Achieving optimal soft tissue balance intraoperatively is a critical element for a successful outcome after total knee arthroplasty. Although advances in navigation have improved the incidence of angular outliers, spatial distance measurements do not quantify soft tissue stability or degrees of ligament tension. Revisions caused by instability, malrotation, and malalignment still constitute up to one-third of early knee revisions. The development of integrated microelectronics and sensors into the knee trials during surgery allows surgeons to evaluate and act on real-time data regarding implant position, rotation, alignment, and soft tissue balance through a full range of motion.
Key points
- •
Historically, ligamentous tension and laxity have not been measured and thus have not been quantified to correlate with patient outcomes.
- •
Intraoperative sensors can guide and confirm correction of soft tissue imbalance.
- •
Intraoperative sensors can communicate the effects of implant alignment and rotation on soft tissue balance.
- •
Intraoperative sensors allow the evaluation of the effects of implant kinematic design on the kinetic profile of the knee joint.
Ligamentous imbalance and incidence of revision
A successful total knee arthroplasty can alleviate pain and reestablish proper kinetics to an arthritic joint. This highly effective procedure is performed in more than 500,000 new patients in the United States every year, and this number is expected to reach 3.48 million by 2030.
Although the survivorship of total knee arthroplasty components is greater than 90% at 15 years, the revision burden (defined as the ratio of revision to the total number of arthroplasties) has not improved for the past decade.
The clinical and economic implications for revision surgery are underappreciated. More than 55,000 revision surgeries were performed in 2010 in the United States, with 48% of these revisions performed in patients younger than 65 years. Total costs associated with each revision total knee arthroplasty have been estimated to exceed $49,000. The current annual economic burden of revision knee surgery is $2.7 billion in hospital charges alone. By 2030, assuming a 5-fold increase in the number of revision procedures, this economic burden will exceed $13 billion annually.
The number of revision total knee arthroplasties is expected to continue to increase, in concert with the rapidly increasing number of primary procedures, over the next 20 years. Thus, new technologies that limit the factors associated with an increased risk of revision are now paramount to both the continued success of primary total knee replacement and reducing the economic burden associated with revision procedures themselves.
Joint infection is still the foremost cause of early revision. However, instability, malrotation, malalignment, component loosening, and patellofemoral complications all result from surgical technique that inadequately addresses soft tissue balance.
Instability is cited in up to 22% of reported reasons for revision. In patients exhibiting instability, excessive laxity in the soft tissues can cause pain, effusions, and an inability to navigate curbs and inclined planes.
Component loosening (up to 17% of early-stage revision; 34% of late-stage revision) is often a secondary effect of accelerated polyethylene wear. Polyethylene microdebris disseminates into the joint space and causes an inflammatory immune response. This inflammation results in osteolysis and disintegration of the bone–component interface. Accelerated wear is seen in patients with excessive soft tissue tension medially, laterally, and in the flexion gap from an excessively tight posterior cruciate ligament (PCL).
Malalignment and patellofemoral complications caused by maltracking can lead to anterior pain, patellar instability, patellar fracture, and tibiofemoral flexion instability. These complications can occur from tibiofemoral rotational incongruency, commonly caused by internal rotation of the tibial tray, femoral component, or both.
Reduction in the occurrence of these soft tissue related complications is essential for minimizing the percentage of revision procedures after total knee arthroplasty. Real-time data, presented intraoperatively, can assist the surgeon in reducing surgical outliers and achieving a well-aligned and well-balanced knee.
Defining balance
Traditional Methods for Defining Balance
To achieve gap balance, most surgeons typically use spacer blocks to confirm that the extension and flexion gaps of the joint are equal with respect to a fixed distance measurement. This gap measurement dictates composite thickness of the final implant.
Surgeons then rely on tactile navigation with their own hands, assessing coronal plane balance through applying a varus-valgus moment to the joint and evaluating the relative opening in each compartment.
Spacer blocks provide information on joint gaps and the alignment of cuts, but are not sensitive to soft tissue balance in the sagittal plane. When using spacer blocks, defining coronal intercompartmental balance in mid flexion and full flexion is often inconsistent, secondary to the open capsule, a subluxed patella, and hip rotation.
Surgical approaches to prepare the knee joint for the final prosthesis vary based on surgeon training and instrumentation. The 2 standard methods that are well documented are
- 1.
Measured resection: a technique in which the surgeon makes all bony cuts based on anatomic references, then uses the trial implants to balance soft tissue tension.
- 2.
Gap balancing: a technique in which the extension gap is balanced after the distal femur and proximal tibia are resected. The flexion gap is then distracted at 90°, allowing ligament tension to guide the femoral rotation.
