included in the recently published guideline for chronic whiplash.4 The literature for the guideline was searched until March 2007. In order to update the evidence, the same search criteria were applied to the same databases from March 2007 until December 2009.
Essential inclusion criteria have been described in detail elsewhere.3, 4 Criteria for participants were: being involved in a motor vehicle crash (MVC), symptoms persisting for more than three months since the injury, and the primary complaint of neck pain. Only randomised controlled trials (RCTs) were accepted, and then rated for quality using the PEDro scale,6 with high-quality trials satisfying a PEDro score of 8–10/10, medium-quality trials rating 4–7/10 and low-quality trials rating 1–3/10. Data, including those on populations, interventions and outcomes, were extracted. Effect sizes (mean difference [95% CI]) or relative risks (RR) (95% CI) were calculated from the primary data using an effect size calculator. Effects for pain outcomes were considered clinically significant when a mean difference of 10% was reported. This is based on previous work where effects of this size were found to be the cut-off point for patients to consider themselves to be at least ‘minimally improved’.7–9 For all other outcomes, effects were considered significant if 95% confidence intervals (CIs) did not include 1.
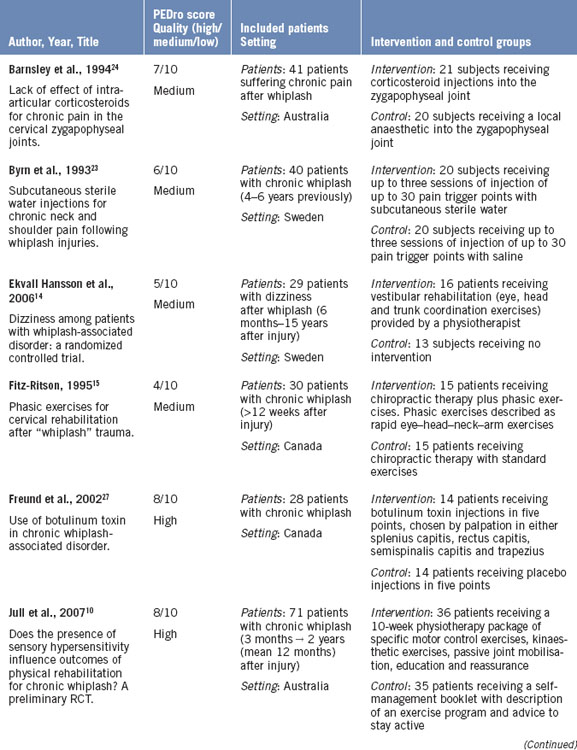
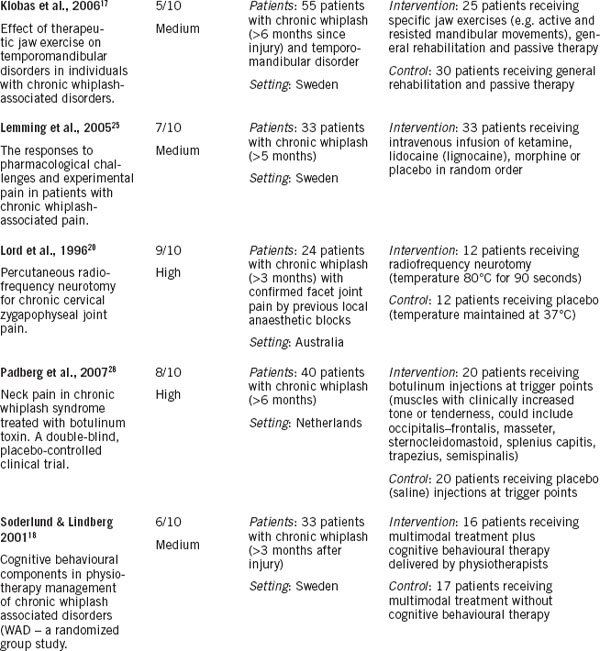
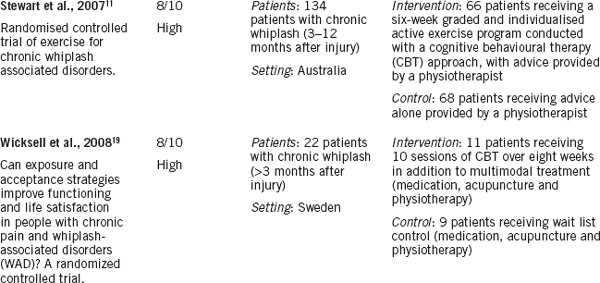
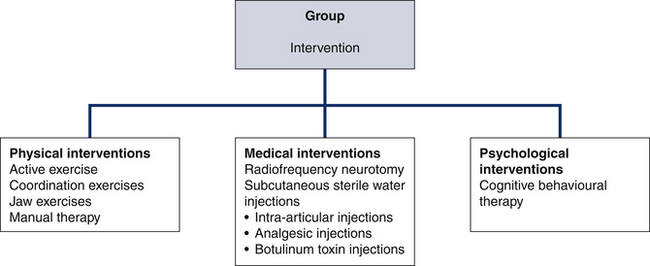
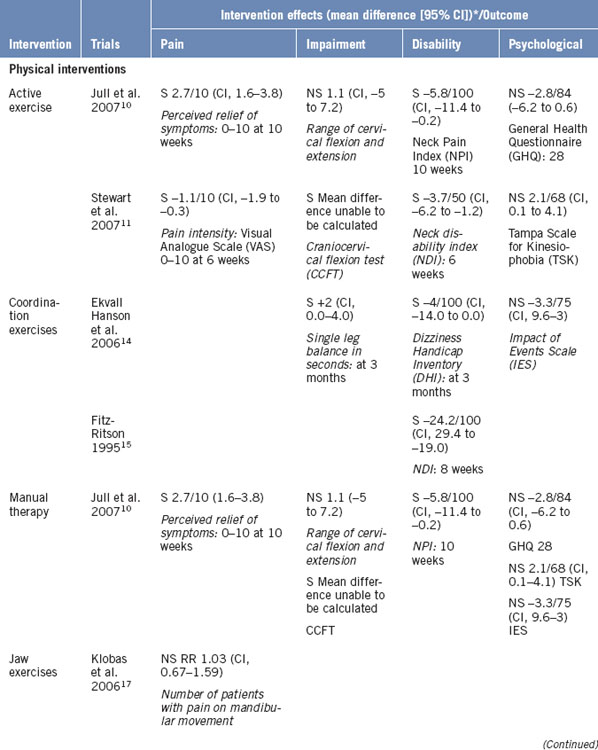
Thirteen trials were found that met the inclusion criteria and, therefore, formed the basis for recommendations for clinical practice in this chapter. The description of these trials is outlined in Table 12.1. The evidence has been categorised according to the intervention (Fig 12.1), namely physical interventions, psychological interventions and medical interventions.
Evidence for physical interventions
Active exercise
Active exercise has demonstrated positive effects in two trials.10, 11 The nature of the active exercise undertaken in the first trial10 is explained in detail elsewhere.12 Exercises were low load in nature to avoid provocation of symptoms and were directed at rehabilitating muscle control in the cervical flexor, extensor and scapula groups of muscles, as well as retraining kinaesthetic sense (Chapters 6 and 7). Active exercise was not provided in isolation in this trial, but rather, as the authors explain, active exercise was combined with advice and manual therapy when indicated.
