CHAPTER 31 Endoscopic Carpal Tunnel Release: The Chow Dual-Portal Technique
Rationale and Basic Science
James C. Y. Chow published his dual-portal technique in 19891 and reported his clinical results in 1990.2 The rationale for developing an endoscopic carpal tunnel release is similar to that used in the development of other endoscopic techniques such as laparoscopic cholecystectomy and arthroscopy. A minimal incision approach to carpal tunnel release leads to a decrease in postoperative pain and an earlier return to daily activities. The dual-portal system has the advantage of creating a fixed space in which to operate. The cannula is fixed at the proximal and distal portals. The cannula creates an operative field into which instruments can be easily moved (Figure 31.1).
Technique
Anesthesia
IV regional anesthesia (Bier block) can also be used. It does not allow the instant feedback of local anesthesia, but once the tourniquet is released the patient’s neurological status returns quickly to preoperative levels such that a complete neuromuscular exam can be performed prior to breaking the sterile field. The Bier block eliminates the need to give fentanyl and midazolam in the doses needed during the “pure” local anesthesia as the patient does not feel the cannula pass into the carpal tunnel. Axillary block and general anesthesia have been used but eliminate the patient feedback noted with the local techniques.
Surgical technique
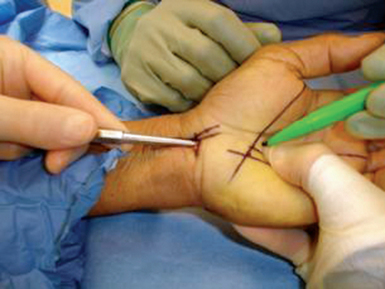
A “washboard” sensation is felt as the tip of the dissector passes over the ridges in the dorsal surface of the transverse carpal ligament (TCL). If this washboard sensation is not felt, the dissector is either palmar to the TCL or in Guyon’s canal. The distal edge of the transverse carpal ligament is able to be palpated using the curved dissector and the position of the distal edge of the transverse carpal ligament is marked on the overlying palmar skin (Figure 31.1).
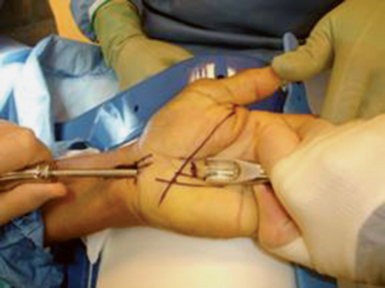
The curved dissector is removed and the slotted cannula/obturator is placed into the carpal tunnel. The operator’s hand is placed on the palmar aspect of the hand between the thenar and hypothenar eminences and the cannula system is lifted (the lift test). The examiner’s palpating fingers should not be able to feel the cannula. If the cannula is palpable, it is either palmar to the TCL or in Guyon’s canal and must be removed and repositioned. Once the cannula is safely placed, taking care to stay close to the hook of the hamate and keeping the cannula system parallel to the long axis of the arm, the wrist and fingers are extended and the hand is placed on the hand holder. The tip of the cannula system is palpated just distal to the distal edge of the TCL. The cannula system is then passed through the distal portal while pushing the superficial palmar arch dorsally with the palmar arch depressor (Figure 31.2).
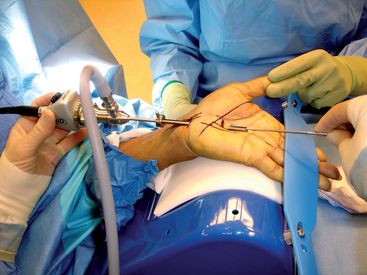
The distal portal is established approximately 4 to 5mm distal to the distal edge of the transverse carpal ligament along the long axis of the ring finger. This effectively allows the cannula system to pass between the common digital nerves of the third and fourth web spaces, distal and palmar to the superficial palmar arch and palmar to the communicating branch sensory branch between the median and ulnar nerves.3 Once the cannula system passes out through this distal portal, the system is fixed in position. The elastic band is placed across the fingers to hold the hand in position. The assistant extends the thumb, thus placing tension on the TCL (Figure 31.3).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree