Fig. 13.1
Schematic path of the median nerve
It enters the hand at the level of the carpal tunnel, which is an hourglass-shaped inextensible osteofibrous tunnel. Its narrow part is the hamulus.
It’s formed dorsally by the palmar concave osteo-ligamentous groove and closed in the front by the flexor retinaculum composed by two layers:
The superficial layer and the antebrachial fascia prolonged distally by the palmar aponeurosis [9].
The deep layer with the carpi volare proximally, then from the distal palmar crease of the wrist, from the flexor retinaculum [8, 11] that spreads from the pisiform bone to the apophysis of the sesamoid bone inward, and from the scaphoid’s tubercle to the trapezium bone outward. Its distal part is covered by fat tissues that form the fat pad of Kaplan and Milford, which contains the superficial palmar arch.
Between these two layers and the two compartments, there is the fascia of Mirza.
Its most internal part forms the floor of Guyon’s canal, limited inward by the insertion of the flexor carpi ulnaris on the pisiform bone and in the front by the antebrachial fascia.
The carpal tunnel contains the nine flexor tendons with their synovial sheath and the median nerve [11], organized in three planes:
Deep plane with the four deep flexor tendons
Medium plane with the superficial flexors (the tendons of the flexor indicis and flexor digiti minimi are deeper and more lateral than the flexor tendons of the third and fourth fingers)
Superficial plane with the median nerve, located in front of the flexor indicis and outside the axis of the fourth finger
The flexor carpi radialis passes through its own canal, separated from the carpal tunnel by a sagittal connective partition.
Mechanically, the flexor retinaculum is the first flexion pulley of the flexor system and therefore optimizes the tendon’s action, making them more efficient and avoiding the “bowstring” effect. It plays an important role in the strength of the grips.
Distally to the carpal tunnel, the median nerve gives off its terminal branches (Fig. 13.2):
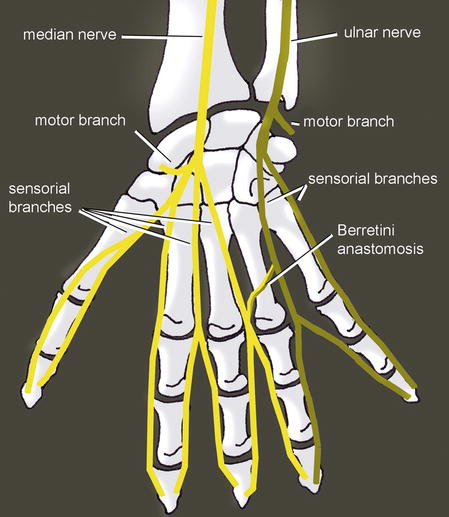
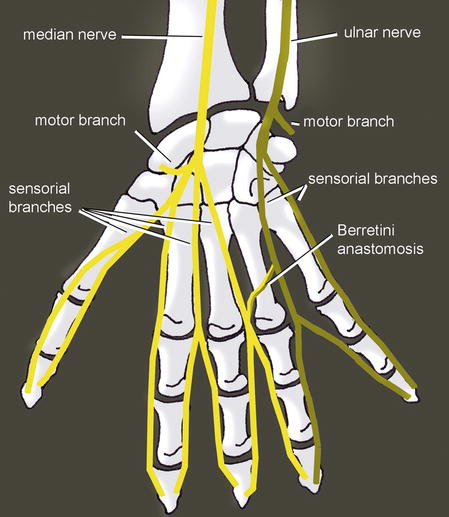
Fig. 13.2
The median nerve ends in 6 branches: 1 motor, 4 sensorial, and 1 anastomosed with the ulnar nerve (Berrettini)
The thenar branch usually comes from the radial side of the nerve, half the time beyond the inferior side of the ligament, in 30 % of the cases behind the ligament bypassing its inferior part, and in 20 % of the cases behind the ligament, passing through it. It rarely comes from the anterior side or the medial part of the nerve.
The proper palmar digital nerve of the thumb.
