Fig. 8.1
aPosteroanterior and b lateral radiographs of the forearm with ulnar stress fracture
All the stress fractures described in the two studies were treated nonoperatively. The patients with complete stress fractures were treated with cast immobilization and subsequent continued activity restriction, and the patients with normal or stress reactions on their radiographs simply stopped rifle drill training and vigorous forearm exercises for 6 weeks [18, 19].
Several recommendations have been proposed to decrease the incidence of forearm stress fractures . Most importantly, military commanders and recruits should be educated about this injury in order to set up a proper training schedule and encourage early diagnosis and treatment. It is recommended that the training protocol be adjusted to (1) use a lighter substitute to replace the rifle in the initial 6 weeks of training; (2) gradually advance the duration of training hours per day in a proper sequence; and (3) extend the time evenly, allocate the training load during the intensive training period, and extend the duration of this period [19]. In addition, a high index of suspicion for a forearm stress fracture should prompt ordering of a bone scan, which shows pathologic uptake within 24 h in 95 % of patients after a stress injury to a bone [20].
It is also important to screen patients early who may have increased risk factors for a stress injury. Although all the previously mentioned studies reported on male subjects, under military conditions, the female-to-male ratio for stress fractures is 4–6:1, which is double the rate seen in athletes [21]. It is hypothesized that women’s bones are more prone to stress with increased load carriage. Female soldiers who present with stress fractures should be screened for vitamin D levels and a thorough menstrual history should be obtained as well. The female athlete triad, the combination of disordered eating, amenorrhea, and osteoporosis, may predispose a female soldier to the development of a stress fracture. However, in a recent study of 423 active duty women, no subject exhibited the full female athletic triad [22]. In addition, some studies have shown that sustained use of a progesterone-based contraceptive may decrease the bone mineral density in women, particularly in those engaged in high levels of physical activity [23].
Olecranon Bursitis
Wasserzug et al. reviewed two 18-man infantry platoons, with soldiers aged 19–20 years old, during their basic military training [24]. Over a period of 10 months, nine soldiers from one platoon developed septic olecranon bursitis, which was defined as an extensive local infection with intense peribursal cellulitis or infected skin lesion that was accompanied by systemic symptoms or signs of a fever of > 37.7 °С, chills, or leukocytosis of more than 10,000 leukocytes/mm3 in the peripheral blood. The authors reported a 3.86 (CI, 1.1–13.6; p = 0.04) relative risk of developing septic olecranon bursitis in soldiers who had moderate to severe trauma to the skin overlying the elbow. They suggested that this trauma served as the “port of entry” for the bacteria. Staphylococcus aureus carrier state was not statistically significant for the development of septic olecranon bursitis, although the rate of S. aureus isolation in the two platoons was 81 %, compared with 20–37 % in the general population. After the outbreak in septic olecranon bursitis, both platoons in the aforementioned cohort were treated with nasal mupirocin ointment for local control and nasal eradication of S. aureus. After this 5-day treatment, no further cases of septic olecranon bursitis were reported.
Despite the lack of statistical significance between carrier state and clinical infection, the absence of reported cases after nasal mupirocin treatment and the fact that the severe infections were associated with a specific S. aureus clone support a potential contribution of S. aureus carrier status. Furthermore, 62 % of the isolates were related to other isolates suggesting a transmission due to close contact and shared equipment during infantry training [24]. In addition, soldiers should be educated on the Army standards of field hygiene that include hand-washing with soap and water after handling any item that can potentially transfer germs and frequent bathing to decrease pathogens. Also according to regulations, during field training exercises, all service members must bring their own toilet articles such as soap, shampoo, washcloths, towels, toothbrush, dental floss, fluoride toothpaste, talcum powder, and foot powder; furthermore, they should not share these items to prevent the spread of infections [25]. In addition, as severe skin injury is identified as a significant risk factor for septic olecranon bursitis, and the morbidity is primarily seen in the dominant elbow, which carries the brunt of the weight of a soldier’s weapon, soldiers should be encouraged to use elbow pads which are part of the standard issue combat equipment [24].
Medial and Lateral Epicondylitis
Lateral and medial epicondylitis are common insertional tendinopathies at the elbow affecting the origin of the extensor carpi radialis brevis and flexor carpi radialis and pronator teres, respectively. An epidemiological study of approximately 12 million US military service members demonstrated an unadjusted incidence rate of 2.98 per 1000 person-years for lateral epicondylitis. This was compared to 0.81 per 1000 person-years for medial epicondylitis. Increasing age was associated with a higher rate of both lateral and medial epicondylitis. Although lateral epicondylitis was diagnosed more frequently in women than in men (adjusted incidence rate ratio of 1.22 [95 % CI 1.19–1.26]), there was no difference in the occurrence of medial epicondylitis between men and women [26].
Both of these tendinopathies are initially treated with nonoperative management to include splinting, occupational therapy, and numerous types of injections, to include corticosteroids, autologous blood, and botulinum toxin [26]. Surgical options include some form of tendon debridement, either done through an open incision or arthroscopically. However, the majority of cases of lateral epicondylitis resolve after approximately 1 year of conservative treatment, with or without treatment [27]. Therefore, it is important to counsel both the active duty service members and their chain of command about the expectations and duration of treatment, as nonoperative management may affect their ability to participate in required military duties for an extended period of time.
Lateral and medial epicondylitis have been associated with both current and former smoking [28]. It is hypothesized that nicotine’s vasoconstrictive properties may place tendons at a higher risk for injury and slow or prevent healing. As suggested earlier, a combined strategy of education and decreased access to low-cost tobacco products may help reduce the prevalence of nicotine use within the military population. These tendinopathies have also been associated with occupational demands combining repetitive and forceful activities, and the risk of developing lateral epicondylitis was more common in patients who had a longer exposure to these activities [28]. This association supports the hypothesis that medial and lateral epicondylitis are caused by repeated microtrauma at the origin of the common flexor and extensor tendons. Once again, it is a combined effort of the patients and their chain of command in order to find ways for the service members to modify their physical load factors and decrease the repetitive activities about their elbow.
Triceps Tendon Rupture
Anabolic steroid abuse was suspected as a contributing factor in a midsubstance rupture of the triceps tendon reported in a 35-year-old active duty soldier by Stannard and Bucknell [29]. The tear, which was 2 cm proximal to the triceps insertion into the olecranon, was sustained during a hyperflexion injury while the soldier was weight lifting. The injury occurred approximately 3 weeks after the patient had received the last in a series of six separate steroid injections for olecranon bursitis over a 1-year period. The soldier had also reported a history of anabolic steroid abuse ending approximately 6 months earlier.
In general, as tendon is the strongest link in the musculotendinous chain, excessive stress placed against the contracted triceps muscle usually results in an olecranon fracture, as opposed to a tendon rupture (Fig. 8.2) [29]. Therefore, it is suspected that both anabolic steroid abuse and local steroid injections are likely to cause damage to an otherwise normal tendon. Similar to the biceps tendon ruptures, this case highlights the need to screen soldiers for anabolic steroid abuse. The authors also recommend caution in using local steroid injections to treat inflamed tissues in a population of strength athletes who are placing high demands on their muscles and tendons [29].
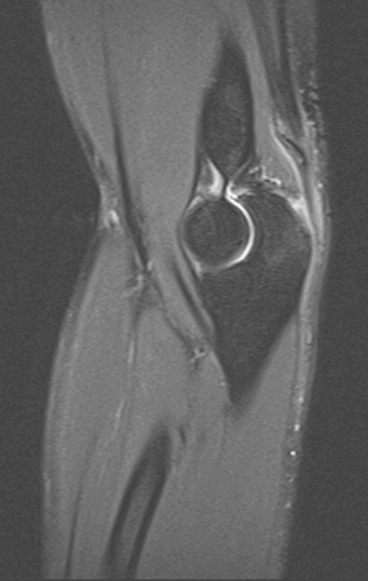
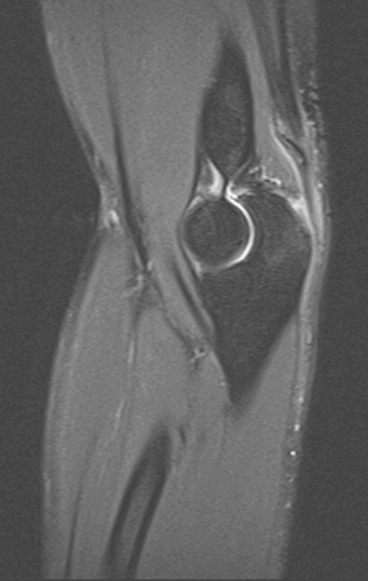
Fig. 8.2
MRI image of low-energy triceps rupture
Scaphoid Fractures
The incidence of scaphoid fractures in the general population in the USA, as estimated by data drawn from the National Electronic Injury Surveillance System (NEISS) from 2002 to 2006, was 21,481 fractures among 909,309 total wrist fractures, with an estimated incidence of 1.47 fractures per 100,000 person-years [30]. It is not surprising, then, as scaphoid fractures are found in the highest rates in young active males, that the incidence in a military population is higher. This is confirmed by a Defense Medical Epidemiology Database (DMED) estimate demonstrating that the incidence is in an order of magnitude higher at 1.21 per 1000 person-years [31]. At Tripler Army Medical Center, from 2001 to 2003, the incidence was 43 cases per 100,000 personnel per year [32].
The mechanism of injury is classic, such as fall on the outstretched hand or direct blows to the wrist such as those sustained while pugil stick fighting. In the military system, scaphoid fractures are referred through unit medical clinics and battalion aid stations by nonspecialists. Given the high incidence and the potentially devastating complications of a missed injury, detection and referral algorithms have been proposed based on the clinical scenario [32].
In addition, the proposal for percutaneous screw fixation treatment for nondisplaced acute scaphoid fractures has come from the military as well. Bond et al., in 2001, proposed in a prospective, randomized study that fixation of these scaphoid fractures with a percutaneous cannulated screw resulted in shorter time to clinically apparent union and earlier return to military duty (8 weeks as opposed to 15 weeks) than if treating the fractures with cast immobilization [33]. This is important considering that return to duty has many implications for deployment, the individual’s career, and the needs of the military.
Hand and Wrist Soft Tissue Injuries
Hand and wrist soft tissue injuries encompass a wide variety of diagnoses, encompassing overuse and acute injuries classified under “sprains.” According to DMSS data, in 2006, the number of military visits related to “sprains and strains” of the hand and wrist were 17,395, while visits related to contusions were 12,385. A total of 11,815 visits were related to overuse injuries of the hand and wrist [4].
Specifically, the incidence of de Quervain’s tenosynovitis in the military has been described. Via the DMED, an ICD-9 query for the diagnosis, 727.04, from the years 1998–2006 has revealed 11,332 cases in 12,117,749 person-years. Women have a significantly higher rate of de Quervain’s tenosynovitis at 2.8 cases per 1000 person-years compared to men at 0.6 per 1000 person-years. In addition, it was found that personnel of age greater than 40 had a rate of 2.0 per 1000 person-years compared to 0.6 per 1000 for personnel under 20 years, as well as a racial difference, which demonstrated that blacks were affected at 1.3 per 1000 person-years compared to whites at 0.8 [34].
Another disease entity described in the literature with respect to the military is carpal tunnel syndrome (CTS). In an epidemiological study of the US Navy from 1980 to 1988, it was found that the incidence was 493 cases per 4,095,708 person-years in men and 90 cases in 365,668 person-years in women. The incidence was higher in women, especially in white women. Occupations with higher standardized incidence ratios included aviation-support equipment technician, engineman, hull-maintenance technician, boatswain’s mate, and machinist’s mate. In women, occupations with significantly high standardized incidence ratios included boatswain’s mate, engineman, hospital corpsman, ocean-systems technician, and personnelman [35].
The overall incidence of CTS in the US military population according to an ICD-9 code (354.0) query of DMED data from 1998 to 2006 is 3.98 per 1000 person-years, in a population of 12,298,088 person-years. This is consistent with previous epidemiological studies of certain populations or working groups reporting incidences between 1.5 and 3.5 per 1000 person-years [36–40]. Again, females have a higher incidence with an adjusted incidence ratio of 3.29, and enlisted personnel and senior officers had an increase in incidence, suggesting that perhaps here there was an occupational relationship [41, 22]
A more recent analysis written in 2011 with stricter means of capturing patients with CTS demonstrated a declining incidence during the period from 2000 to 2010 from 2.71 to 1.37 per 1000 person-years with a crude overall incidence rate of 1.71 per 1000 person-years. This reflects an incidence similar to the general population. The incidence is thought to be an underestimate, however, given that the analysis required two outpatient visits with this diagnosis rather than one. However, again it was shown that females have a higher incidence, as well as personnel who were older. Other occupational risks included being in the Air Force and in health care and administrative occupations [42].
Specifically, personnel who perform activities involving repetitive bending and twisting of the hands and wrists and use vibrating tools are known to be at a relatively high risk for CTS. The incidence of this problem among dental personnel is described by Lalumandier et al. in a survey study identifying the likelihood of having symptoms of CTS. By survey analysis, 25.4 % were determined to indicate a high probability of CTS. Further more, of the 18 dental job specialties, dental therapy assistants and dental hygienists had the highest prevalence of CTS, 73 and 57 %, respectively [43]. Further more, another study using actual clinical and electrodiagnostic data in a sampling of personnel has determined that at baseline the incidence of median nerve abnormalities among dental personnel even prior to training is higher than the 5 % reported in healthy populations but less than the previously mentioned 25 % [44]. Another study in a different sample determined that even after training there was no shift in the prevalence of electrodiagnostic abnormalities of the median nerve [45].
Injuries to the Hand
Injuries to the hand are very common and are often the cause of evacuation out of theater. These injuries are not necessarily due to battle injuries; in fact, in one study of isolated hand injuries in the British military, in a 6-year period, only 9 % were from battle. From this 6-year period, 6337 medical cases were evacuated back to the UK, 6.5 % of which were identified as hand injuries. Half of the injuries involved fractures, and 73 % of the patients required surgery. In the cases of personnel requiring surgery, 1/3 of them had surgery in a deployed setting, and of these patients who had primary nerve or tendon repairs tended to do worse than their counterparts who had surgery after evacuation in a delayed fashion [46]. Another British study described hand injuries at British Military Hospital in Shaibah, 2004, where 478 of 5614 patients (8.5 %) had hand injuries. Most of the hand traumas were due to noncombat injury (92%), specifically soft tissue injuries. These traumatic injuries occurred most frequently in males, manual workers, combat soldiers, and engineers/mechanics. The authors also found that many patients required periods of restricted duty (52 %) and some required evacuation (8 %), in particular, those patients who required surgery [47].
The US military reports similarly high rates of noncombat-related hand traumas. An analysis of 2007–2009 data from Ibn Sina Hospital in Baghdad, Iraq, demonstrates that of 7520 patients seen, 331 patients had hand injuries, 74 of which required evacuation. The hand trauma mechanisms were mostly related to work accidents, specifically injuries sustained while closing vehicle doors, hatches, and turrets [48].
Hand Fractures
One study out of the 121st Combat Support Hospital in Yongsan, South Korea, describes the incidence of metacarpal fractures. A total of 37 % of musculoskeletal visits to this hospital each week are hand injury related. Between 2006 and 2007, 66 patients presented to the occupational therapy clinic with metacarpal fractures. A high proportion of the patients were single males on their first duty assignments and the mechanism of injury was from striking a person or object out of anger [49]. This is not unlike the demographic and mechanism of these aptly named boxer’s fractures in the general population. Similarly, in men, small finger metacarpal fractures are associated with social deprivation, as the mechanism of injury is often assault or punch injury [50].
Overuse injuries with respect to osseous aspects of the hand are possible as well as manifested in stress fractures. Push-ups can be a source of potential microtrauma that can lead to carpal and metacarpal stress fractures, as noted in a case report [51].
