I. RUPTURES OF THE DISTAL BICEPS BRACHII
A. Anatomy. Rupture of the distal biceps may occur at the muscle tendon junction or more commonly at its tendinous insertion into the radial tuberosity.
B. Mechanism of injury. This injury typically occurs in men 30 to 60 years old. Most patients report pain or a tearing sensation in the antecubital fossa after elbow flexion against resistance.
C. Examination. In a normal elbow, the biceps tendon should be easy to identify and palpate. Inability to “hook” the finger under the lateral edge of the biceps tendon strongly suggests biceps tendon rupture.1 Because other muscles contribute to elbow flexion, the patient demonstrates minimal elbow flexion weakness, but does have weakness to forearm supination. With an intact biceps tendon, squeezing the biceps muscle belly in the upper arm should produce supination of the forearm. Absence of supination with the “squeeze test” suggests distal biceps tendon rupture.2
D. Radiographs. Routine elbow radiographs occasionally reveal small bony avulsions from the radial tuberosity, but most often show no abnormalities. If the diagnosis is not clear clinically, MRI of the elbow can identify biceps tendon rupture (Fig. 19-1).
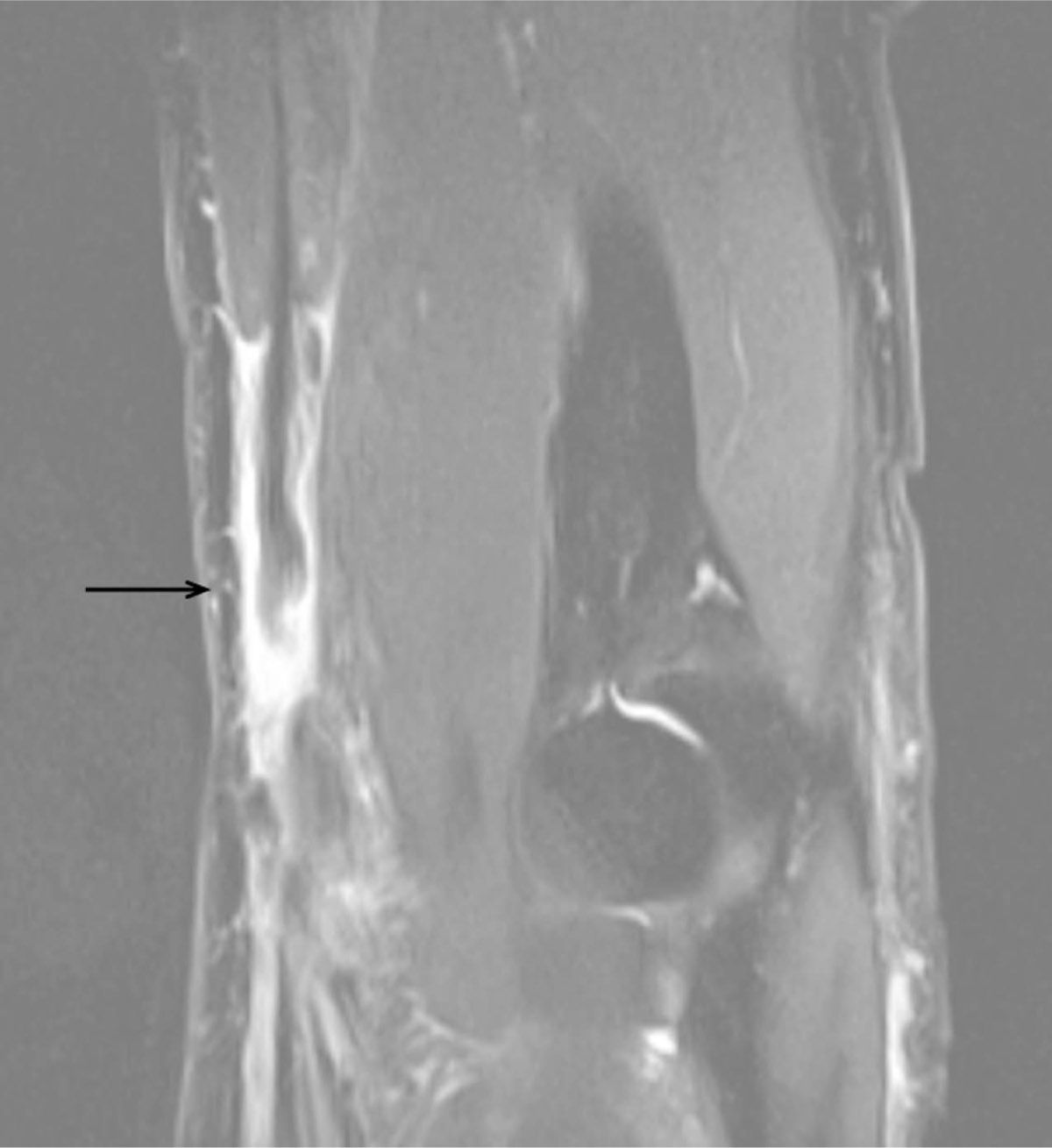
Figure 19-1. Sagittal section MRI of the elbow of a 64-year-old man who had pain and swelling at the elbow after tripping over a treadmill. The arrow indicates the distal end of the biceps tendon (black) that has retracted surrounded by fluid.
E. Treatment. Treatment of distal tendon tears is controversial. The biceps functions as a weak elbow flexor and a strong forearm supinator, and patients who do not have the tendon repaired do lose some forearm supination strength.3 Active, otherwise healthy, individuals may wish to undergo surgical repair. Tendon repair is technically easier, and results are better if performed within 3 weeks of the injury. Therefore, patients who may be operative candidates should be referred promptly to an orthopaedic surgeon. Surgeons employ various tendon repair techniques, typically followed by 6 to 8 weeks of rehabilitation.4
F. Complications. Complications of surgical repair include heterotopic ossification and synostosis, loss of forearm rotation, and nerve injury.
II. DISLOCATION OF THE ELBOW JOINT accounts for 20% of all dislocations, second only to glenohumeral and interphalangeal joint dislocations.
A. Anatomy. Dislocation of the ulnohumeral joint most commonly occurs in a posterior direction and can result in disruption of the elbow capsule, the medial and collateral ligaments, and the muscles originating from the medial and lateral epicondyles. O’Driscoll et al.5 has described the mechanism of the typical elbow dislocation as starting with disruption of the lateral collateral ligament complex, extending through the anterior and posterior capsule, and only disrupting the medial collateral ligament in the most severe cases (the circle of Horii).
B. Mechanism of injury. Elbow dislocation usually results from a fall on an outstretched arm.
C. Examination. The elbow typically appears very swollen, and the patient is unable to actively move the joint. In the examination of an injured elbow, there may be confusion about whether the deformity arises from a dislocation of the elbow or from a supracondylar fracture, but this can be resolved clinically by comparing the relative positions of the two epicondyles and the tip of the olecranon by palpation. These three bony points form an isosceles triangle. The two sides remain equal in length in a supracondylar fracture. If the elbow is dislocated, however, the two sides become unequal (Fig. 19-2). The position of the proximal radius can be palpated on the lateral surface of the elbow to rule out radial head dislocation. The function of the peripheral nerves and the state of the circulation to the hand, including capillary refill and presence of radial pulse, should be carefully noted. Nerve injuries, most commonly involving the ulnar nerve, occur in 1% to 17% of elbow dislocations.6 Brachial artery injury is rare, but can have devastating consequences if not promptly recognized and treated.
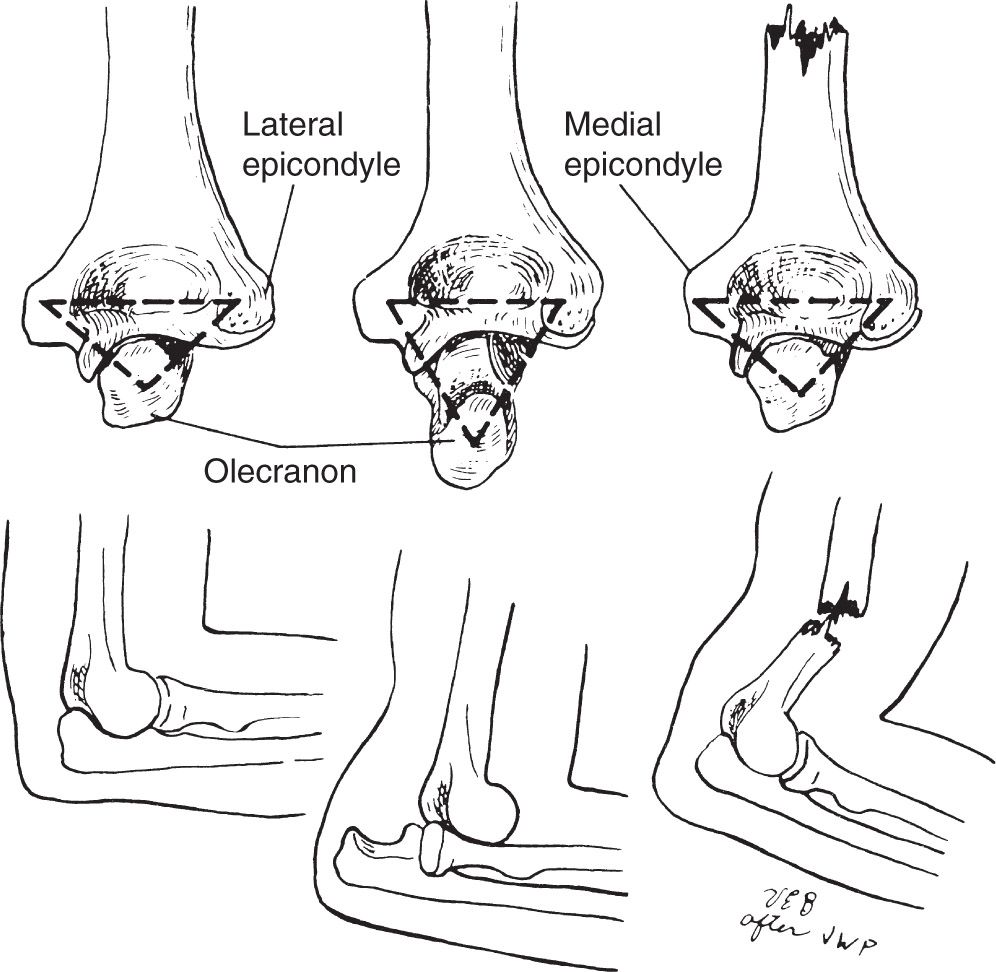
Figure 19-2. The two epicondyles and the tip of the olecranon form an isosceles triangle. This triangle is maintained with a supracondylar humeral fracture, but with an elbow dislocation, the two sides of the triangle become unequal or distorted.
D. Radiographs. Radiographs should include anteroposterior and lateral views of the elbow, an anteroposterior view of the humerus, and an anteroposterior view of the forearm. Imaging of the elbow demonstrates whether the displacement is directly posterior (Fig. 19-3), posterolateral, or posteromedial. Fractures of the coronoid process have been identified in 10% to 15% of elbow dislocations. Fractures involving the distal humerus, proximal ulna, or radial head signify a more complex injury that typically requires operative intervention.

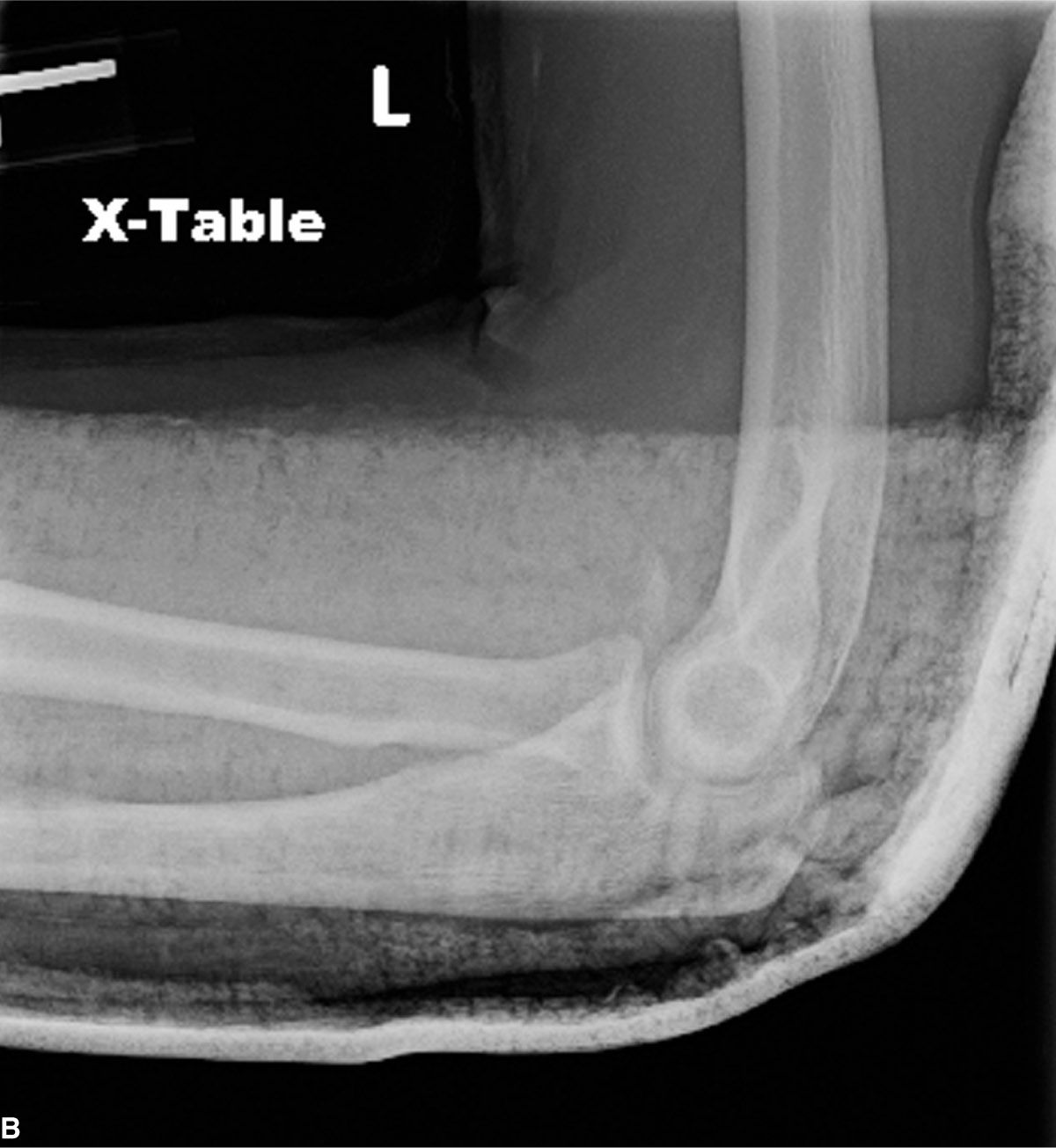
Figure 19-3. A: This lateral radiograph of the elbow of a 21-year-old man demonstrates a posterior dislocation of the elbow following a snowboarding injury. B: The elbow is concentric following closed reduction. The patient started elbow motion 5 days after injury, and ultimately obtained motion from 0° to 145° of flexion.
E. Treatment. All elbow dislocations should be initially managed with closed reduction, which can often be performed in the emergency room setting. Sedation may be necessary for proper muscle relaxation. Reduction can usually be achieved by exerting gentle traction on the slightly flexed elbow while applying countertraction to the humeral shaft. Postreduction AP and lateral elbow radiographs are mandatory to confirm congruent reduction. After reduction, the examiner should document the arc of flexion through which the elbow remains stable. This can be determined by examining the elbow fluoroscopically throughout flexion and extension and determining at what degree of extension the joint begins to subluxate. Alternatively, the elbow can be gently taken through flexion and extension, and the patient asked to report when they feel the joint becoming unstable (apprehension). The elbow should be placed in a posterior splint in 80° to 90° of flexion with the forearm in neutral. The patient should be seen within 3 to 5 days with repeat radiographs to confirm reduction and to initiate range of motion exercises.7
If the elbow joint cannot be reduced, there may be interposed soft-tissue or bone fragments and open reduction and ligament repair will be necessary. Combination elbow fracture/dislocations almost always require open reduction with internal fixation (ORIF).
F. Complications
- Limited range of motion. Early initiation of active range of motion (within 5 days) has been shown to improve final range of motion.7
- Heterotopic ossification can develop, and its treatment should follow the guidelines in Chapter 3, I. Posttraumatic elbow stiffness can be successfully treated by open release.8 If associated with postresection instability, a hinged external fixator can be used with good results in motivated patients.9
- Recurrent instability can be difficult to diagnose; when recognized, surgical reconstruction can be successful.5
III. FRACTURES OF THE OLECRANON
A. Anatomy. Olecranon fractures may be simple transverse, comminuted, displaced, or nondisplaced. The triceps tendon inserts into the proximal olecranon, and displaced fractures of the olecranon result in inability to actively extend the elbow.
B. Mechanism of injury. Olecranon fractures can occur as the result of a fall directly onto the elbow or activation of the triceps against resistance.
C. Physical examination. There is often swelling and ecchymosis over the fracture site. If the fracture is not displaced on radiographs and nonoperative treatment is a consideration, the patient’s ability to actively extend the elbow should be assessed. Associated neurovascular injuries are uncommon.
D. Radiographs. AP and lateral radiographs of the elbow typically demonstrate the fracture.
E. Treatment.
- Nondisplaced fractures with intact triceps function should be treated in a posterior splint with the elbow flexed 90°. Pronation and supination movements are started in 2 to 3 days, and flexion–extension movements are started at 2 weeks. Protective splinting or a sling is used until there is evidence of union (usually around 6 weeks). Close clinical and radiographic follow-up is essential to ensure full ROM and to identify any displacement.
- Displaced fractures should be reduced anatomically and fixed internally with tension band wiring or plate fixation. Fixation should be secure enough to allow early motion. In some instances where the proximal fragment is small, fragment excision and triceps advancement can be considered.
F. Complications.
- Symptomatic hardware. Regardless of whether a plate or tension band wiring is used for fixation, the hardware is often prominent in the subcutaneous tissue overlying the olecranon.
- Loss of motion. Even patients with simple fractures fixed anatomically often lose 10° to 15° of extension. Functional range of motion from 30° to 110° of flexion meets the needs for ADLs for most patients.
IV. EPIPHYSEAL FRACTURES OF THE PROXIMAL RADIUS
A. Anatomy. Ossification of the radial head epiphysis typically appears around the age of 5.
B. Mechanism of injury. These injuries result from a fall on the outstretched hand in children and adolescents ages 6 to 16.
C. Examination. Pain, occasionally swelling, and tenderness are usually present over the proximal end of the radius. There is also limitation of elbow motion. The wrist should also be carefully examined for evidence of injury to the distal radius and/or distal radioulnar joint.
D. Radiographs: AP and lateral radiographs of the elbow often demonstrate the abnormality. Radiographs of the forearm and/or wrist should be obtained in children to rule out any associated injuries. However, due to the differing appearance of elbow epiphyses as the skeleton matures, images of the contralateral uninjured elbow may be helpful in cases where the diagnosis is not clear.
E. Treatment.
- Fractures with less than 15° of angulation are immobilized in a long-arm splint for 1 to 2 weeks. Active exercise is then initiated while the arm is protected in a sling.
- Angulation of greater than 15° calls for manipulation under anesthesia. If this fails, operative reduction is required. These fractures can often be reduced with the aid of an intramedullary wire as described by Metaizeau.10 After reduction, the intramedullary pin is left in place for about 8 weeks, although active motion exercises for the elbow can begin 2 weeks after surgery. The radial head should never be removed in children.
V. FRACTURES OF THE RADIAL HEAD AND NECK IN ADULTS
A. Anatomy. The radial head articulates with both the capitellum of the distal humerus and the proximal ulna. It also contributes to elbow stability against valgus loads.
B. Mechanism of injury. This common injury should be suspected following a fall on the outstretched hand whenever there is swelling of the elbow joint, tenderness over the head of the radius, and limitation of elbow motion (especially painful pronation and supination).
C. Physical examination. Patients with radial head fractures typically present with tenderness directly over the radial head and limited elbow motion. More comminuted or displaced radial head fractures may cause crepitus with pronation and supination. The examiner should document any other areas of elbow tenderness, as medial elbow tenderness may indicate a more severe elbow injury with instability. Be careful to also examine the wrist and forearm for tenderness, as radial head fractures are associated with Essex-Lopresti injuries (disruption of the interosseous membrane of the forearm).
D. Radiographs. If the fracture is not apparent on anteroposterior and lateral elbow radiographs, a radial head view may demonstrate the injury. A posterior and/or large anterior fat pad sign, indicative of an elbow effusion, should raise suspicion of a radial head fracture. Fractures are often described using the modified Mason classification.
- Mason 1: Nondisplaced fracture of the radial head.
- Mason 2: Partial articular fracture with greater than 2 mm of displacement.
- Mason 3: Fracture involving the entire radial head, splitting into two or more fragments. In the Hotchkiss11 modification of the Mason classification, type 3 fractures are defined as head fractures too comminuted to allow for open reduction internal fixation.
- Mason 4: Fracture of the radial head associated with an elbow dislocation. The Mason 4 is an additional category proposed by Johnston12 and utilized by some practitioners.
- Minimally displaced (<1 mm) fractures of the head (Mason 1) or impacted fractures of the radial neck may be placed in a posterior splint for comfort at the time of injury, but elbow motion exercises should be initiated within 3 to 5 days. Early active motion increases the final range of motion (particularly elbow extension) and improves outcome.
- Management of Mason 2 fractures of the radial head depends on the size and number of the fracture fragments, the degree of displacement, associated injuries, and the patient’s elbow range of motion. Fractures involving less than one-third of the articular surface can be managed with early motion if the patient is able to move through a full arc of pronation and supination. If the patient cannot pronosupinate because of pain, aspiration of the elbow effusion and injection of 5 mL of 1% lidocaine can relieve pain and allow better assessment of true range of motion.
Open reduction internal fixation should be considered for displaced fractures involving more than 30% of the articular surface. Hardware can be placed in a “safe zone” on the radial head that corresponds to the 90° arc between the radial styloid and Lister’s tubercle.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