Interdigital nerve: in 90 % of the cases, there is an anastomosis between the nerve of the third space and the one of the fourth space (terminal branch of the ulnar nerve from Guyon’s canal). It’s called the anastomosis of Berrettini, located in the fat pad and therefore exposed during surgery.
Therefore:
At the motor level, it innervates:
The anterior compartment of the forearm, except the flexor carpi ulnaris and the two medial heads of the flexor digitorum profundus (innervated by the ulnar nerve)
The two radial lumbrical muscles (branches from the first and second space) and the external thenar muscles (abductor pollicis and superficial fascicle of the flexor pollicis brevis, as the deep fascicle of the flexor pollicis brevis and the adductor pollicis is the medial thenar muscle innervated by the ulnar nerve) innervated by the thenar branch
At the sensorial level, it innervates:
The palmar side of the three first fingers and the radial half of the fourth finger
The dorsal side of the two distal phalanges of the index and the third finger and the radial side of the two distal phalanges of the fourth finger (Fig. 13.3)
Fig. 13.3
Sensorial innervation by the median nerve
13.2 Carpal Tunnel Syndrome
Carpal tunnel syndrome is a set of clinical signs, meaning there is an entrapment of the median nerve at the level of the carpal tunnel.
It’s the most frequent pathology of the hand and mostly occurs bilaterally in 50-year-old women [15].
13.2.1 Physiopathology
There is a dual physiopathology in this syndrome:
Ischemia of the median nerve, which explains the increase of symptoms during the night and the alleviating maneuvers described by the patients [10].
Intra-canal hyper-pressure (from 3 to 30 mmHg), causing the apparition of symptoms. It can be related to various causes:
Fractures of the inferior extremity of the radius.
Tenosynovitis of the flexors [11], inflammatory rheumatism, hormonal changes, and diabetes. Aside from obvious metabolic contexts, tenosynovitis is present only in 4 % of the cases, making the synovectomy useless.
Intra-canal tumors and muscular anomalies (hypertrophic lumbricals, palmaris longus or flexor digitorum superficialis with a distal or digastric muscle belly, Frohse palmaris profundus from the anterior side of the radius to the deep side of the superficial palmar aponeurosis).
Repeated flexion–extension movements, often related to a professional or sports activity.
Despite the large number of possible causes, it is most often idiopathic.
The two mechanisms are probably intricately linked. The preponderance of one or the other can explain the different electro-clinical observed forms. In fact, the median nerve at the level of the wrist is composed of 50 % big fibers, which are the only ones explorable by EMG and sensible to pressure. The small fibers (C fibers and fibers of the sympathetic system) are more sensible to ischemia.
13.2.2 Clinical and Paraclinical Signs
The presence of digital acroparesthesia, sometimes felt like pain and mostly during the night, seems to be the most characteristic sign. The fifth finger isn’t usually damaged.
The reproduction of the signs with a cuff inflated above the venous pressure (Gilliat test), a prolonged flexion of the wrist (Phalen test), or the percussion of the nerve (Tinel pseudo-test) is evocative, but far from being constant.
Their respective predictive values are 100, 87, and 50 %. A hypoesthesia in the territory of the median nerve and an atrophy of the external thenar muscles make the diagnosis obvious but are, fortunately, very rare as they mean we’re dealing with a severe deficit form of the syndrome.
Other than the following neurologic injuries, the Raynaud syndrome is the key element of the differential diagnosis.
The EMG is essential as it studies the distal motor latency and the speed of the sensorial conduction and allows [13, 19]:
Confirming the diagnosis.
Assessing the severity.
Looking for an associated neurologic injury realizing a double crush syndrome, compression of the ulnar nerve in the elbow and radicular compression, or thoracic outlet syndrome, diabetic neuropathy, for example. In the case of double crush syndrome, it’s hard to tell which pathology causes which symptoms. The carpal canal treatment is simple (contrary to the previous pathologies) and should therefore be proposed first.
There are 10 % false negatives. They are starting forms with damage of the small fibers that are explored on the exam or a transitory damage of a small number of big fibers. In these cases, a test infiltration is essential.
13.2.3 Medical and Surgical Treatment
A conservative treatment (orthosis, gestures, corticoid infiltration) is possible, with 30–75 % of improvement depending on the authors [17]. It is therefore difficult to know if this improvement is due to a lull in the pathology or is a therapeutic effect. Infiltration often betters the speed of the nervous conduction after 1 month but doesn’t change the spontaneous evolution after 1 year, unlike the surgery that we realize after a loss of 2.7 m/s [16].
The surgical treatment is essential in three cases [1, 2]:
If there is a sensorial or motor deficit. When there’s deficit, there is little pain, with a major axonal loss. It occurs more often in old patients and may be a particular form of the pathology, the evolution from painful subjective forms to forms with deficit being poorly known. Surgery clearly improves symptoms.
In the case of neurogenic path of the abductor pollicis brevis, the other parameters only reflecting the importance of the conduction block.
If the symptoms persist after 1 year.
Surgery is very efficient, with an almost immediate relief. Aside from all the secondary effects that can happen in every hand surgery, some specific secondary effects are frequent and can persist until 6 months in 25 % of the cases, justifying the cessation of work because of loss of strength and pillar pain. They’re related to hypertrophic healing of the retinaculum or slight modifications in the architecture of the carpal bones.
Some publications demonstrate that complex surgeries of the root canal like synovectomy or endo-neurolysis are useless and that an incision in the axis of the fourth finger is safe [20, 23]. Therefore, several authors have suggested the endoscopic section of the retinaculum and have presented their results in the early 1990s [20, 22, 24].
The endoscopic technique allows a better postoperative comfort and an earlier use of the hand, as well as a shorter leave from work [12]. However, the results 6 months after surgery are the same, except maybe for the strength recovery.
The endoscopy is reliable, with a relapse rate comparable to the conventional technique and a close failure rate (0.05 %) [18].
The complications are more frequent than with the conventional technique but are resolving most of the time. In 2/3 of the cases, the complication is the contusion of the nerve or the branch of the third space occurring when preparing the ligament or introducing the endoscope [18].
The technique with one opening seems to have better results than the one with two openings, and it is logical to reduce the scar as much as possible, especially in a contact area [24].
Contrary to the conventional technique, the endoscopic liberation allows conserving the inter-thenar fascia and the superficial palmar aponeurosis.
To avoid any neuroma in the palmar cutaneous branch of the median nerve, the cutaneous incision must stay medial to the palmaris longus. However, similar branches intended to innervate the skin of the hypothenar eminence arise from the ulnar nerve (cutaneous palmar branch of the ulnar nerve and nerve of Henlé), and only a small incision (endoscopic) decreases the risk of neuroma.
13.2.4 Rehabilitation and Orthotic Treatment, Without Surgery or Preoperative
When the nerve damage is moderate, the rehabilitation and wearing a resting orthosis can delay or even avoid surgery. This treatment is only efficient in some cases, most of the time when the inflammation has mechanical causes.
We can observe temporary paresthesia, often nocturnal, without other neurologic disorders.
13.2.4.1 Rehabilitation
It’s about fighting against inflammatory phenomena and, depending on the indications, mobilizing the median nerve.
Fight Against Trophic Disorders and Pain
This exercise is based on the association of cryotherapy, pressotherapy, analgesic vibrotherapy, and draining massages that can help reduce intra-canal edema, therefore participating in the decompression of the median nerve in the carpal tunnel.
Longitudinal Massages
These massages are applied on the accessible area of the nerve that is closest to the painful area.
It consists in realizing a longitudinal pressure along the nerve on 3–4 cm to improve vascularization and enable axonal flow.
The ideal pressure recreates the distal symptomatology without creating pain. It’s maintained for a few minutes, until we obtain a variation of the initial response [14].
The preferential area is proximal to the flexor retinaculum, where the nerve isn’t reachable.
In this area, the nerve is located on the ulnar side of the flexor pollicis longus [4] and the flexor carpi radialis and on the radial side of the palmaris longus.
The patient is placed in decubitus, with a 30° flexion of the elbow.
After finding the median nerve, longitudinal maneuvers are realized along it.
Another way to apply this technique consists in pressing the median nerve and slowly mobilizing the wrist in flexion/extension. It’s not the finger but the nerve that moves, which can be better tolerated by the patient.
Fight Against Perineural Adherences
These exercises improve glidings between the median nerve and the adjacent tissues, which limit the compressive constraints and improve vascularization.
Nervous Mobilizations [6]
The goal of the mobilizations of the nerve is to mobilize the median nerve respective to the adjacent tissues to limit the risks of compression and ischemia.
The progression of the mobilization is based on the upper limb tension tests, described by Butler in 1991.
For the median nerve, the mobilization is described by the ULTT 1 or the ULTT 2a in several steps:
ULTT 1 based on a shoulder abduction of 90° or more (Fig. 13.4):
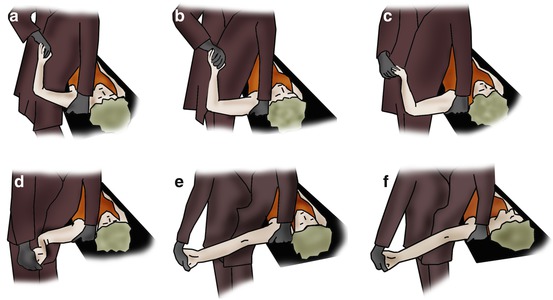
Fig. 13.4
Mobilization of the median nerve (ULTT1). (a) Ninety degrees of shoulder abduction (110° for the roots C5 to C7). (b) Slight shoulder depression. (c) Wrist supination and extension, finger extension, elbow flexed. (d) Ninety degrees of shoulder external rotation. (e) Elbow extension. (f) Contralateral head rotation
90° of shoulder abduction (110° for the roots C5 to C7)
Slight shoulder depression
Wrist supination and extension, finger extension, and elbow flexed
90° of shoulder external rotation
Elbow extension
Contralateral head rotation
ULTT 2a based on the association traction/external rotation of the shoulder (Fig. 13.5):
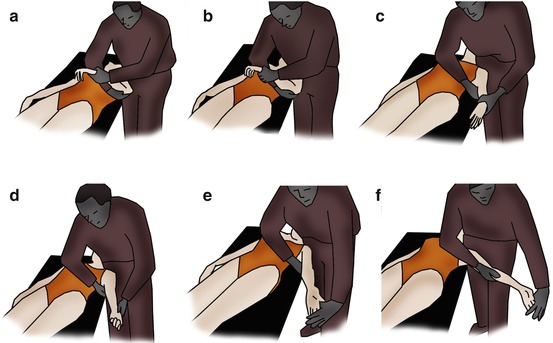
Fig. 13.5
Mobilization of the median nerve (ULTT 2a). (a) Position with a “triple grip” (pelvis + 2 hands of the physiotherapist). (b) Strong shoulder depression. (c) Elbow extension. (d) Shoulder supination and external rotation. (e) Wrist and finger extension. (f) Shoulder abduction until 30°
Position with a “triple grip” (pelvis + 2 hands of the physiotherapist)
Strong shoulder depression
Elbow extension
Shoulder supination and external rotation
Wrist and finger extension
Shoulder abduction until 30°
The two mobilizations can be done, but in any case, the steps are continued until the patient feels a bearable tension.
The last position is held 6 s to avoid any ischemic risk.
Mobilizations of the Tissues Adjacent to the Nerve
Alternating contraction–relaxation–stretching of the adjacent muscles allows a perineural pumping that improves local trophicity and maintains the inter-tissue glidings.
This mobilization of the tissues around the nerve can be realized by alternating movements in the wrist and fingers, allowing a dissociative contraction of the muscles adjacent to the median nerve.
It can be obtained by imitating the animated images in a slideshow (Fig. 13.6). The patient maintains the position while the picture is on display.
Fig. 13.6
Imitation exercises mobilizing the tissues adjacent to the median nerve
Massages Against Fibrosis
They’re realized along the median nerve, on the anterior part of the forearm, and at the level of the flexor retinaculum and the thenar muscles.
We use dot-shaped massages, glided pressures, and kneading that improve local trophicity, fight against perineural fibrosis, and relax the muscles adjacent to the nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








