Abstract
Objective
To assess, in obese type 2 diabetics (T2D), the impact of a home-based effort training program and the barriers to physical activity (PA) practice.
Method
Twenty-three obese T2D patients (52.7 ± 8.2 years, BMI = 38.5 ± 7.6 kg/m 2 ) were randomized to either a control group (CG), or an intervention group (IG) performing home-based cyclergometer training during 3 months, 30 min/day, with a monthly-supervised session. The initial and final measurements included: maximal graded effort test on cyclergometer, 6-minute walk test (6MWT) and 200-meter fast walk test (200mFWT), quadriceps maximal isometric strength, blood tests and quality of life assessment (SF- 36). A long-term assessment of the amount of physical activity (PA) and the barriers to PA practice was conducted using a questionnaire by phone call.
Results
Patients in the CG significantly improved the maximal power developed at the peak of the cyclergometer effort test ( P < 0.05) as well as the quadriceps strength ( P < 0.01). There were no significant changes in the other physical and biological parameters, neither in quality of life. At a mean distance of 17 ± 6.4 months, the PA score remained low in the two groups. The main barriers to PA practice identified in both groups were the perception of a low exercise capacity and a poor tolerance to effort, lack of motivation, and the existence of pain associated to PA.
Conclusion
This home-based intervention had a positive impact on biometrics and physical ability in the short term in obese T2D patients, but limited effects in the long term. The questionnaires completed at a distance suggest considering educational strategies to increase the motivation and compliance of these patients.
Résumé
Objectif
Évaluer, chez des diabétiques de type 2 (DT2) obèses, l’impact d’un programme de réentraînement à l’effort à domicile et les freins à la pratique de l’activité physique (AP).
Méthode
Vingt-trois DT2 obèses (52,7 ± 8,2 ans, IMC = 38,5 ± 7,6 kg/m 2 ) ont été randomisés dans un groupe témoin (GT) ou un groupe s’entraînant à domicile sur cycloergomètre 3 mois, 30 minutes/j, avec une séance mensuelle supervisée (GE). Les mesures initiales et finales comportaient : un test d’effort incrémental maximal sur cycloergomètre, des tests de marche de six minutes et 200 m, la force maximale isométrique du quadriceps, un bilan biologique et une évaluation de la qualité de vie (échelle SF-36). À distance, une évaluation de l’AP et des freins à sa pratique a été effectuée par questionnaire téléphonique.
Résultats
Les patients du GE ont significativement plus amélioré la puissance développée au pic de l’effort lors du test sur cycloergomètre ( p < 0,05) ainsi que la force du quadriceps ( p < 0,01). Il n’existait pas de modifications significatives des autres paramètres physiques, biologiques, et de la qualité de vie. Le score d’AP à 17 ± 6,4 mois est resté faible dans les deux groupes. Les freins principaux à la pratique d’AP étaient la perception d’une faible capacité et d’une mauvaise tolérance à l’effort, le manque de motivation, l’existence de douleurs liées à l’AP.
Conclusion
Cet entraînement à domicile a eu un impact positif sur la biométrie et les capacités physiques à court terme chez des patients DT2 obèses, mais des effets limités à long terme. Les questionnaires réalisés à distance permettent d’envisager des stratégies éducatives pour augmenter la motivation et l’observance de ces patients.
1
English version
1.1
Introduction
A sedentary way of life has been clearly identified as a major risk factor of appearance or progression of type 2 diabetes . Regular practice of physical activity (PA) is therefore part of the current recommendations in preventing type 2 diabetes and in the treatment of patients with diabetes . The mechanisms of action of PA are well established, as well as its efficacy in terms of prevention of diabetes-related complications . However, it appears that the practice of PA is insufficient in these patients and that education programs need to be developed. The factors limiting the practice of physical activity during type 2 diabetes are multiple in these patients who are often in a spiral of physical inactivity, a source of effort deconditioning . The reasons of this sedentary way of life are multiple , at the same time physical (associated co-morbidities such as peripheral arterial disease, neuropathy, plantar ulcers, arthrosis ), psychosocial (mood disturbance , lack of family support, erroneous representations of physical activity ), environmental (work-related constraints, distance from the structures allowing PA practice), and financial . They can participate in the lack of motivation for physical activity often reported by these patients. Their assessment may allow better a understanding of the limits for a regular PA practice, and guiding the educative proposals made to diabetic patients in the frame of an adapted PA . In France, for the patients with type 2 diabetes, the rehabilitation programs including supervised effort training are generally proposed subsequently to an acute cardiovascular event only. They are less frequently proposed in a situation of primary cardiovascular prevention where most often a conventional educative approach is realized, including counsel regarding physical activity, sometimes associated with a practical session of PA. This situation is partly due to the lack of human means and of specialized technical capacity, not allowing proposing supervised PA sessions to a large number of diabetic patients. In view of the extent of the type 2 diabetes “epidemic”, efficient alternatives in socioeconomic terms must be proposed. The practice of home-based PA programs represents an interesting alternative, as it was shown by a program started at the hospital and continued at home . These programs should at least include aerobic exercise sessions of moderate intensity of 30 min, 5 days a week, in order to control weight and to improve the glycemic status, and if possible light muscular reinforcement exercises learnt under initial supervision . The objectives of this work were:
- •
to assess the impact of a tailored program of 3-month home-based effort training in patients with type 2 diabetes in primary cardiovascular prevention: at short term, on the anthropometric, biological parameters, on the effort capacities, and on quality if life; and at long term, on the habits of regular PA practice;
- •
to list the main barriers to regular PA practice reported by the patients, as well as the ways to improve compliance to a regular PA practice.
1.2
Material and methods
This was a randomized, prospective, monocentric study. This project received a grant within the framework of a clinical research hospital protocol no. 2002-0256, and obtained the agreement of the Committee for the protection of persons participating to biomedical research.
1.2.1
Patients
This protocol was proposed to patients with type 2 diabetes confirmed at least one year earlier, followed-up for check-up in the Diabetology department of the Dijon University Hospital, men and women, aged 40 to 70 years. Inclusion criteria were: associated neuro-orthopedic deficiency making the performance of regular training or muscular and walking tests impossible; cardiovascular pathologies contra-indicating physical exercise (unstable angina, non stabilized cardiac insufficiency, tight aortic stenosis, severe ventricular rhythm disorders, uncontrolled arterial hypertension, proliferative diabetic retinopathy); infectious or inflammatory evolving affection.
1.2.2
Protocol
1.2.2.1
Physical examinations
The patients benefited from the following evaluations on inclusion visit and on end of study visit at 3 months:
- •
height, weight and body mass index (BMI) measurement;
- •
maximal effort test with measurement of gas exchange on cyclergometer, with initial warm-up at 30 Watts for 3 min, and 10 Watts increase in 1-min stages. The test was realized under continuous electrocardiogram monitoring during the effort and the 6 min of post-effort recovery, and blood pressure was checked every 2 min. The analyzed parameters were: maximal power, defined as the power reached during the last completed stage of 1 min, the maximal cardiac frequency, VO 2 peak, VO 2 at first ventilation stage, as established by the method of Wasserman ;
- •
6-min walk test (6 MWT) and 200-m fast walk test (200m FWT) on indoors marked out ground. The initial 6 MWT was performed following a familiarization test, as recommended in cardiorespiratory pathologies , in order to prevent any learning effect. Under these conditions, this test appeared to be reproducible in obese women ;
- •
measurement of maximal isometric strength of the right knee extensors;
- •
biological tests including: lipid profile, glycosylated hemoglobin (HbA1c), fasting glycemia, Homeostasis Model Assessment index (HOMA) reflecting the insulin-resistance level;
- •
quality of life scale SF-36 .
Furthermore, for the intervention group (IG) patients, the walking and muscular strength tests were repeated during a supervised session at the beginning of the 2nd and 3rd months. During these sessions, the supervisor advised the patient regarding an adapted resistance of the cyclergometer in order to stay within a cardiac frequency (CF) zone of ±5 beats around the CF observed at the ventilation threshold during the initial effort test. Finally, the patients were contacted again by phone between 12 and 18 months after the end of the protocol, in order to complete a questionnaire including three categories of assessment ( Appendix 1 ):
- •
a global assessment of the current physical activity through the PA Questionnaire of Dijon, validated in French ;
- •
an inventory of the reasons limiting the practice of physical activity through a closed questionnaire of 12 items derived from that of Thomas et al. , describing the most frequent causes of physical inactivity. The explored domains concern the fears related to PA, the physical sensations related to PA, the environmental context;
- •
an evaluation of the solutions envisaged by the patient to improve the regularity of a physical activity practice, through a closed questionnaire. The working-out of this questionnaire was approved by four health professionals specialized in PA during chronic incapacitating illnesses ( Appendix 2 ).
1.2.2.2
Intervention
After signing the informed consent, each patient was randomly included either in the control group (CG), or in the intervention group (IG):
- •
in the IG, all patients had a cyclergometer at their disposal at home during 3 months (Ergo-bike, Cardio 2002 PC, Dream electronic, Germany), as well as three supervised training sessions within the Physical Medicine and Rehabilitation department of the University Hospital of Dijon, at the beginning of the program. The recommendations given to the patients were to perform a daily cyclergometer session with: an initial 5 min warm-up at 20 W, then 20 min at the cardiac frequency corresponding to the first ventilation threshold measured during the initial test of effort, then active recovery at 20 W during 5 min . There was no particular phone follow-up, except for the technical management of the material in case of problem;
- •
in the CG, the patients only received counsels regarding regular PA practice, if possible daily (oral information associated to written documents), in accordance with the recommendations .
1.2.3
Statistical analysis
We used a 2-factor ANOVA (group [intervention vs. control] × time [pre vs. post]) with repeated measure for the time factor, in order to study the effects of the group and time factors, as well as their potential interaction, on the evolution of the continuous variables (lipid test, glycemia parameters, biometry, strength of the quadriceps, results of the effort tests, quality of life questionnaires). For the non-parametric variables, we used a Wilcoxon test. Regarding the questionnaires data, we compared the results between the two groups with the exact Fisher’s test. The statistical analyses were performed with the SPSS software for Windows. The level of significance chosen for all tests has been set to P < 0.05 taking a bilateral hypothesis.
1.3
Results
1.3.1
Population
Twenty-three patients were included, with five drop-outs (three for non-completed protocol, two for intercurrent illnesses non protocol-related). Eleven subjects were therefore randomized to the training group and 12 to the control group. The patients’ characteristics at baseline are shown in Table 1 . The patients were of a mean age of 52.8 years (± 8.5 years), mainly women, with stage 2–3 obesity, all undergoing a drug treatment in accordance with the recommendations ( Table 1 ) . There was no difference in the anthropometric and physical characteristics between the two groups at inclusion ( Table 1 ).
| Control group ( n = 12) | Intervention group ( n = 11) | Difference between groups (P) | |
|---|---|---|---|
| Age | 52.8 ± 8.5 | 52.4 ± 8.2 | > 0.05 |
| Sex (M/F) | 4 / 8 | 6 / 11 | > 0.05 |
| Weight (kg) | 110.4 ± 25.2 | 106.9 ± 26.4 | > 0.05 |
| BMI (kg/m 2 ) | 40.1 ± 7.3 | 39.3 ± 9.9 | > 0.05 |
| Obesity class (%) | I (17%), II (33%), III (50%) | I (26%), II (27%), III (47%) | > 0.05 |
| Insulinotherapy | 12 | 11 | > 0.05 |
| Oral anti-diabetics | > 0.05 | ||
| Metformin | 8 | 7 | > 0.05 |
| Hypoglycemic sulfonamides | 2 | 3 | > 0.05 |
1.3.2
Evolution of the anthropometric and biological parameters
The anthropometric and biological parameters did not show significant modifications ( Table 2 ).
| Control group ( n = 12) | Intervention group ( n = 11) | P | |||||
|---|---|---|---|---|---|---|---|
| M0 | M3 | CV % | M0 | M3 | CV % | ||
| BMI | 40.1 ± 7.3 | 40.4 ± 6.6 | 1.1 ± 8.2 | 39.3 ± 9.9 | 37.1 ± 8.2 | −5.6 ± 6.0 | NS |
| Weight (kg) | 110.4 ± 25.2 | 110.6 ± 18.7 | 1.1 ± 8.2 | 106.9 ± 26.4 | 100.9 ± 23.0 | −5.6 ± 6.0 | NS |
| FG (mmol/l) | 10.4 ± 3.2 | 9.6 ± 3.3 | −7.6 ± 27.8 | 9.6 ± 3.8 | 9.3 ± 3.5 | 3.1 ± 34.0 | NS |
| HbA1C (%) | 9.0 ± 2.0 | 8.6 ± 1.7 | −4.4 ± 11.9 | 8.3 ± 1.6 | 7.9 ± 1.9 | −4.8 ± 13.6 | NS |
| HOMA-IR | 23.1 ± 53.4 | 1.8,1 ± 30.4 | 21.6 ± 129.1 | 26.8 ± 75.4 | 14.9 ± 20.6 | 44.4 ± 364.4 | NS |
| CHOL (mmol/l) | 4.5 ± 1.2 | 4.6 ± 0.6 | 2.2 ± 4.2 | 4.3 ± 1.2 | 4.3 ± 1.1 | 13.0 ± 6.9 | NS |
| LDL-C (mmol/l) | 2.8 ± 1.0 | 2.8 ± 0.6 | 0.6 ± 6.2 | 2.3 ± 0.8 | 2.4 ± 0.7 | 1.7 ± 5.6 | NS |
| HDL-C (mmol/l) | 0.9 ± 0.2 | 0.1 ± 0.2 | 88.8 ± 43.5 | 1.0 ± 0.4 | 0.9 ± 0.2 | 11.0 ± 53.0 | NS |
| TG (mmol/l) | 1.8 ± 0.8 | 1.8 ± 0.9 | 0.2 ± 2.2 | 1.9 ± 1.2 | 1.7 ± 0.8 | −1.8 ± 39.5 | NS |
1.3.3
Evolution of the physical capacities
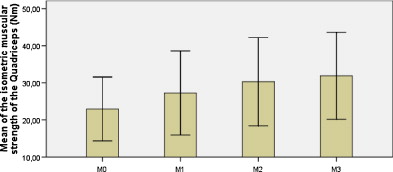
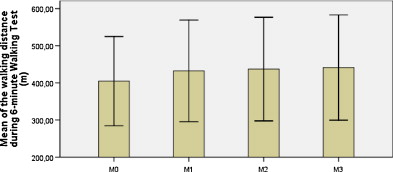
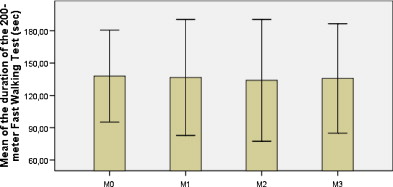
The improvement of the maximal power developed at the end of the effort test on cyclergometer, as well as the muscular strength of the quadriceps were significantly more important in the Training Group ( Table 3 ). There was no difference of improvement between the two groups for the VO 2 peak or for the VO 2 at the ventilation threshold, neither for the performance during the walking tests ( Table 3 ). The evolution of the physical parameters (maximal isometric muscular strength of the quadriceps, walking tests) during the follow-up visits is shown in Figs. 1–3 .
| Control group ( n = 12) | Intervention group ( n = 11) | P | |||||
|---|---|---|---|---|---|---|---|
| M0 | M3 | CV % | M0 | M3 | CV % | ||
| VO 2 peak (ml/kg/min) | 16.4 ± 3.7 | 16.1 ± 3.6 | −1.9 ± 7.3 | 16.4 ± 2.5 | 17.1 ± 2.9 | 4.2 ± 13.9 | NS |
| VO 2 threshold (ml/kg/min) | 10.2 ± 2.2 | 9.6 ± 1.8 | −5.8 ± 9.7 | 9.7 ± 2.0 | 9.6 ± 1.8 | 1.0 ± 13.9 | NS |
| Power (Watt) | 95.0 ± 31.2 | 91.8 ± 27.6 | −3.3 ± 16.4 | 93.5 ± 24.7 | 101.2 ± 28.0 | 8.2 ± 17.4 | 0.04 (F = 3.9) |
| 6mWT (m) | 389.5 ± 80.9 | 393.3 ± 82.0 | 0.1 ± 14.1 | 404.7 ± 61.8 | 441.0 ± 65.3 | 9.1 ± 12.2 | NS |
| 200mFWT (sec) | 144.0 ± 43.2 | 158.1 ± 66.1 | 9.8 ± 27.0 | 137.0 ± 20.6 | 135.78 ± 46.4 | 5.8 ± 9.9 | NS |
| Quad (Nm) | 23.4 ± 8.2 | 23.4 ± 15.0 | −0.1 ± 45.7 | 23.4 ± 6.4 | 32.3 ± 7.0 | 38.0 ± 36.1 | 0,008 (F = 8.7) |
1.3.4
Quality of life score
There was no significant difference between the 2 groups regarding the SF-36 total score or sub-scores.
1.3.5
Evaluation at a distance from the protocol through the questionnaires on physical activity
This evaluation was performed on average 17 ± 6.4 months after the end of the protocol without any significant difference concerning this delay between the two groups (15.8 ± 6.2 months in the Control Group vs. 17.5 ± 6.7 months in the Training Group).
1.3.5.1
Evaluation of the physical activity score
The results of the Dijon questionnaire on physical activity were not different between the two groups (CG: 14.8 ± .5.8 /30 points, and IG: 14.7 ± 6.3 /30, P > 0.05).
1.3.5.2
Evaluation of the barriers to the practice of physical activity
From the results presented in Fig. 1 , we have schematically distinguished causes of physical inactivity evaluated as rare (< 20%), little frequent (between 20 and 39%), frequent (between 40 and 59%), and very frequent (≥ 60%). So, the very frequent causes of physical inactivity reported by the patients are: “Low motivation”, “Poor PA capacity”, “Pain following PA”, “Bad tolerance during PA”. On the opposite, each of the items concerning the “fears” is reported by less than 40% of the patients.
1.3.5.3
Solutions envisaged by the patients to improve regular physical activity observance
The answers with a frequency higher than 40% are the following ( Fig. 2 ):
- •
location of PA practice: indoors and outdoors (mixed);
- •
social context of PA: concerning collective PA, mixed groups are preferred;
- •
PA follow-up: preferably weekly, in consultation with a physical assistant;
- •
segmental work: muscular reinforcement practice is privileged;
- •
financial support to favor PA.
Finally, to the question: “Classify by increasing order of preference the type of aerobic physical activity”, the patients answered on average in the following order: rowing machine < swimming pool < bicycle < walking.
1.4
Discussion
This study has highlighted the favorable impact at short term of an effort training program of 3 months in type 2 diabetes obese patients, on the muscular and functional walking capacities, as well as on the body mass. This program has however had no significant effects on the metabolic parameters, and has not allowed leading to modifications in the habits of PA practices at long term. The answers of the patients to the questionnaires concerning the barriers to a regular practice of PA and the solutions to improve observance allow a comprehensive approach of the psychobehavioral, physical and environment mechanisms leading to physical inactivity in this population. The programs of physical exercise recommended in the global management of type 2 diabetes combine global endurance exercises (cyclergometers or walk) with segmental muscular reinforcement exercises , this association providing the maximum of efficacy compared to each technique taken separately . These global programs may be supervised or not, provided to out-patients or complete hospitalized patients There is no specific study comparing these various solutions for type 2 diabetics, probably because it is recommended that the practice of muscular reinforcement exercises be supervised . So, in order to be in realistic conditions closer to real life, we have privileged here the practice of a home-based aerobic activity, in the image of the cost-efficacy study of Brun et al. .
Our protocol has shown the efficiency of pedaling in these obese patients with type 2 diabetes highly deconditioned (VO 2 initial peak of 4.7 METs, that is to say less than 40% of the performance of healthy matched subjects ), as can be seen from the significant improvement of the maximal power at the end of the final test of effort and of the maximal muscular strength of the knee extensors in the Intervention Group. The VO 2 peak tends to be increased in the Intervention Group, but at the limit of significance. This resistance to improvement of aerobic performances has already been reported by Vergès et al. in coronary patients with diabetes . It is still not well explained, possibly multifactorial, with however a probable role of hyperglycemia . It is nevertheless important to aim at this improvement, as it has been clearly shown that a high effort capacity is a factor reducing the risk of cardiovascular events and of mortality of any cause in type 2 diabetics , obese patients , and patients presenting with a metabolic syndrome .
We haven’t found any difference between the groups as regards the improvement of the walking performances at 6 mWT and 200m FWT, despite the more marked improvement in the intervention group of the muscular strength of the knee extensors, playing an important role during the propulsive phase of the walk. A non-linear relation between these two variables has already been reported in healthy elderly subjects , and could have been more marked in this study because of the muscular deconditioning of the patients. Furthermore, we have chosen to measure the muscular strength at the end of the protocol, but the potential delay between the strength earnings and their transfer to a functional improvement remains not well known.
We found a weight loss in the intervention group, but non-significant, with results (−6 kg) comparable with those usually reported during the intervention including aerobic training, associated or not to muscular reinforcement . It was not however the main objective of this study. Moreover, the different studies measuring the effect of PA on weight loss are often associated with diet measures. Therefore the specific effect of PA is difficult to assess.
Concerning the biological parameters, the results show no modification in both groups. These results in contradiction with those reported in the meta-analysis of Thomas et al. are probably related to the lack of power of the study, and to the fact that this meta-analysis included indiscriminately any type of exercise, aerobic associated or not with muscular reinforcement. It could also be related to an average observance with patients who haven’t otherwise increased their daily PA outside the protocol, as shown by the poor Dijon scores of PA, collected at a distance in both groups. Nevertheless, a weight loss such as that noted in the Intervention Group should induce an improvement of the metabolic profile . Another hypothesis is therefore that of poor drug observance, as already reported in this population taking stringent treatments . As we have not collected this element, we cannot conclude on it. There was no significant difference in evolution of quality of life between both groups. Our study focused on overweight subjects; many of them were in difficult social situations (financial precariousness, social isolation…). The home-based PA program presented here was not much monitored, and there was no global management, particularly social, that could be appropriate for improving the quality of life of these patients.
The analysis of the questionnaires on the evaluation of the amount of PA at a distance from the protocol shows that the effects of this program are not persisting, with an average low PA score (about 14/30 in both groups), corresponding to an important level of sedentary way of life . This low impact on regular long-lasting PA observance represents the main limit of home-based programs, and our results are in accordance with those of Shinji et al. who have recently shown that after a 17.2-months follow-up, 37% of the patients included in a home-based program of effort training of aerobic, non-monitored type, declare having given up any regular physical activity. This was confirmed by another study in sedentary patients at risk of diabetes followed-up for one year, where no difference was found regarding daily energy expenditure between the control group simply receiving lifestyle counsel by mail, and the group monitored by a physical coach at home or by phone . Regarding the muscular reinforcement programs, Dunstan et al. report a 67.1% declared observance at a 12-months distance from a home-based segmented PA program (initiated at the centre). This was insufficient however to maintain the improvement on the HbA1C initially obtained.
The questionnaires concerning the barriers to the performance of regular PA and the solutions envisaged by the patients to improve the regularity of their practice allow bringing out some trends characterizing the causes of physical inactivity in this sample of patients. Contrary to the barriers reported by type 1 diabetics , the most often mentioned reasons concern the feel related to PA practice, whereas fears related to PA practice are less often mentioned. The most frequently cited item is the non-motivation for performing PA. This suggests that the patients are in a precontemplative stage, with reference to the classification of the transtheoretical model of Prochaska and DiClemente . Therefore it could probably be interesting to try out an initial motivational approach in this population, in order to prevent any early demotivation linked for example to dyspnea or to musculo-arterial pain. It is indeed probable that in this obese diabetic population, the coexistence of psychical causes (“fears” in general) and organic causes (pain, poor tolerance, low capacity) interact in the lack of motivation for regular PA. If this program could allow removing some barriers, particularly psychological, to the performance of PA, some organic causes may probably still remain, such as low physical capacity, pain during and after the effort, which are sufficient to maintain the vicious circle of physical inactivity.
The home-based PA programs with initial supervision are therefore only a step in the life habit changes of these patients. A long-term follow-up should probably be provided in order to perpetuate the practice of PA . This approach could be characterized in France by the performance of rehabilitation programs combined with an educational approach in type 2 diabetic patients presenting a high risk of non-observance of regular PA.
We have attempted to consider a few solutions to perpetuate the results of a training program by questioning the patients directly about their opinion on how to improve their practice of regular PA. A solution often cited is a varied practice in a varied environment too, probably in a wish to fight against monotony during practice. There is also a high request for monitoring by PA professionals, 80% of the patients putting forward the interest of a follow-up by a physical assistant. This seems therefore to be an important element to propose these patients at the end of effort training programs. This follow-up could be performed by physical instructors trained to adapted physical activities in coordination with the medical and paramedical teams. Such an intervention has demonstrated an improvement at 12 months of the declared amount of PA (+115 min per week) in the intervention group compared to the control group (−15 min per week) . Financial support is also frequently requested by the patients to increase the amount of PA. Financing accelerometers or podometers could be a clever choice, since it has been shown in some studies that such measures allow improving the observance to PA in type 2 diabetics . Finally, at the era of telemedicine, other innovating strategies could be built up in order to promote long-term regular PA such as the use of a mobile or of the Internet to manage a PA program .
1.5
Limits
The limit of this work is the limited number of inclusions. The results of this pilot study need therefore to be confirmed. The recruitment of this study determined the selection of diabetic patients presenting with a very important overweight (BMI > 35 kg/m 2 ) and with a very much altered initial glycemic status (HbA1C > 8%, fasting glycemia > 1.7 g/l). This constitutes a selection bias linked to the mode of recruitment in the diabetology department. This protocol has indeed been proposed to subjects for whom the maximal drug treatment and the educative approach did not allow restoring their glycemia. Hence it is possible that the results of the proposed intervention are limited, particularly regarding the metabolic parameters, by an escape effect from the other implemented therapies (medications and dietetics mainly). The results obtained can probably not be generalized to the whole population presenting with type 2 diabetes. Furthermore, the absence of measurement of body composition and of the waist limits us in the interpretation of the cardiovascular risk evolution in particular, as the waist measurement, highly correlated with the quantity of abdominal fat , represents a strong independent predictive factor of mortality . Similarly, it does not allow either knowing whether weight loss was associated to a decrease of the light mass, which is probable with regard to the absence of muscular reinforcement in the intervention, and could possibly explain the lack of results concerning the evolution of glycemia control and of HOMA-IR. The absence of PA questionnaire and of a study on the barriers to PA at inclusion represents also a factor limiting the study of the intervention impact on these elements. The initial protocol did not include these measures, which have been added afterwards, in an attempt, among other things, to understand the difficulties of motivation of the subjects who often needed numerous phone recallings. Lastly, we have neither data concerning the amount of physical activity performed in the control group during the period of intervention, nor any objective data on observance for the patients in the intervention group, except for the questioning of the intermediary evaluations. Moreover, the questionnaire concerning the solutions envisaged for increasing the practice had only four types of aerobic activities and two types of segmented activities, and we cannot exclude that some patients did other activities, more original and not reported in this questionnaire.
1.6
Conclusions
This work has shown the short-term benefits of a home-based program of effort training on exercise and functional walking capacities in poorly managed type 2 obese diabetics, without any effect on metabolism. The significance of these results remains however limited by the lack of power of the study. The interest of this work lies more in the evaluation of this program at a distance on the preservation of a PA, as recommended. The result appears disappointing, suggesting a modification of the management approach of these patients with poor observance, probably by combining an educative, physical approach and the relay of associations. Follow-up care and specialized rehabilitation and the networks hold here an important place in the implementation of such programs once the patients leave the acute care departments. It will probably be necessary to better characterize screening criteria of patients at risk of sedentary life in order to propose adapted solutions of follow-up and management. Our population of overweight diabetes patients seems to correspond to this situation, as can do the whole population of the most deficient patients in terms of physical exercise capacity such as those with cardiac insufficiency, or hemiplegic patients. A better understanding of the psychobehavioral, physical, and environmental mechanisms leading to physical inactivity will allow better fighting against this vicious circle.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgements
This study received a grant from the “Programme Hospitalier de Recherche Clinique” 2002.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







