Fig. 18.1
Endoscopic ulnar nerve release utilising the hooded scope as developed by Hoffman and Storz. The ulnar nerve is seen below the flexor carpi ulnaris (Copyright Dr. Gregory Bain)
Rehabilitation following endoscopic repair involves early active range-of-motion activities and a return to normal activities as tolerated.
18.2.2 Endoscopic Ulnar Nerve Anterior Transposition
If the ulnar nerve is found to be unstable, an endoscopic anterior transposition can be performed [29]. A standard ulnar nerve release is performed. The MIMS is excised. Care is required to ensure any adjacent vessels are identified and cauterised if required. The ulnar nerve is then mobilised and transposed anterior to the medial epicondyle (Fig. 18.2). Once the nerve is checked proximally and distally to ensure no kinking, the subcutaneous fat is sutured to the soft tissue over the medial epicondyle. Rehabilitation involves placing the elbow into a sling in flexion for 1 week to allow for soft tissue healing and stabilisation of the nerve in its new bed.
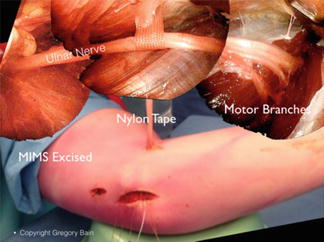
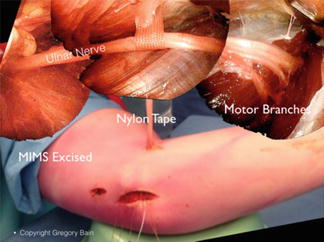
Fig. 18.2
Endoscopic ulnar nerve transposition. Below is the elbow with the main working portal over the medial epicondyle. A proximal portal was used to retract the ulnar nerve at the time of resection of the medial intermuscular septum (MIMS). An anterior portal has a nylon tape to retract the nerve. The composed photo shows the ulnar nerve held transposed by the nylon tape and the multiple motor branches dissected free (Copyright Dr. Gregory Bain.)
18.2.3 Olecranon Bursitis
Surgery traditionally involves open bursectomy, with incision over the point of the olecranon. However, wound healing can be a problem owing to the area of bridging skin. Endoscopic techniques allow for faster healing with improved outcome.
Utilising the wet technique, two separate 1.5 cm longitudinal portals are made 2 cm proximal and distal to the margins of the bursa, in the midline. Distension is maintained via saline inflow and arthroscopic cannula to prevent fluid draining away. The scope can then be placed into the bursa, resecting the bursa from inside-out until normal tissue planes are visualised. Care should be taken to protect the overlying skin and to prevent any perforations that may develop into sinuses.
The senior author’s preferred technique is the dry endoscopic procedure, specifically for treatment of sterile olecranon bursitis [36], utilising the Storz endoscopic equipment described above (Fig. 18.3). A 2 cm incision distal to the bursa is made to allow the introduction of the hooded scope, and the subcutaneous tissues are elevated off the bursa and olecranon. A separate proximal portal is made, and a pituitary rongeur is used to resect the bursa and cautery to control bleeding and fluid accumulation postoperatively (Fig. 18.4). To prevent recurrence in the dead space, the elbow should be placed in a sling at 90° of flexion.
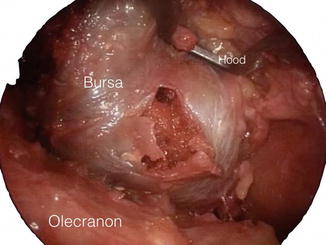
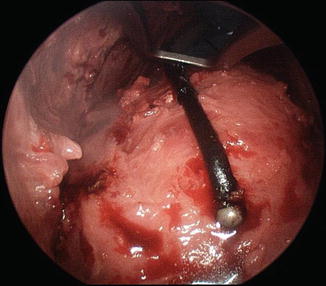
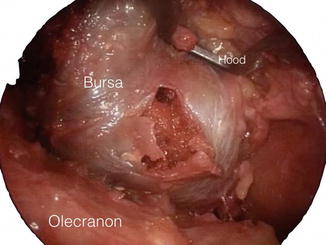
Fig. 18.3
Endoscopic olecranon bursa resection utilising dry endoscopy. Note the hood suspends the soft tissues and skin. The bursa is released and then excised whilst maintaining the skin over the olecranon, optimising healing (Copyright Dr. Gregory Bain)
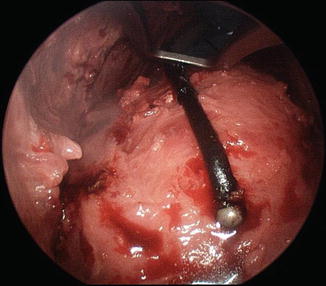
Fig. 18.4
After endoscopic resection of olecranon bursa, the tourniquet is deflated and cautery is used on any significant bleeding points identified (Copyright Dr. Gregory Bain)
18.2.4 Olecranon Spurs
Once the position of the spur is identified using fluoroscopy, dry endoscopy can be used to resect the spur by introduction of high-speed burr. Fluoroscopy can then be used to ensure complete resection (Fig. 18.5).
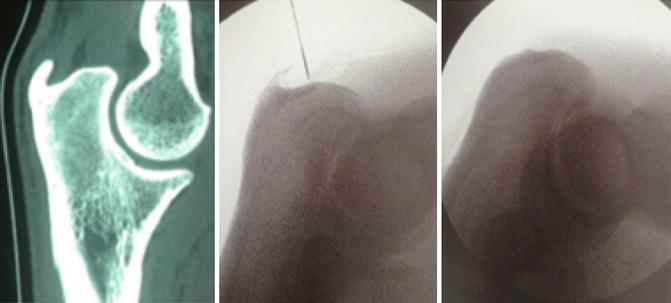
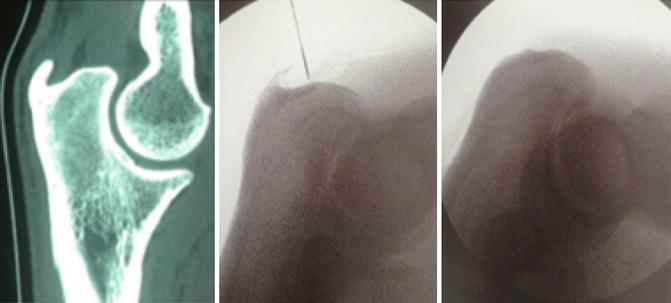
Fig. 18.5
Olecranon spur as seen on CT scan. Intra-operatively, fluoroscopy is used to identify the position of the spur and post-operatively to ensure complete resection (Copyright Dr. Gregory Bain)
18.2.5 Dry Elbow Arthroscopy
Dry arthroscopy has been utilised in elbow, providing greater appreciation of the anatomy of the elbow joint, reducing the risk of fluid extravasation and compartment syndrome. When the joint is distended with air, the synovial and articular surfaces are able to reflect light, allowing superior clarity and better understanding of subtle findings of the soft tissues and articular cartilage (Fig. 18.6). This technique has been shown to be particularly useful in synovitis, as fluid distension in wet arthroscopy may compress the soft tissues, change the shape of the synovium and reduce its vascularity [30, 34].
Fig. 18.6
Dry elbow arthroscopy, note the quality of the image and the depth of field. The synovial fluid on the surface of the articulation reflects the light, providing a better understanding of the surface itself. In the normal fluid arthroscopy, the synovial folds are flattened and the small vessels are compressed. However with dry arthroscopy, the synovial fold maintains its shape, and the small vessels perfuse the synovium and can be seen (Copyright Dr. Gregory Bain)
However, there are relative contraindications to using dry arthroscopic techniques. When radiofrequency ablation is required, wet arthroscopy should be used to provide cooling effect to the joint and prevent risk of chondrocyte damage. Furthermore, there is a theoretical risk of air embolus when arthroscopy is performed under air pump pressure and when a tourniquet is not inflated. Therefore, this technique should not be used with an air pump until further research is available [34].
It can also be used for any of the therapeutic procedures, such as synovectomy, resection of osteophytes and capsulectomy (Fig. 18.7).
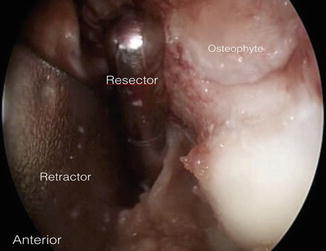
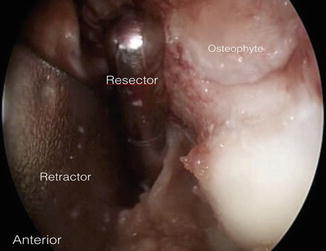
Fig. 18.7
Dry elbow arthroscopy is being used here for anterior humeral osteophyte resection. Intermittent irrigation is used to clear any debride from the resector (Copyright Dr. Gregory Bain)
18.2.6 Arthroscopy and Elbow Arthroplasty
Arthroscopic management of elbow arthroplasty has been utilised as a valuable adjunct in the diagnosis of painful or swollen arthroplasty. Arthroscopy in this setting allows for targeted biopsies for microbiological diagnosis and for assessment of mechanical factors before an informed decision regarding definitive management is made [34]. Mechanical diagnosis can be made, and sometimes running repairs can be performed (Fig. 18.8).
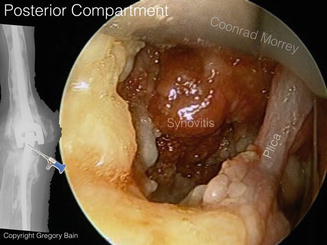
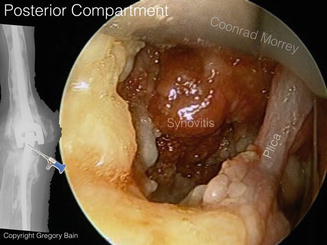
Fig. 18.8
Arthroscopic assessment of a patient with a suspected elbow arthroplasty infection shows synovitis and plica that was excised (Copyright Dr. Gregory Bain)
18.2.7 Endoscopic Suturing
The senior author has performed deep suturing endoscopically using barbed sutures (Fig. 18.9). These are ideal for endoscopic repairs, as they do not require knot tying. The sutures can be inserted in the same way as we perform microsurgery. They can be used to repair deep fascia and other soft tissues [36].
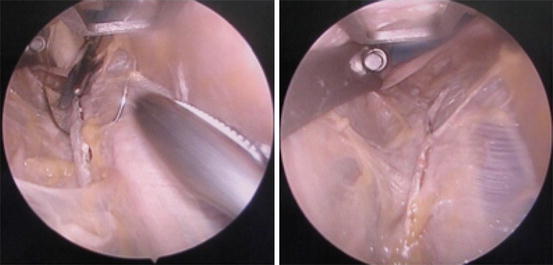
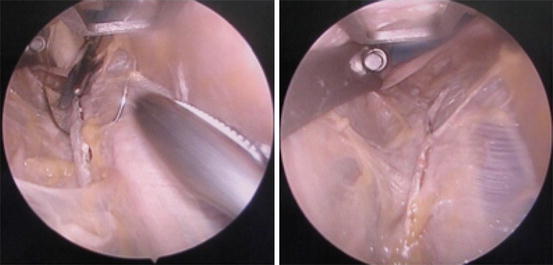
Fig. 18.9
Endoscopic suturing using barbed sutures in a cadaveric model. The suture technique is similar to the microsurgery. Once positioned, the sutures are pulled tight, and the barbs of the suture hold the suture in place (Copyright Dr. Gregory Bain)
18.2.8 Other Procedures
Soft tissue endoscopy has grown to encompass a range of pathologies (Table 18.1). In the elbow, endoscopy has been successfully utilised in biceps bursoscopy and distal biceps tendon repairs [9, 15, 37]. which is described in more detail in another chapter in this series. In the forearm, endoscopic techniques have been used for decompression of the anterior interosseous nerve [22, 25], pronator syndrome [27], and performing fasciotomy in cases of chronic exertional compartment syndromes [10, 32].
Table 18.1
Indications for endoscopic procedures about the elbow, forearm and wrist
Procedure | Indication |
|---|---|
Releases | Ulnar nerve release at cubital tunnel anterior interosseous nerve release |
DeQuervain’s tenosynovitis, intersection syndrome | |
Forearm fasciotomy in chronic exertional compartment syndrome | |
Excision | Bursectomy (olecranon bursitis) |
Tenosynovectomy (e.g. of the extensor tendons) | |
Excision of lesions (e.g. olecranon rheumatoid nodules) | |
Olecranon spur resection | |
Harvesting | Vessel graft (e.g. radial artery for CABG) |
Nerve graft (e.g. distal PIN, MCNFA)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





