Elbow Arthroscopy for Panner Disease and Osteochondritis Dissecans
Theodore J. Ganley
Christine M. Goodbody
J. Todd R. Lawrence
R. Jay Lee
DEFINITION
Panner Disease
Panner disease is a condition in which there is compromised subchondral bone, potentially due to repetitive microtrauma and diminished blood supply to the developing ossific nucleus within the distal humerus chondral epiphysis in preadolescents.9
Those affected are typically 6 to 10 years old, and symptoms usually respond to a reduction of the offending repetitive microtrauma.9
Osteochondritis Dissecans of the Capitellum
This term is used to describe the condition of compromised subchondral bone in the capitellum of adolescents, which can lead to secondary articular surface separation.8
Osteochondritis dissecans (OCD) of the capitellum is most commonly seen in children ages 10 to 17 years old, particularly those who engage in overhead throwing sports and activities in which the elbow serves as a loadbearing joint.
ANATOMY
The three articulations in the elbow are the ulnohumeral joint, the radiocapitellar joint, and the proximal radioulnar joint.
The ulnohumeral joint is a hinge joint that allows for flexion and extension of the elbow, whereas the radiocapitellar and radioulnar joints are trochoid joints that allow for axial rotation and pivoting of the elbow.
The capitellum articulates with the rim of the radial head throughout flexion-extension and pronation-supination.
Secondary ossification centers are involved in the formation of the distal humerus, proximal radius, and ulna. The ossification center of the capitellum appears at 18 months and completely fuses by age 14 years.
Descending extraosseous branches of the brachial artery supply the capitellum. Chondral vessels supply the osseous nucleus, which in turn supplies the chondroepiphysis.
PATHOGENESIS
It is theorized that both Panner disease and OCD of the capitellum arise from repetitive submaximal stresses, which in summation result in abnormal valgus forces exerted across the radiocapitellar joint.3,4,11,13
The result of this abnormal stress on the radiocapitellar joint may depend on the age of the patient, with those exposed to the stress at a younger age (6 to 10 years) developing Panner disease and those exposed to the stress at a later age (10 to 17 years) developing OCD of the capitellum.
The development of the lesions also depends on the limited blood supply of the capitellum, which allows for limited repair potential.
NATURAL HISTORY
With activity restriction, reossification and resolution of symptoms typically occur in Panner disease.7
The natural history of OCD is articular surface separation for patients who do not restrict their activities. Even with activity modification and brief periods of immobilization, elbow OCD lesions will progress in most patients treated nonoperatively.
In OCD of the capitellum, radiographs will initially show irregularity and fragmentation of the capitellum. Erosion, lysis, and sclerosis may be observed in later stages.
PATIENT HISTORY AND PHYSICAL FINDINGS
Early stages
Patients have full motion but complain of vague aching lateral elbow discomfort during throwing and load-bearing activities as well as swelling at the lateral elbow. They typically have full range of motion.
Synovitis: occasional mild palpable effusion
Later stages: Patients complain of mechanical symptoms, including locking and catching, and limited flexion and extension.
Examination may reveal palpable synovial thickening, elbow effusion, decreased range of motion, and tenderness over the radiocapitellar joint.
IMAGING AND OTHER DIAGNOSTIC STUDIES
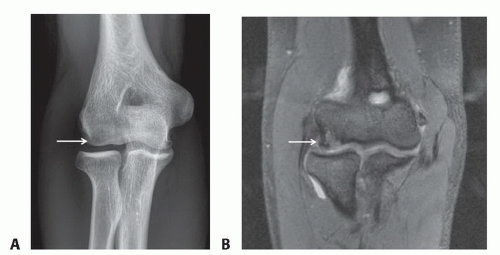
Anteroposterior (AP) and lateral radiographs of the elbow are needed to evaluate both conditions. In Panner disease, the size of the ossific nucleus and the degree of radiolucency can be determined from the radiographs. In OCD lesions, fragmentation, erosion, subchondral lysis, or cystic changes may be seen on radiographs (FIG 1A).
Magnetic resonance imaging (MRI) findings in OCD may reveal bone edema, synovitis, and loose bodies as well as subchondral and cartilage separation (FIG 1B).
DIFFERENTIAL DIAGNOSIS
Familial OCD
Hemophilia and variants
Multiple epiphyseal dysplasia
Autoimmune vasculitis
Steroid-induced avascular necrosis
NONOPERATIVE MANAGEMENT
Treatment for Panner disease consists of the following:
Sling for 4 to 6 weeks
Range-of-motion exercises
Cessation of all offending activity
Follow-up radiographs through resorption and reconstitution phases at 3-month intervals prior to resumption of sport-specific exercises.
Nonoperative treatment of OCD is reserved for cases in which the cartilage is intact. It consists of the following:
Immobilization in a posterior splint or sling for 6 weeks
Removal of the splint or sling for a few minutes several times per day to perform range-of-motion exercises
Rest until symptoms resolve
Follow-up radiographs through resorption and reconstitution phases prior to resumption of sport-specific exercises
SURGICAL MANAGEMENT
Surgical management is largely dependent on the character of the lytic lesion (stable vs. unstable, intact vs. partially or completely detached articular cartilage) and the presence or absence of symptoms.
Surgery is generally reserved for unstable lesions with partially or completely detached articular cartilage.
Persistent pain and swelling despite intact cartilage may warrant arthroscopic evaluation with a search for loose bodies as well as consideration of lesion drilling to stimulate subchondral bone healing.
Preoperative Planning
All imaging studies obtained before surgery should be reviewed. An MRI may be helpful to determine the extent of the lesion and the location and size of chondral or small osteochondral loose bodies in the joint.
A thorough physical examination should be performed under anesthesia to note range of motion and appropriate or pathologic degrees of laxity.
Positioning
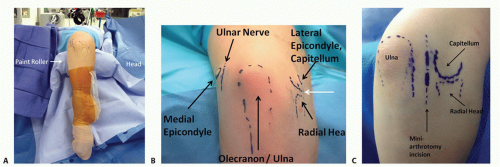
The patient is adequately padded and placed in the lateral decubitus position.
The involved elbow is placed over a padded bump that places the elbow in 90 degrees of flexion.
The extremity is then prepared and draped, allowing unhindered flexion and extension of the elbow and internal and external rotation of the shoulder (FIG 2A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree