2 Elbow Injuries
Pediatric Elbow Injuries in the Throwing Athlete: Emphasis on Prevention
Robert C. Manske, PT, DPT, SCS, MEd, ATC, CSCS, and Mark Stovak, MD
Introduction
Approximately 30 million children and teenagers participate in organized sports in the United States (Adirim and Cheng 2003). Despite the fact that sports are the leading cause of injury in adolescent athletes, it is estimated that more than half of those injuries are preventable (Emery 2003). Pain in the elbow is a common occurrence in young baseball players, especially pitchers. Table 2-1 lists possible differential diagnoses in adolescents with elbow pain. One study found that elbow pain in youth baseball pitchers was associated with multiple factors including age, weight, height, number of pitches thrown during the season, satisfaction with performance, fatigue, lifting weights, and playing outside of the league (Lyman et al. 2001). Studies have found that, during a season, 26% to 35% of youth baseball players have either shoulder or elbow pain, with self-reported shoulder pain in more than 30% of pitchers and elbow pain in more than 25% immediately following a game (Lyman et al. 2001, Lyman et al. 2002). The simple act of throwing is violent because of the stresses it places on the elbow. Because ligaments and muscles are attached to the bone at the medial elbow at a time when the secondary ossification centers are not fused, a traction apophysitis can occur when this growth plate is not able to withstand the forces placed on it. Conversely, compression on the lateral side of the elbow commonly is a cause for Panner’s disease or osteonecrosis of the capitellum.
Table 2-1 Adolescent Elbow Pain Differential Diagnosis
| Locale | Possible Diagnosis | Age (years) |
|---|---|---|
| Lateral | Avascular necrosis of capitellum (Panner’s) | 7–12 |
| Osteochondritis dissecans | 12–16 | |
| Medial | Medial apophysitis (Little Leaguer’s elbow) | 9–12 |
| Medial collateral ligament strain/sprain | All | |
| Flexor/pronator strain | All | |
| Medial epicondyle avulsion | <18 | |
| Ulnar neuritis | All | |
| Posterior | Olecranon apophysitis | |
| Olecranon (posterior) impingement | ||
| Olecranon osteochondrosis | ||
| Triceps/olecranon tip avulsions | ||
| Other | Fracture | All |
| Loose bodies | >18 | |
| Synovitis | All |
Little Leaguer’s elbow
Little Leaguer’s elbow is considered a host of elbow pathology in a young throwing athlete. The various types of injuries that can be considered Little Leaguer’s elbow are listed in Table 2-2.
Table 2-2 Forms of Little Leaguer’s Elbow
| Medial epicondyle fragmentation |
| Medial epicondyle avulsion |
| Delayed apophyseal growth of medial epicondyle |
| Accelerated apophyseal growth of medial epicondyle |
| Delayed closure of the medial epicondylar apophysis |
| Delayed closure of the olecranon apophysis |
| Osteochondrosis of the capitellum |
| Osteochondritis of the capitellum |
| Osteochondrosis of the radial head |
| Osteochondritis of the radial head |
| Hypertrophy of the ulna |
| Olecranon apophysitis |
Medial tension injuries
Medial tension injuries most commonly include medial epicondylar apophysitis. With repetitive stress to the medial elbow in the throwing adolescent, the flexor pronator mass and the ulnar collateral ligament apply tensile forces that cause medial epicondyle apophysitis (Pappas 1982, Rudzki and Paletta 2004). This apophysitis is thought to occur rather than rupture of the ulnar collateral ligament (Joyce et al. 1995). Chronic attritional tears of the ulnar collateral ligament are fairly rare in adolescent athletes (Ireland and Andrews 1988). Despite this rarity, it appears that ulnar collateral injuries are increasing in high school athletes. Petty et al. (2004) reported that the percentage of high school athletes who required ulnar collateral ligament reconstruction in their center jumped from 8% between 1988 and 1994 to 13% between 1995 and mid-2003. Injuries to the ulnar collateral ligament in adolescent athletes generally occur as acute events, rather than through attrition as in older, more skeletally mature athletes.
Lateral compression injuries
Several conditions caused by compression of the lateral side of the elbow can occur in younger pitchers. Two of the more common are osteochondritis dissecans (OCD) and Panner’s disease. Although traditionally these have been thought to be the same condition by some, they are separate entities. Osteochondritis is a localized condition involving articular cartilage that has separated from the underlying subchondral bone and is caused by repetitive trauma (Yadao et al. 2004). Panner’s disease is a focal osteonecrosis of the entire capitellum seen primarily in boys aged 7 to 12 years old and is not associated with trauma (Yadao et al. 2004).
Posterior compression injuries
Whereas medial and lateral elbow pain occurs as a result of “valgus extension overload” during the late cocking–early acceleration phase of throwing, posterior pain occurs during the terminal phase of throwing as the elbow is locked into full extension. The synovium can be pinched in the olecranon when the elbow is in full extension, resulting in posterior impingement syndrome, or the posterior apophysis can be stressed by triceps traction, causing olecranon apophysitis (Crowther 2009).
Prevention
Several associations have provided recommendations regarding adolescent athletes and prevention of both elbow and shoulder problems. The American Academy of Pediatrics and USA Baseball each have guidelines regarding pitch counts. The American Academy of Pediatrics recommends limits of 200 pitches per week or 90 per outing, while the USA Baseball Medical and Safety Advisory Committee recommends a more stringent 75 to 125 pitches per week or 50 to 75 pitches per outing depending on age (Committee on Sports Medicine and Fitness, USA Baseball Medical and Safety Advisory Committee 2001).
USA baseball guidelines
Pitch Counts
Pitch counts should be carefully monitored and regulated in adolescents. Recommended limits vary depending on age of the pitcher (Table 2-3).
Table 2-3 USA Baseball Recommended Pitch Counts
| Age (yrs) | 2006 USA Baseball Guidelines | 2010 Little League Baseball Regulations |
|---|---|---|
| Daily limits | ||
| 17–18 | n/a | 105/day |
| 15–16 | n/a | 95/day |
| 13–14 | 75/game | |
| 11–12 | 75/game | 85/day |
| 9–10 | 50/game | 75/day |
| 7–8 | n/a | 50/day |
| Weekly limits | ||
| 13–14 | 125/wk; 1000/season; 3000/yr | |
| 11–12 | 100/wk; 1000/season; 3000/yr | |
| 9–10 | 75/wk; 1000/season; 2000/yr | |
| 7–18 | ||
Additionally, pitchers 16 years of age or younger must adhere to the following rest requirements:
Pitchers 17 to 18 years of age should adhere to the following rest requirements:
Pitch Types
Because the risk of injury from throwing breaking pitches is increased in the adolescent athlete, curveballs and sliders are not recommended (Lyman et al 2002). These pitches become even more problematic when the athlete does not exhibit adequate throwing mechanics. Recommended ages to learn types of pitches are listed in Table 2-4.
Table 2-4 Recommended Age to Learn Pitches
| Pitch | Age |
|---|---|
| Fastball | 8–10 |
| Change-up | 10 |
| Curveball | 14 |
| Knuckleball | 14 |
| Slider | 16–18 |
| Forkball | 16–18 |
| Splitter | 16–18 |
| Screwball | 17–18 |
USA Baseball Medical and Safety Advisory Committee.
