Fig. 14.1
Schematic location of the ulnar nerve
It continues its path under the flexor carpi ulnaris and above the flexor digitorum superficialis, behind the arcade of Amadio and Beckenbaugh.
In the middle part of the forearm, it gets ventral and goes along the flexor digitorum superficialis toward the Guyon’s canal in the wrist (Fig. 14.2).
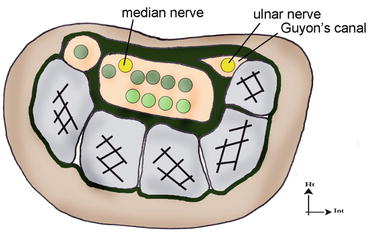
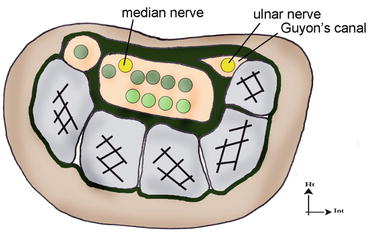
Fig. 14.2
Path of the ulnar nerve in the Guyon’s canal
It then gives off four branches, the most ulnar being motor (hypothenar eminence, interossei, third and fourth lumbricals, adductor pollicis, deep bundle of the flexor pollicis brevis) [3].
The two medium branches are the sensory nerves of the 5th and half of the 4th finger (Fig. 14.3).
Fig. 14.3
Sensorial territory of the ulnar nerve
The most radial branch forms the Riche and Cannieu anastomosis (or Berrettini anastomosis).
It innervates the flexor carpi ulnaris and the two medial heads of the flexor digitorum profundus in the forearm.
In the hand, it innervates all the intrinsic muscles except for the two radial lumbricals, the opponens pollicis, the abductor pollicis brevis, and the superficial bundle of the flexor pollicis brevis.
14.2 Entrapment Syndromes of the Ulnar Nerve [4]
14.2.1 Compression of the Ulnar Nerve at the Level of the Elbow [1, 2]
The vulnerability of the ulnar nerve, because of its anatomical path, has been known since the beginning of the twentieth century. A traumatic origin, or one secondary to a degenerative damage, was frequently found, and in 1957 Osborne described the concept of the cubital tunnel syndrome. He showed that opening this tunnel has positive effects on the symptomatology.
14.2.1.1 Etiology
Primitive forms in a context of hyper-use
Traumatic forms by direct contusion, fracture of the inferior extremity of the humerus, elbow dislocation, or prolonged compression [5]
Secondary forms, nontraumatic with arthrosis, rheumatoid polyarthritis, osteochondromatosis, or tumor
14.2.1.2 Clinical Exam [6]
It must look for traumatic or nontraumatic factors that could be causing the symptoms. The symptomatology depends on the fibers concerned by the compression; it can be mostly sensorial or motor.
Paresthesias occur in the 5th finger and the ulnar side of the 4th finger, and they can be more important during the night as the elbow is flexed (around 90°) and becomes permanent.
For the motor function, we have to look for a global loss of the clamping strength and an ulnar paralysis with Froment’s sign, revealed by a flexion of the interphalangeal joint of the thumb when pinching a sheet of paper between the pulps of the thumb and index. This compensation is related to the contraction of the flexor pollicis longus (innervated by the median nerve) that compensates the weakness of the adductor pollicis (innervated by the ulnar nerve) (Fig. 14.4).


Fig. 14.4
Froment’s test: maintain a sheet of paper being pulled away is impossible without compensating with the flexor pollicis longus (innerved by the median nerve) as the adductor pollicis (innerved by the ulnar nerve) is inefficient. (1) Negative test and (2) positive test
The weakness of the interossei is brought to light by Wartenberg’s sign, which is a permanent abduction of the 5th finger (Fig. 14.5).


Fig. 14.5
Wartenberg’s sign, meaning the 4th palmar interosseous is weak. The abduction of the 5th finger is permanent because of the effect of the extensor digiti minimi
Tinel’s sign has a sensitivity of 62 % but is not enough to unsure the nerve suffering, as it is also present in patients with no neurological damage.
14.2.1.3 Complementary Exams
We look for signs of arthrosis or traumatic sequels with radiography of the elbow.
The electromyogram is part of the systematic assessment in every entrapment syndrome and determines the seriousness and level of the injury.
14.2.1.4 Medical and Surgical Treatment
Medical Treatment
When symptomatology is intermittent with a minimal damage on the electromyogram, the medical treatment combines anti-inflammatories with an orthosis in 30° of elbow flexion, worn during the night. Compression phenomena must be reduced adapting the workstation.
Surgical Treatment [7–11]
Extra–articular neurolysis improves symptomatology in most of the cases; epicondylectomy and transposition of the ulnar nerve are used in case of relapse, nervous instability, or bony deformity.
Extra–articular neurolysis: realized with plexus block and pneumatic tourniquet. It consists in successively lifting every compression site, with section of the retinaculum of the ulnar canal, the Osborne’s fascia, and the arcade of Amadio and Beckenbaugh, while checking that there isn’t any nervous subluxation that would require an anterior transposition or a medial epicondylectomy.
Medial epicondylectomy: [7], it consists in removing the medial epicondyle to decrease the path of the nerve and the intracanal pressure during the movements of flexion–extension [5].
Subcutaneous transposition: it consists in modifying the path of the nerve, placing it under the medial epicondyle and therefore decreasing the tension and stretching during the movements of flexion–extension of the elbow. This transposition can be subcutaneous or submuscular and is realized when simple neurolysis has failed and in case of degenerative or posttraumatic deformities.
14.2.2 Compression of the Ulnar Nerve at the Level of the Wrist
Damage of the ulnar nerve in the wrist is less frequent than in the elbow. It requires a paraclinical assessment with electromyogram and echography to look for the various possible causes of damage of the nerve in this anatomical area.
The ulnar nerve gets into the palm of the hand through Guyon’s canal, which has a triangle shape and is limited by the flexor retinaculum in its superior part, the hook of the hamate laterally, and the insertion of the pisohamate ligament and the pisiform medially.
There are various etiologies, from a tumorous or vascular pathology to a traumatic or degenerative origin.
The medical treatment consists in wearing a resting orthosis during 6 weeks, followed by rehabilitation. However, most of the times the patients seek a consultation when they are already in an advanced stage, therefore needing surgery liberating the sensory branches and the motor branch.
14.3 Rehabilitation and Orthotic Treatment of the Compressions of the Ulnar Nerve [12]
14.3.1 Without Surgery [13]
As for the median nerve, this treatment concerns moderate damages of the nerve without important sensorial and motor disorders. The patient describes tingling sensations, most often during the night.
The rehabilitation and orthotic treatment delay and can even avoid surgery.
14.3.1.1 Rehabilitation
The techniques used are the same as for the median nerve, adapted to the anatomical situation of the ulnar nerve.
Fight Against Inflammation and Pain
It’s based on a combination of cryotherapy, pressotherapy, and draining massages that can help decreasing the perineural inflammation.
Longitudinal Massage
This massage is applied at the level of the accessible area of the nerve closest to the damaged area.
It consists in realizing a longitudinal pressure along 3–4 cm of the nerve, to improve its vascularization and restart the axonal flow.
The ideal pressure recreates the distal symptomatology, without producing pain. It’s maintained a few minutes, which allows obtaining a variation of the initial symptoms.
In epitrochlear–olecranon compressions, the patient is placed in decubitus with his elbow in 30° of flexion. After locating the groove (sometimes with an area with fibrosis), we realize longitudinal maneuvers along the ulnar nerve. Transversal maneuvers can also be done to relax the retinaculum of the epitrochlear–olecranon groove (or ulnar canal).
For compressions in the wrist, the patient is in the same position. We locate the external part of the flexor carpi ulnaris, where the ulnar nerve passes since the inferior 1/3 of the forearm, and realize the longitudinal massage there.
A different way of doing this technique consists in realizing a static pressure at the level of the damaged area and mobilizing the closest joint. The nerve is mobilized, which is sometimes better tolerated by the patient.
We realize this technique on the two possible compression sites, no matter where the “major” compression is.
Fight Against Perineural Fibrosis
It improves glidings between the ulnar nerve and the adjacent tissues, which limits the compressive constraints to which it is exposed and improves its vascularization.
Mobilization of the Nerve (Fig. 14.6) [14]
Fig. 14.6
Mobilization of the ulnar nerve described by Butler
Nervous mobilizations aim to mobilize the nerve respective to the adjacent tissues to limit the risks of compression and ischemia.
The progression of the mobilization is based on the Upper Limb Tension Tests described by Butler in 1991.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