In contrast, the exercise undertaken in the second trial11 was provided with the treating physiotherapists following cognitive behavioural principles, such as goal setting, shaping and reinforcement.13 Exercises were individualised, progressive and submaximal. They were prescribed according to the functional activities outlined by the patients as being affected due to whiplash.
Both active exercise trials demonstrated small effects for the primary outcomes of both pain and disability in the short term (Table 12.2). Jull et al.10 demonstrated a mean difference of perceived pain relief of symptoms of 2.7/10 (CI, 1.6–3.8) in the active exercise group compared with the control intervention at 10 weeks. The mean difference for disability between groups was –6% (–5.8/100 [CI, –11.4 to –0.2]). Stewart et al.11 demonstrated a mean difference of pain intensity of –1.1/10 (CI, –1.9 to –0.3) in the active exercise group compared with the control intervention at six weeks. The mean difference for disability was 8% (–3.7/50 [CI, –6.2 to –1.2]). These reported small effects suggest that there is room for improvement in treatment outcomes with this approach, which is discussed later in this chapter.
Coordination exercises
Two trials investigated the efficacy of coordination exercises and demonstrated a positive effect in comparison to the control interventions.14, 15 The interventions used in these studies were termed phasic exercises15 and vestibular rehabilitation,14 respectively. However, it appears that both interventions appear similar and involve coordination exercises between the eyes and the head and neck, with the intent of improving outcomes in whiplash patients with dizziness or visual disturbances. The phasic exercises used in Fitz-Ritson’s trial15 were developed from Janda’s original work,16 and are intended to coordinate eye movements with neck and body movements. A sample exercise is described as standing, holding a hand out to the side, then looking at the hand and turning the head to face the hand. Vestibular exercises were similarly described by Ekvall Hansson et al.14 as exercises using eye, head and trunk movements. A sample exercise was described as ‘standing on foam and turning the head from side to side’.14 The similarities in the interventions in both of these groups have, therefore, led to these trials being discussed together in this chapter.
The effects demonstrated for coordination exercises were moderate in the ‘phasic exercises trial’ and small in the ‘vestibular’ exercise trial. Phasic exercises demonstrated a mean difference in reduction of disability at eight weeks of 24% (–24.2/100 ([CI, –29.4 to –19.0]) compared with standard exercise.15 Vestibular rehabilitation demonstrated a mean difference of 6% (–6/100 [CI, –16.0 to 0.0]) improvement in the dizziness handicap inventory at six weeks compared with the control group.14 It seems unusual that two studies that used similar interventions had such different effects. However, it should be noted that several methodological issues in the Fitz-Ritson trial15 may bias the outcomes. These issues include no concealment of allocation, no blinded measurement of outcome and that the groups were not matched for age and gender. The results, therefore, should be interpreted with caution.
Therapeutic jaw exercise
One trial found no additional benefit for therapeutic jaw exercise (TJE) in patients with whiplash and temporomandibular joint (TMJ) disorder.17 Patients were randomised to receive TJE in addition to general rehabilitation and passive therapy, or general rehabilitation and passive therapy alone. TJEs were described by the authors as aiming to improve TMJ and muscle function by improving mobility, relaxing tense muscles and improving strength and coordination. The general exercises included mobility and stabilisation exercises, as well as passive therapies, such as electrotherapy and massage.
Manual therapy
No studies have investigated the efficacy of manual therapy alone in the management of chronic whiplash. Jull et al.10 included manual therapy in their multimodal intervention, which, as previously stated, also included active exercise, kinaesthetic exercise and advice. The effects for the multimodal program were beneficial in comparison to a self-management program. However, the effects for manual therapy alone cannot be determined.
The lack of trials investigating the effect of manual therapy on chronic whiplash may suggest an area for further research. However, given the now complex manifestation of some individuals with chronic whiplash, it would seem inadequate to address these complex manifestations with one modality alone.
Evidence for psychological interventions
Cognitive behavioural therapy
Three trials examined the effect of cognitive behavioural therapy (CBT) approaches for patients with chronic whiplash, all reporting positive effects in comparison to the control group.11, 18, 19 Although psychological interventions for whiplash are specifically discussed in Chapter 13, these three trials will be briefly outlined here as two of the studies were predominantly physiotherapy exercise based with adherence to principles of CBT.
The first trial, by Stewart et al.,11 as previously mentioned, included a cognitive behavioural component in the exercise arm of treatment, with both components delivered by a physiotherapist. The elements of CBT employed were based on Nicholas and Tonkin’s work,13 and included shaping, pacing, reinforcement and goal setting. Exercise and activity in this trial were applied according to these CBT principles. Given the multimodal interventions, the benefits attributable to the CBT component cannot be separated from the active exercise component in Stewart et al.’s trial.11 The intervention in the second trial (Soderlund & Lindberg18) was similar to that used by Stewart et al., in that patients in the intervention group received exercises delivered by a physiotherapist under the principles of CBT. The control group received exercises as well as other treatment modalities. However, in contrast to Stewart et al.’s trial, the effects in this trial can be attributed to the CBT element, as exercises were included in both groups. In the third trial,19 the intervention group received individual sessions of CBT delivered by a psychologist in addition to multimodal treatment (medication, acupuncture and physiotherapy), while the control group received the multimodal treatment alone. Any effects, therefore, can be attributed to the CBT.
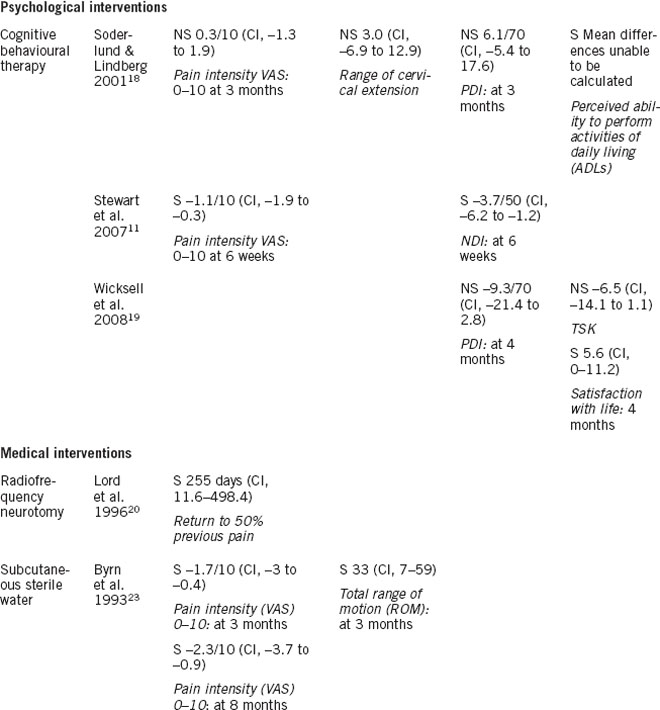
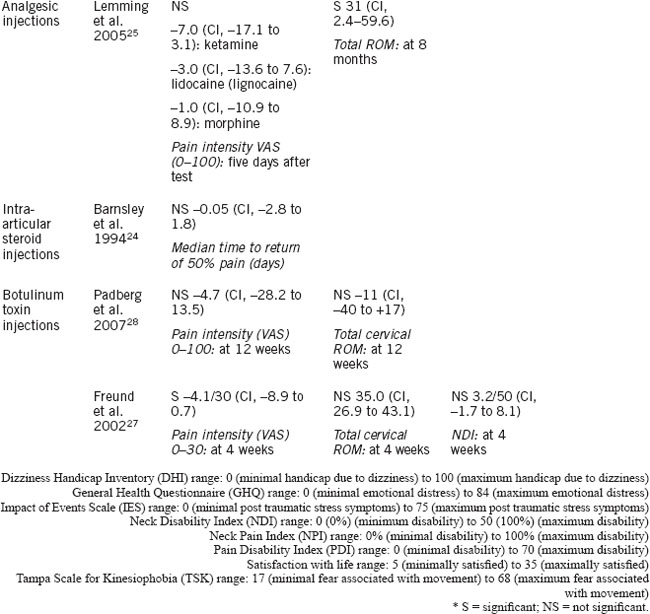
The effects in the studies employing a CBT approach delivered by a physiotherapist were small. Stewart et al.’s results for pain and disability have been discussed above (see also Table 12.2) and included a small effect for improvement in disability. The only positive effect reported by Soderlund and Lindberg18 was a significant difference in the perceived ability to perform activities of daily living in the cognitive behavioural group compared to the exercise alone group (χ2, 10.3; P < 0.05). There was no benefit demonstrated with CBT for short- and mid-term follow-up treatment of pain and disability outcomes (e.g. mean difference in disability at three months, 6.1/70 [CI, –5.4 to 17.6]). The effects for CBT delivered by a psychologist were not found to be significant. Although Wicksell et al.19 reported large effects in their original data, when the mean difference between groups was calculated for this chapter, the effects for reduction in disability (using the Pain Disability Index [PDI]) were found to be insignificant (e.g. mean difference in disability, –9.3/70 [CI, –21.4 to 2.8]).
Further investigation into the role of cognitive behavioural approaches for patients with chronic whiplash is required. Two of the three studies outlined utilised a physiotherapist to deliver exercises in a manner consistent with cognitive behavioural principles, and only one study investigated CBT delivered separately by a psychologist. To date, the evidence suggests that the effect of CBT in reducing disability due to whiplash may be minimal. However, its role in managing other aspects of psychological health is discussed further in Chapter 13.
Evidence for medical interventions
Radiofrequency neurotomy
One high-quality trial found a positive effect for radiofrequency neurotomy as a medical intervention compared with a control procedure.20 In this trial, patients were included if they had previously responded to a median branch nerve block to the facet joint, thus implicating these joints as the source of neck pain in these patients. The radiofrequency neurotomy procedure was described as inserting an electrode under fluoroscopic control to the median branch of the cervical dorsal ramus of the nerve supplying the painful joint. The temperature was raised to 80°C for the neurotomy procedure, and remained at 37°C for the control procedure.
The large effect demonstrated by radiofrequency neurotomy may need to be considered together with the costs and accessibility of this form of treatment. First, the procedure was effective with highly selected subjects (i.e. only those whose symptoms had been demonstrated, by diagnostic blocks, to arise from the lower cervical joints). Second, the trial was performed in a specialised research setting; therefore, the results may not be generalisable. The Neck Pain Task Force has also criticised this trial, commenting that responses to facet blocks were non-validated and not required to be in a pharmacological range.21 Furthermore, no other outcomes were reported, and others that were are not statistically significant. For example, at three weeks after surgery, nine subjects in the radiofrequency group compared with six subjects in the control group reported greater than 50% pain relief.22 Side-effects to the radiofrequency neurotomy have included long-term anaesthetic or dysaesthetic areas of skin.22 Therefore, while radiofrequency neurotomy is recommended in the treatment of patients with chronic whiplash and confirmed facet joint involvement, caution must be applied.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree