(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
Whether the operation is performed by endoscopic or open technique, enough bone has to be removed to prevent impingement of the retrocalcaneal bursa between the calcaneus and Achilles tendon. Endoscopic calcaneoplasty has several advantages, including low morbidity, functional aftertreatment, outpatient treatment, excellent scar healing, a short recovery time, and quick sports resumption, in comparison with the open technique. In this chapter, the terminology of Achilles-related pathology is highlighted. The etiology, history, physical examination, and additional diagnostic imaging for detection of chronic retrocalcaneal bursitis are mentioned. The operative technique for endoscopic calcaneoplasty including positioning and detailed description of portal placement and surgical technique is mentioned.
Retrocalcaneal bursitis is an inflammation of the bursa in the recess between the anterior Achilles tendon and the posterosuperior calcaneus (retrocalcaneal recess), resulting in a clinically visible and painful soft tissue swelling, medial and lateral to the Achilles tendon. On conventional radiography, a posterosuperior calcaneal prominence can be identified.
Endoscopic calcaneoplasty for retrocalcaneal bursitis has several advantages, including low morbidity, functional aftertreatment, outpatient treatment, excellent scar healing, a short recovery time, and quick sports resumption.
21.1 Introduction
In patients with a chronic retrocalcaneal bursitis, who fail to respond to conservative treatment, an endoscopic calcaneoplasty can be indicated (Van Dijk et al. 2001). There are many different surgical techniques to treat chronic retrocalcaneal bursitis. Regardless the technique, resecting sufficient bone is important for a good outcome. A recent systematic review concluded that endoscopic surgery is superior to open intervention (Wiegerinck et al. 2012a).
21.2 Terminology for Achilles-Related Pathology
Overuse injuries of the Achilles tendon can be divided into insertional and non-insertional problems. Since there is no evidence available for inflammation in patients with “tendinitis” the term tendinosis has been proposed (Puddu et al. 1976). In 1998, Maffuli proposed to use the term tendinopathy: clinical definition, characterized by a combination of pain, swelling, and impaired performance of the tendon (Maffuli et al. 1998). When the pain is located at the posterosuperior calcaneal prominence, this entity has been called Haglund’s syndrome (Haglund 1928). Originally Haglund described a condition of a painful hindfoot caused by an enlarged posterosuperior calcaneal border in combination with wearing of rigid low-back shoes (Van Dijk 2006). Today in Haglund’s disease, we describe a clinical situation of pain and tenderness at the posterolateral aspect of the calcaneus where a calcaneal prominence can be palpated. This entity is also known as “pump bump.” A distinction between Haglund’s disease and other pathologic conditions such as a superficial Achilles bursitis must be made. It must be differentiated from Haglund’s syndrome. This syndrome involves a painful swelling of an inflamed retrocalcaneal bursa sometimes combined with insertional tendinopathy of the Achilles tendon. The syndrome is caused by repetitive impingement between the ventral aspect of the Achilles tendon and the posterosuperior calcaneal prominence. Patients typically have pain after a period of rest, when starting walking. Operative treatment consists of removal of the inflamed bursa and resection of the bony prominence. A distinction should be made with other pathologies in this region.
We have proposed a terminology which comprises the combination of anatomical location, symptoms, clinical findings, and pathological changes for each entity (Van Dijk et al. 2011; Wiegerinck et al. 2012b). The terminology is shown in the insert. Achilles tendinopathy and paratendinopathy often coexist. Retrocalcaneal bursitis is often seen in combination with insertional tendinopathy. Other combinations are possible but occur less frequently.
Terminology for Achilles Tendon Pathology
1.
Achilles Tendinopathy (Fig. 21.1)


Fig. 21.1
Achilles tendinopathy. Clinical picture to show the area of the pain. X-ray to show level of pathology (thickened Achilles tendon). On the right a clinical example
The main symptoms are Achilles tendon pain and swelling located typically at 2–7 cm from the insertion onto the calcaneus and impaired performance. It involves isolated pathology of the tendon proper and includes the histopathological diagnosis of tendinosis.
Tendinosis implies the histopathological diagnosis of tendon degeneration without clinical or histological signs of intratendinous inflammation and is not necessarily symptomatic.
2.
Achilles Paratendinopathy
Paratendinopathy is defined by degeneration and/or inflammation of the thin membrane around the Achilles tendon. Exercise–induced pain and local swelling around the tendon’s midportion are the main symptoms.
Acute paratendinopathy is characterized by edema and hyperemia of the paratendon, with infiltration of inflammatory cells, possibly with production of a fibrinous exudate that fills the tendon sheath causing palpable crepitation on physical examination.
In chronic Achilles paratendinopathy, exercise–induced pain is the main symptom, while crepitation and swelling diminish.
3.
Insertional Achilles Tendinopathy (Fig. 21.2)
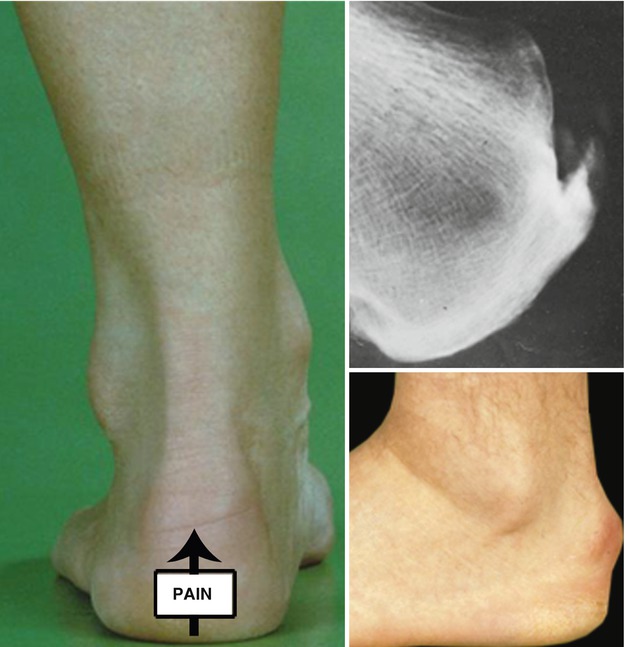
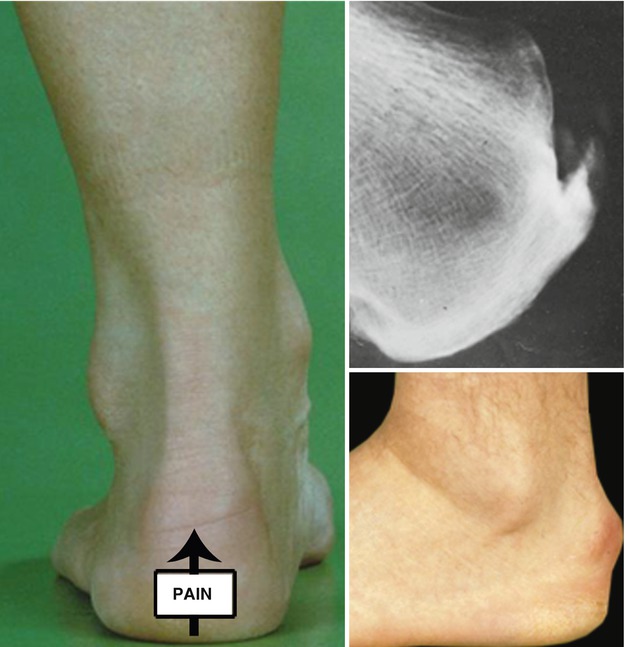
Fig. 21.2
Insertional Achilles tendinopathy. Clinical picture to show the typical location of pain on palpation: midportion insertion. The X-ray shows a typical spur at the insertion side. The clinical example on the right bottom shows the typical appearance of a patient with symptomatic insertional Achilles tendinopathy
It is defined as tendinopathy at the Achilles tendon insertion onto the calcaneus resulting in bone spurs and calcifications inside the tendon at the insertion site. Patients complain of pain and stiffness and sometimes (a solid) swelling. On physical examination the tendon insertion (at the midportion of the posterior calcaneus) is painful. A swelling may be visible and a bone spur may be palpable.
4.
Retrocalcaneal Bursitis (Fig. 21.3)


Fig. 21.3
Retrocalcaneal bursitis. The pain is typically located at the level of the posterosuperior border of the calcaneus on the medial and lateral side, just next to the Achilles tendon (see arrows). On the X-ray (bottom right) the Kager’s triangle between the Achilles tendon and the calcaneus is blurred. On the top right a clinical example with swelling of the retrocalcaneal bursa medial and lateral from the insertion of the Achilles tendon
It is an inflammation of the bursa in the recess between the anterior inferior side of the Achilles tendon and the posterosuperior aspect of the calcaneus (retrocalcaneal recess), which results in a clinically visible and painful soft tissue swelling, medial and lateral to the Achilles tendon at the level of the posterosuperior calcaneus. On conventional radiography, frequently a posterosuperior calcaneal prominence can be identified.
5.
Superficial Calcaneal Bursitis (Tendon Not Involved) (Fig. 21.4)


Fig. 21.4
Superficial calcaneal bursitis. On the left we see the typical location of the pain on the posterolateral calcaneus just anterior to the lateral insertion of the Achilles tendon. The X-ray does not show an abnormality. On the bottom right a clinical example of such a superficial bursitis on the lateral side of the calcaneus
An inflammation of the bursa located between a posterolateral calcaneal prominence and the skin, which results in a visible, painful, solid swelling, and discoloration of the skin on the posterolateral side of the calcaneus. It is often associated with rigid heel shoes. The Achilles tendon is not involved.
21.3 Anatomy
The retrocalcaneal bursa is situated in the retrocalcaneal recess between the anterior aspect of the Achilles tendon and the posterosuperior part of the calcaneus (Fig. 21.5).
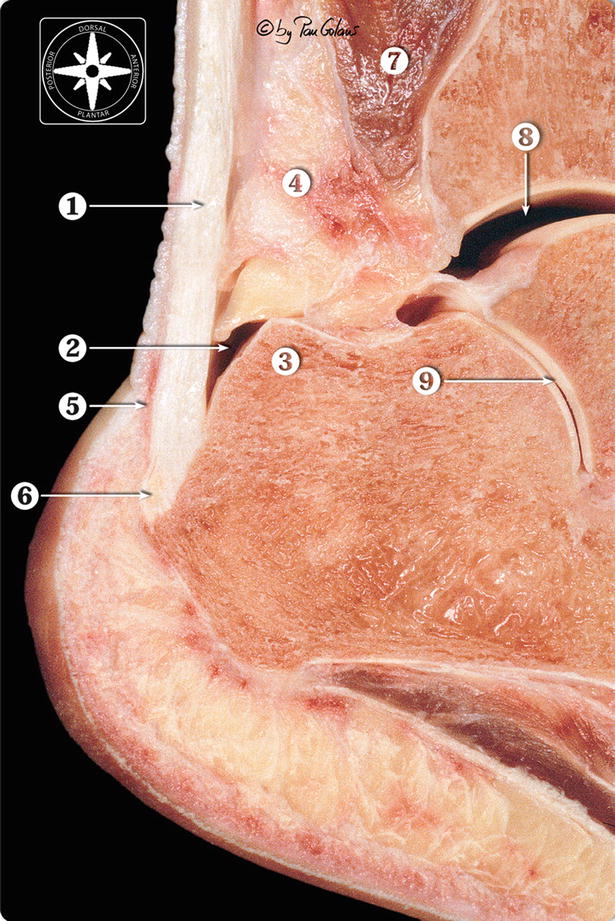
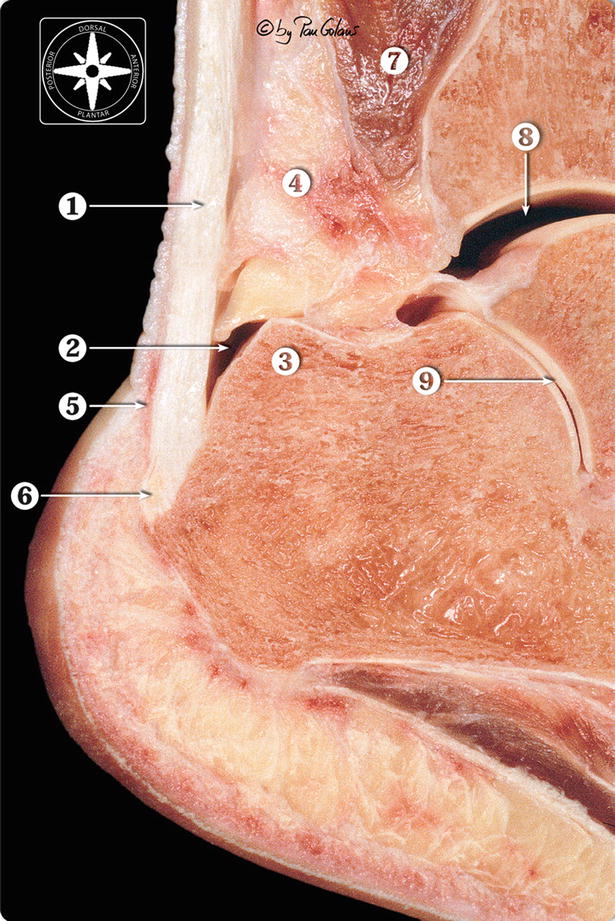
Fig. 21.5
Sagittal section of the ankle. Posterior detail. 1 Calcaneal or Achilles tendon. 2 Retrocalcaneal bursa. 3 Posterosuperior part of the calcaneus. 4 Kager’s fat pad or pre-Achilles fat pad. 5 Subcutaneous bursa. 6 Bone spur in the insertional Achilles tendinopathy. 7 Flexor hallucis muscle belly. 8 Ankle joint. 9 Subtalar joint (With kind permission of © Pau Golanó 2013)
Kager’s fat pad, also known as the pre-Achilles fat pad, is a mass of adipose tissue occupying the Kager’s triangle. Normally this fat pad, as seen on a lateral standing radiograph of the ankle, is a triangular radiolucency with sharp, gently curving borders. The anterior border is the posterior aspect of the flexor hallucis longus muscle and tendon, the posterior border is the Achilles tendon, and the distal border is the superior surface of the calcaneus.
21.4 Etiology
Retrocalcaneal bursitis is caused by repetitive compression of the retrocalcaneal bursa between the anterior aspect of the Achilles tendon and the posterosuperior aspect of the calcaneus. It occurs most often at the end of the second or the third decade, mainly in females, and is often bilateral. However, it may occur in both sexes and at any age.
With dorsiflexion of the ankle, the anterior part of the tendon impinges against the posterosuperior rim of the calcaneus. This repetitive motion can lead to retrocalcaneal bursitis. A hindfoot varus and pes cavus are both predisposing factors for heel pain. In the cavus foot, the calcaneus is not only in varus malalignment, but it is also more vertical, which results in a more prominent projection posteriorly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








