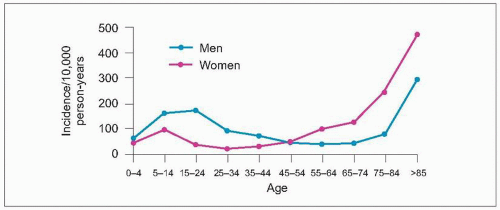
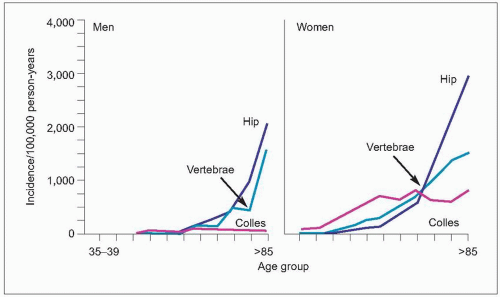
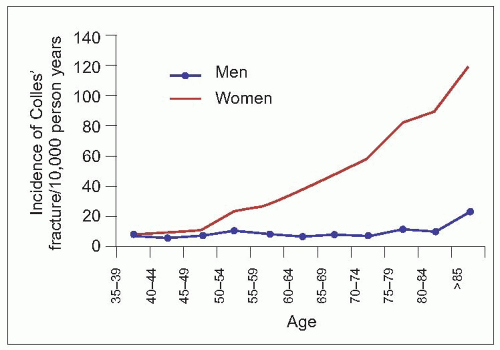
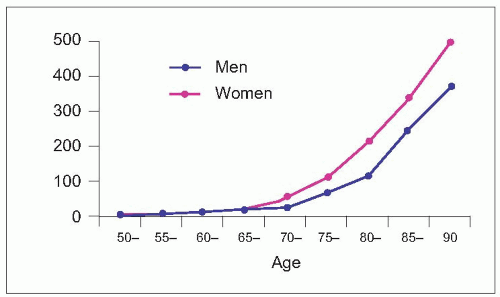
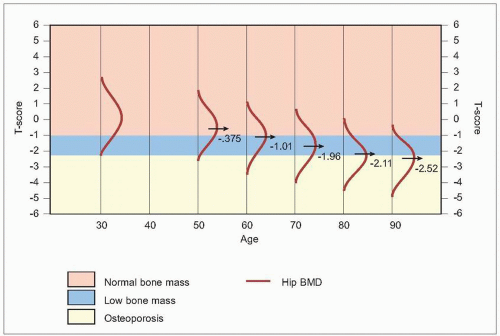
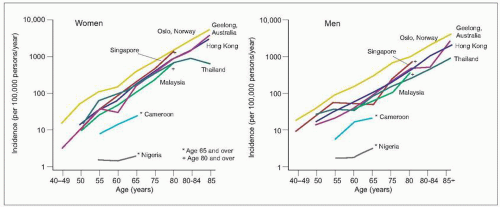
The incidence of hip fractures increases exponentially with age (
2.8). Ninety percent occur in people over 50 years of age and the average age of sustaining a hip fracture in developed countries is 80 years. The estimated rates in westernized countries are 33/100,000 person-years in women aged aged 50-54 years, rising to over 1808/100,000 person-years in women 80 years and older, with rates in men of 28 and almost 900, respectively
9 (
Table 2.1). However, the female preponderance of hip fractures is not common to all populations. The age-specific incidence varies between countries (
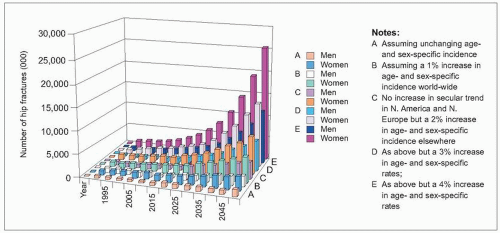
2.9). Worldwide, there were estimated to be 1.31 million hip fractures in 1990, about 909,000 in women and 405,000 in men
10. Fracture rates vary in different countries (
Table 2.1), being highest in North America and Europe, particularly in Scandinavia. The risk of osteoporotic fractures is lower in nonwhite than white populations. Incidence rates are extremely low in African countries and intermediate among Asian populations. Rates vary in regions and in Asia the rates for hip facture are twofold higher in Hong Kong than in Korea, with intermediate are reported from Malaysia, Thailand, and mainland China.