Hand Soft Tissue Injuries
As much as the majority of hand injuries sustained in the military in a noncombat setting are not fractures but soft tissue injuries, specific hand soft tissue injuries are not very well described. One study out of Tripler Army Medical Center describes collateral ligament injury of the thumb metacarpophalangeal (MCP) joint. In a period of 5 years, 56 patients presented with thumb MCP joint instability, and 18 % had a radial collateral ligament injury. The mechanism of injury for radial collateral ligament insuffiency was most likely an axial load injury, whereas for ulnar collateral ligament insufficiency, the mechanism of injury was most likely an abduction–adduction moment. As a whole, the patients with radial collateral ligament injuries were younger and more of them required surgery compared with those in the group presenting with ulnar collateral ligament injuries [52] (67 vs. 40 %).
Part 2: Combat Trauma
Epidemiology of Blast Trauma
The percentage of personnel surviving battlefield injuries continues to increase, most of which is attributable to improvements in protective equipment, evacuation systems, and modern medical treatment. Protective equipment advances have prevented significant amounts of damage due to penetrating abdominal trauma, but the feasibility of protecting extremities to include the lower arm and hand is not readily apparent [53]. Approximately 70 % of battlefield injuries are to the extremities [54]. A lot of these injuries result in high-energy wounds caused by IEDs, mortars, rockets, rocket-propelled grenades, and guns of various types [55, 56]. The wounds are often contaminated and the zone of injury is very large. In case of a high-energy wound, the concern is control of infection, management of soft tissue, timing of definitive fixation, attempting limb salvage, and timing of amputee management [56]. In general, management of these injuries involves meticulous early debridement, control of infection, and wound management with delayed reconstruction [56, 57].
A 2007 analysis of extremity injuries out of the Joint Theater Trauma Registry (JTTR) as a result of combat trauma sustained in OIF and OEF found that from 2001 to 2005, 1281 soldiers sustained 3575 wounds to include 915 fractures; of these, 75 % were from explosive injury; 461, or 50 % of the fractures, were of the upper extremity, with hand fractures being the most common at 36 % [58]. In an analysis of the US Navy/Marine Corps Combat Trauma Registry (CTR) for patients who received treatment for combat wounds in Iraq from 2004 to 2005, out of 665 extremity combat-wounded patients, 261, or 39 %, sustained injuries to the upper extremities, and 181, or 27 %, sustained injuries to both upper and lower extremities. In this analysis, upper extremity wounds were less likely to be coded as serious or fatal by Abbreviated Injury Scale (AIS) scoring [59].
Burn Injuries
Burn injuries comprise 5–20 % of modern combat injuries [60]. In the USA, combat casualty burns are admitted to the US Army Burn Center at Brooke Army Medical Center. From March 2003 through June 2005, 299 OIF/OEF combat casualty burn patients were admitted; of these, 285 survived injury . Of these, 221 (78 %) sustained burn injury to at least one hand, of which 143 (65 %) recovered and returned to duty [61]. In order to combat this, an All Army Activity (ALARACT) message emphasizing the importance of hand protection was disseminated in December 2005, but its efficacy is questioned [62].
Nerve Injuries
Another specific type of injury to note is that of the peripheral nerves. In the British literature, one epidemiological study found 261 peripheral nerve injuries in 100 service members. The most common upper extremity nerve injured was the ulnar nerve. A total of 164 of the injuries sustained were a result of explosions, and 213 were associated with open wounds; in fact, 50 patients sustained major tissue loss [63].
Early Management
In the acute setting , management of these battle injuries entails time-tested principles of early and aggressive debridement, as first widely agreed upon at the Inter-Allied Surgical Conference in 1917. It was at this time that the term “debridement” came into being as meaning incision accompanied by excision of the damaged underlying tissue. In general, this entails excision of the skin margin, generous extension of the wound, exploration through all layers, and excision of damaged muscle [64].
It is important to note that most of these injuries are not isolated. At least 60 % of patients with ballistic trauma to the hand have a concomitant injury elsewhere [65]. After adequate evaluation and prioritization, hand and upper extremity wounds are assessed and managed surgically. The goals of the initial surgery include preservation of vital structures, restoration of viability, and prevention of sepsis. This entails conservative debridement, relief of evolving hematomas, reduction of fractures, and revascularization as feasible. Wounds should be left open. The second surgery should continue to follow principles of maximum preservation of vital structures, and now affords a second look to assess for viability and to set the stage for further reconstructive procedures [66].
There are many similarities between the treatment of blast injuries sustained in the combat environment and current civilian damage control orthopedics. As in civilian traumas, the early administration of antibiotics is key to decreasing infection rates in open fractures and amputations. A key distinction in the deployed environment is that it is important to use broad-spectrum antibiotics for coverage against gram-positive, gram-negative, and anaerobic species [67]. High doses of IV penicillin or, alternatively, erythromycin, chloramphenicol, or a cephalosporin have been recommended to decrease the risk of gas gangrene, which is caused by anaerobic Clostridium species [68]. It is also recommended that all patients receive tetanus toxoid with the addition of antitetanus immunoglobin for those with an unknown immunization status. US military predeployment screening ensures that all active duty soldiers are up-to-date with their immunizations—to include tetanus [69]. In high-grade open fractures, particularly those with large cavitations, the use of a polymethylmethacrylate antibiotic bead pouch is a proposed technique to deliver a high concentration of antibiotics, decrease wound dead space, and reduce bone desiccation until wound coverage is completed.
Another vital aspect of early wound management and evacuation of patients is the advent of negative pressure wound therapy. Many studies have previously found negative pressure wound therapy to be very beneficial as an adjunct to managing open, complex wounds due to better wound granulation, wound contraction, improved control of wound exudates, decreased wound edema, reduced skin maceration, and improved pain management [70–74]. After a study in which 31 enrolled patients with 40 separate wounds flying with such devices had good, predictable outcomes with no increases in wound complications or increases in aircrew workload, these devices are ubiquitous in the management of these wounds at the outset [75]. In fact, a gauze-based, topical, negative-pressure dressing system can be used as a functional splint more efficiently than standard dressings and plaster splints [76].
Negative pressure therapy is used because early wound coverage is often unfeasible due to combat environment and transfer time. In a series of open fractures, Gustilo and Anderson showed a decrease in infection rate from 83 to 18 % when the fractures were covered within 10 days of injury [77]. Unlike civilian injuries, the large amounts of nonviable tissue and deeply impacted debris associated with these blast injuries typically cannot be treated with early wound coverage.
Debridement surgeries should focus on the curettage of contaminated bone ends to remove foreign material, along with the removal of all nonmetallic foreign material and small, devitalized bone fragments, and on the excision of nonviable fat, muscle, and fascia back to healthy tissue [68]. Irrigation and debridement procedures are generally carried out every 24–48 h, and the wound is left open until it is clean and granulation tissue has appeared [67]. Therefore, early stabilization using Kirschner wires, external fixators, or plaster of paris remains the mainstay of fracture care. A recent retrospective review of US military personnel treated with internal fixation within the theater of combat operations reported only one postoperative infection that occurred after a revision internal fixation procedure [24]. However, the authors acknowledged that the treated injuries were less severe than those seen in our current conflicts. Because adequate surgical debridement to allow for definitive fixation and wound closure is not typically available within the combat environment, expedited evacuation to higher echelons of medical care is paramount. Lin et al. reported an average evacuation time of 8.0 days for US soldiers with open fractures [69]. Wound coverage was achieved within an average of 12 days post injury .
Finally, outside of prevention of infection and preparation for definitive wound coverage, early heterotopic ossification (HO) prophylaxis is being taken more into consideration. Nonsteroidal anti-inflammatory medications have not been shown to provide prophylaxis against HO following surgical treatment of elbow traumas [78]. Radiotherapy delivered within 72 h of surgery has shown to be effective in the decrease of HO development at the elbow [79]. Unlike civilian traumas, several contraindications exist to the use of radiotherapy for combat-related injuries; severe systemic polytraumas, open and contaminated wounds requiring serial debridements, and fractures or spine injuries requiring operative stabilization and fusion [80].
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