Medial Collateral Ligament and Ulnar Nerve Injury at the Elbow
Michael Levinson, PT, CSCS, and David W. Altchek, MD
Anatomy and biomechanics
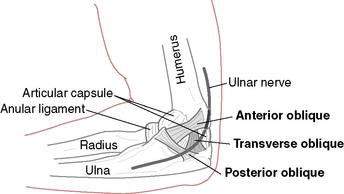
The MCL is composed of two primary bundles. The anterior bundle runs from the sublime tubercle of the ulna and inserts on the inferior surface of the medial epicondyle. The anterior bundle tightens in extension and loosens in flexion. The posterior band runs from the posterior portion of the medial epicondyle and inserts at the ulna proximal and posterior to the sublime tubercle (Fig. 2-1). The posterior bundle tightens in flexion and loosens in extension. The anterior bundle is the prime focus of the MCL reconstruction. The ulnar nerve runs in the space posterior to the medial epicondyle. The space is referred to as the cubital tunnel. The roof of the tunnel is referred to as the cubital tunnel retinaculum. At this location, the nerve is significantly exposed.
Mechanism of injury
Injury to the MCL is a result of the repetitive, extreme valgus loads to the elbow while throwing. The MCL is the primary restraint to valgus stress at the elbow. Dillman et al. (1995) demonstrated that a fastball thrown by an elite baseball pitcher produces a load that approaches the actual tensile strength of the MCL. The MCL attempts to withstand these forces during the late cocking and acceleration phases of throwing. Repetitive overloading can result in inflammation and microtears of the ligament, which can eventually lead to failure. Continuing to throw with instability can lead to degenerative changes in the elbow.
Surgical treatment
Medial Collateral Ligament Reconstruction
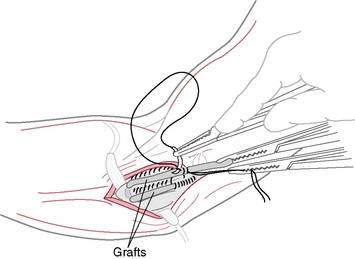
Reconstruction of the medial collateral ligament is performed using the “docking technique” described by Altchek et al. (2000). The anterior bundle is the primary focus of the reconstruction. The ipsilateral palmaris longus is the graft of choice. In the absence of this muscle, the gracilus is used. Our rehabilitation guidelines are not affected by graft choice; however, when using the gracilis, the affected lower extremity must be considered.
This procedure includes a routine arthroscopic evaluation of the elbow through a muscle-splitting approach that preserves the flexor–pronator origin (Fig. 2-2). Bone tunnels are created in the humerus and ulna. The graft is “docked” securely in the tunnels with sutures (Fig. 2-3). This technique also minimizes the number of tunnels and reduces the size of the drill holes. Finally, this technique avoids an obligatory ulnar nerve transposition.
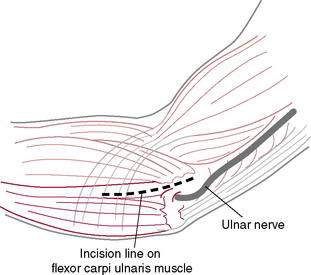
Figure 2-2 Exposure is created by splitting the flexor carpi ulnaris muscle.
(Redrawn from Levinson M: Ulnar Collateral Reconstruction in Postsurgical Rehabilitation Guidelines for the Orthopedic Clinician. 1st edition, St. Louis, Elsevier, 2006.)
Rehabilitation Overview and Principles
The rehabilitation program following MCL reconstruction is based on the healing restraints and functional demands of the graft (Rehabilitation Protocol 2-1). Time frames for returning to certain activities are based on allowing the graft to both strengthen adequately and regain adequate flexibility. The program features early, safe range of motion (ROM) to allow optimal tissue healing and minimize the effects of immobilization. Elbow ROM in a hinged brace is initiated after 1 week to prevent contracture, provide pain control, enhance collagen formation, and nourish articular cartilage. Range of motion is increased gradually in the brace over the initial 6-week postoperative period. Aggressive, passive stretching should be avoided throughout rehabilitation. Elbow extension is restored using a low-load, long-duration stretch, which has been demonstrated to be an effective method for restoring range of motion.
REHABILITATION PROTOCOL 2-1 Medial Collateral Ligament Reconstruction Guidelines
Rehabilitation following ulnar nerve transposition follows the same progression as the MCL reconstruction; however, the progression is generally shorter (Rehabilitation Protocol 2-2). The brace is discontinued after 3 weeks, at which time a formal strengthening program is begun. A throwing program normally can be initiated at 10 to 12 weeks.
Conservative Treatment of Medial Collateral Ligament Injuries
As mentioned previously, improved operative techniques and rehabilitation guidelines have made surgical intervention the treatment of choice, especially for throwing athletes. Little scientific data exist to support conservative treatment, especially in competitive throwers, for return to pre-injury activity level. However, at times conservative treatment may be an option (Rehabilitation Protocol 2-3).
REHABILITATION PROTOCOL 2-3 Conservative Medial Collateral Ligament Injury Guidelines
Treating Flexion Contracture (Loss of Extension) in Throwing Athletes
Tigran Garabekyan, MD, and Charles E. Giangarra, MD
Recommended criteria for a safe return to sports include
See Rehabilitation Protocol 2-4 for the treatment protocol following elbow arthroscopy.
REHABILITATION PROTOCOL 2-4 After Elbow Arthroscopy
Phase 2: Intermediate Phase
Post-Traumatic Elbow Stiffness
Daniel Woods, MD, and Charles E. Giangarra, MD
Classification
The etiology of elbow stiffness has been classified by various authors. Kay (1998) based his scheme on the anatomic components involved. Type I involves soft tissue contractures; type II involves soft tissue contractures with ossification; type III involves nondisplaced articular fracture with soft tissue contracture; type IV involves displaced intra-articular fractures with soft tissue contracture; and type V involves post-traumatic bony bars blocking elbow motion.
Morrey (1990) classified elbow stiffness into intrinsic, extrinsic, and mixed causes (Table 2-5). Intrinsic causes are related to intra-articular pathology resulting from deformities or malalignment of the articular surface, intra-articular adhesions, loose bodies, impinging osteophytes, and fibrosis within the olecranon or coronoid fossa. Extrinsic causes are related to all entities aside from the articular surface. Examples include skin contracture from scars or burns, capsular and collateral ligament contracture, and heterotopic ossification. Another important extrinsic cause is injury to brachialis or triceps resulting in a hemarthrosis, which may cause scarring, fibrosis, and limitation of motion. Entrapment of the ulnar nerve can lead to pain resulting in loss of motion and eventual capsular contracture. Mixed etiologies are defined as extrinsic contractures resulting from intrinsic pathology.
Table 2-5 Morrey’s Causes of Elbow Stiffness by Location of Pathology
| Extrinsic |
| Intrinsic |
Heterotopic ossification
Heterotopic ossification (HO) is an important cause of post-traumatic stiffness of the elbow. Direct trauma, neural axis injury, surgical intervention, and forceful passive manipulation may cause HO, which is directly related to the severity of the initial injury. Noted radiographically approximately 4 to 6 weeks following the event, HO presents with swelling, hyperemia, and loss of motion of the affected joint. HO in the upper extremity has been classified by Hastings and Graham (1994) into three types: I, without functional limitation, II, subtotal limitation, and III, complete bony ankylosis (Table 2-6). Treatment consists of physical therapy and indomethacin or a diphosphonate to begin shortly after the insult. If HO continues to progress, surgical excision of the heterotopic bone when the hyperemia and swelling begin to diminish is indicated. When the HO matures, prompt surgical treatment is important to avoid soft-tissue contractures that may result from prolonged loss of motion.
Table 2-6 Heterotopic Ossification Classification: Upper Extremity
| Class | Description |
|---|---|
| I | Without functional limitation |
| II | Subtotal limitation |
| IIA | Limitation in flexion/extension |
| IIB | Limitation in pronation/supination |
| IIC | Limitation in both planes of motion |
| III | Complete bony ankylosis |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree