Figs. 15.1 and 15.1′
Anatomical location of the radial nerve (anterior and posterior parts)
The “medium floor” goes from the humeral condyle to the inferior part of the radial head, and in this part the nerve splits into the posterior interosseous nerve (motor innervation) and the superficial branch of the radial nerve (sensorial innervation).
The anterior branch is anterointernal and courses on the brachialis muscle. The posterior branch courses laterally between the brachialis and the brachioradialis.
The “lower floor” corresponds to the posterior interosseous nerve passing between the superficial and deep bundles of the supinator, through a muscular or fibrous arcade called the arcade of Fröhse (30 % of the cases).
The radial nerve gives off a posterior branch that innervates the extensor carpi ulnaris, the extensor digitorum, and the extensor digiti minimi with its posterior branch and the abductor pollicis longus, the extensor pollicis brevis, the extensor pollicis longus, and the extensor indicis with its anterior branch.
The anterior sensorial branch passes along the posterior side of the brachioradialis, then gets closer to the radial artery, and avoids the lateral side of the radius to cross the abductor pollicis longus, extensor pollicis brevis, and extensor carpi radialis tendons.
The nerve reaches the dorsal side of the wrist and then splits into four dorsal digital branches (Fig. 15.2).
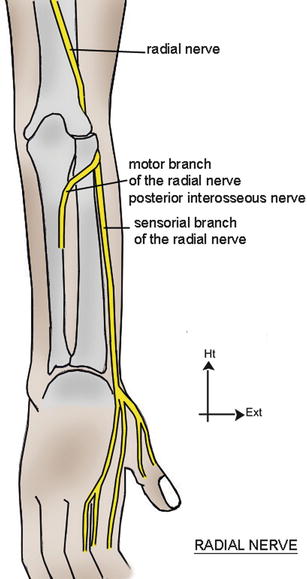
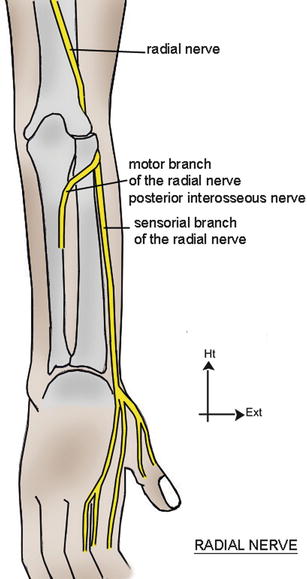
Fig. 15.2
Sensorial innervation by the radial nerve (superficial branch)
15.2 Compression in the Humeral Groove [2, 3]
A radial palsy at this level can be secondary to three mechanisms:
A traumatic damage caused by a fracture of the distal third of the humerus, which requires an exploration during the osteosynthesis.
An extrinsic compression because of a prolonged pressure or an overinflated tourniquet kept too long.
There are also “spontaneous” palsies corresponding to anatomical structures fixing the nerve to the distal part of the groove and causing mechanical conflicts during prolonged repetitive movements. This could lead to a surgical exploration if the patient doesn’t show signs of recovery after 2 months, with a disturbed EMG.
15.3 Compression in the Elbow [2–4]
In the elbow, the radial nerve is subjected to stretching and twisting constraints in flexo-extension and prono-supination. There are two distinguishable symptomatologies.
15.3.1 Radial Tunnel Syndrome
It corresponds to a compression of the radial nerve in the radial tunnel, between the humeroradial joint and its emergence from the supinator.
There is pain at the level of the epicondyle, which can spread until the wrist without sensorimotor disorders and is increased by movements of extension and supination. The differential diagnosis with epicondylitis requires a meticulous exam as pain is located at approximately 5 cm below the epicondyle. The EMG is hard to interpret but allows doing the diagnosis, following a rigorous protocol.
A conservative treatment will always be recommended at first, along with rest, adaptation of the workstation and orthosis, NSAIDs, and muscle relaxants.
After an observation period of 3 months, surgery will be proposed with opening of the superficial bundle of the supinator and the deep part of the extensor carpi radialis brevis. An orthosis is given to the patient for 2–3 weeks, with the wrist in 20° of extension.
15.3.2 Posterior Interosseous Nerve Syndrome
It corresponds to the compression of the posterior interosseous nerve at the level of the supinator arch.
It causes a more or less partial loss of the wrist and finger extension that gets worse over time and can be secondary to repetitive movements in patients who have an anatomical predisposition (thick arcade of Fröhse) or a tumor.
An MRI allows the identification of swellings compressing the nerve, and an EMG is always realized to confirm the increase of the distal motor latency and the muscular integrity.
With surgery, we can realize a neurolysis of the posterior interosseous nerve in its entire pathway along the supinator, followed by 15 days of immobilization before starting the rehabilitation.
15.4 Compression in the Wrist [2, 3, 5]
Wartenberg’s syndrome is the compression of the sensorial branch of the radial nerve between the brachioradialis and the extensor carpi radialis longus tendons, in pronation and ulnar inclination of the wrist.
The EMG confirms the diagnosis, comparing the sensorial conduction speed with the opposite side.
The treatment consists in resting the wrist in 20° of extension with an orthosis immobilizing the thumb. If the medical treatment fails, surgery allows excising at least 6 cm of the fascia between the brachioradialis and the extensor carpi radialis longus.
15.5 Rehabilitation and Orthotic Treatment
15.5.1 Without Surgery
As for the median and ulnar nerves, this treatment concerns moderate damages of the nerve without important sensorial and motor disorders. Its goal is to delay or even avoid surgery.
The patient often presents nocturnal paresthesias, without any other neurological disorder.
15.5.1.1 Rehabilitation
Fight Against Inflammation and Pain
It’s based on a combination of cryotherapy, pressotherapy, and draining massages that can help decreasing the perineural inflammation.
Longitudinal Massage
This massage is applied at the level of the accessible area of the nerve closest to the damaged area.
It consists in realizing a longitudinal pressure along 3–4 cm of the nerve to improve its vascularization and restart the axonal flow.
The ideal pressure recreates the distal symptomatology, without producing pain. It’s maintained a few minutes, which allows obtaining a variation of the initial symptoms.
For compressions in the humeral groove, the patient is placed in decubitus. The therapist grabs the posterior side of the elbow with one hand and looks for an area of induration in the lateral side of the arm with the other hand. We apply a “coma” movement to follow the path of the radial nerve.
The association of internal and external rotations of the arm effectively participates in this exercise.
For compressions in the elbow, the patient is in decubitus. The therapist maintains the forearm with one hand and places his thumb across, slightly above the flexion crease of the elbow, on its lateral side. He realizes the longitudinal massage with his thumb or alternates flexion/extension movements of the elbow, with the thumb still.
The radial nerve can also be manipulated 5 cm below the epicondyle, which is a particularly painful area in radial tunnel syndromes. The patient is in the same position as before, and the therapist grabs the forearm with both hands so that his thumbs contact with the painful area and the elbow in 100° of flexion.
He applies the longitudinal massage on the radial nerve with his thumbs or alternates flexion/extension movements of the elbow with the thumb still.
For compressions in the wrist, the patient is in the same position, and the therapist realizes longitudinal massages at the level of the emergence of the superficial branch of the radial nerve.
We can also mobilize the nerve alternating radial and ulnar inclinations, the thumb still.
Fight Against Perineural Fibrosis
It improves glidings between the radial nerve and the adjacent tissues, which limits the compressive constraints to which it is exposed and improves its vascularization.
Mobilization of the Nerve [6]
Nervous mobilizations aim to mobilize the nerve with respect to the adjacent tissues to limit the risks of compression and ischemia.
The progression of the mobilization is based on the upper limb tension tests described by Butler in 1991.
For the radial nerve, the mobilization is based on the ULTT 2b and has several stages (Fig. 15.3):
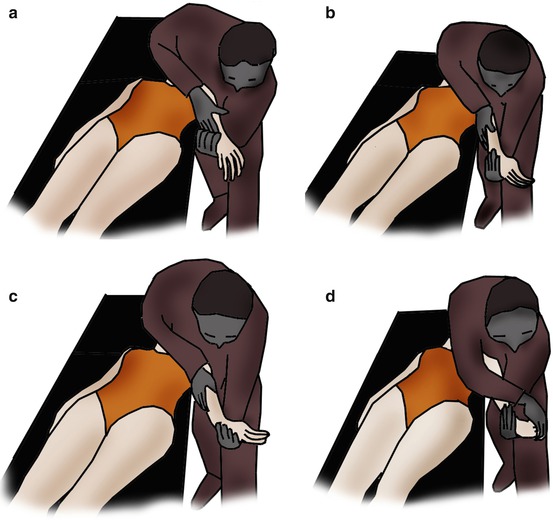
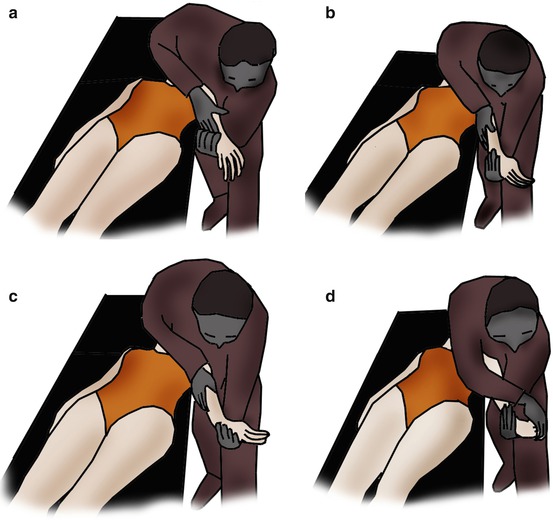
Fig. 15.3
Nervous mobilization technique by David S. Butler based on the upper limb tension tests. (a) Position with a “triple grip” (pelvis + 2 hands of the physiotherapist). (b) Shoulder internal rotation, pronation, and strong depression. (c) Wrist flexion and ulnar inclination to put the superficial branch in tension. (d) Finger and thumb flexion
Position with a “triple grip” (pelvis + 2 hands of the physiotherapist)
Shoulder internal rotation, pronation, and strong depression
Wrist flexion and ulnar inclination to put the superficial branch in tension
Fingers and thumb flexion
These stages are realized until the patient feels a bearable tension. The last position is then maintained 6 s to avoid any ischemic risk.
Mobilization of the Adjacent Tissues
Alternating contraction–relaxation–stretching of the adjacent muscles produces a perineural pumping that improves local trophicity and maintains glidings between tissues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