Several factors contribute to inaccuracy in restoring normal balance and alignment in total knee arthroplasty when using either of the previously mentioned techniques. First, bony landmarks currently used to determine femoral rotation have been shown to be inaccurate, particularly in a deformed arthritic knee. Second, soft tissue releases do not always affect flexion and extension gap balance symmetrically. Finally, optimizing tibiofemoral balance can sometimes negatively affect patellofemoral tracking.
The difficulties in achieving balance persist despite the availability of the techniques described earlier, because determining the degree of ligament balance in total knee arthroplasty has traditionally been established by the subjective assessment of each surgeon. Surgical results achieved by these subjective methods have been variable without the availability of intraoperative data to correlate techniques to outcomes. Until recently, no method was available with which to quantify the relative “feel” of a joint when guiding soft tissue release.
Novel Methods and a More Precise Definition of Balance
Technological advances in microelectronics have only recently made it possible for the surgeon to quantify how ligamenture surrounding the joint directly affects articular kinetics through a full range of motion. This new sensor-embedded technology allows the surgeon to adjust for soft tissue imbalance, while receiving dynamic visual feedback regarding the specific knee design, within each patient-specific soft tissue envelope. For the first time, subjective surgeon assessment can be quantified, and balance in the coronal and sagittal planes is verifiable.
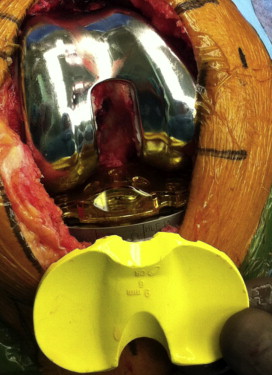
The sensor-embedded microelectronic array is housed in the standard tibial insert ( Fig. 1 ) trial to identify the effects of alignment, rotation, and ligamentous tension or laxity on the geometric design of the knee.
Clinical and biomechanical analyses have shown that optimal joint kinematics are best evaluated with the patella reduced and the medial capsule closed. The knee is taken through a full range of motion, and the intercompartmental load differential is examined in early flexion, mid flexion, and full flexion to detect coronal plane asymmetry. The femoral rollback and posterior drawer is tested while the femoral contact points are evaluated to assess sagittal plane stability.
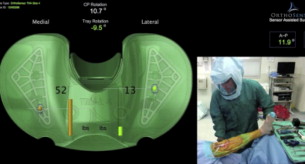
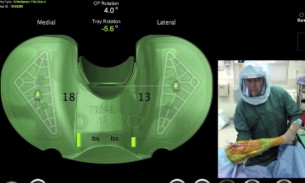
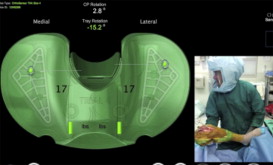
The development of sensor-embedded technology has allowed the construction and verification of a more scientifically based definition of balance . A new definition of soft tissue gap is exhibited from 10° to 110° of flexion. In terminal extension, the effects of compression, the screw-home mechanism, and the posterior capsule mask the effects of soft tissue tension or laxity ( Figs. 2–4 ).
Therefore, the most useful application for this intraoperative data is to apply it to the evaluation of subtle joint imbalance, tibiofemoral rotational incongruency, and component malalignment.
Clinical applications for dynamic soft tissue balancing
Rotational Incongruency
Tibiofemoral rotational incongruency in total knee arthroplasty is associated with anterior knee pain, poor kinematic function, unfavorable patellar tracking, and decreased implant survivorship. In one particular study, arrack and colleagues showed that as little as 4.6° of internal rotation can cause anterior knee pain. Additionally, Berger and colleagues reported that 5° to 8° of tibiofemoral rotational incongruency leads to patellar maltracking.
To establish an appropriate rotational orientation of the femoral component, anatomic reference points are commonly used. Flexion distraction technique is also used to obtain a parallel flexion gap using the ligament tension in flexion to determine the femoral rotation.
When aligning the tibial tray, the mid to medial third of the tibial tubercle is commonly used. However, errors have been reported when using this landmark, because of a wide variance of up to 25° of rotation inherent in the line between tibial tubercle and posterior tibial plane.
A retrospective analysis of intraoperative data from 100 consecutive total knee replacements found that 63.1% of patients exhibited an average of 6.3° ± 4.3° of asymmetrical tibiofemoral contact-point positioning in extension. Tibial tray rotation for all patients was initially dictated by the location of the mid-third of the tibial tubercle. Guided by intraoperative sensor feedback, the surgeon was able to correct all rotational incongruency in every case.
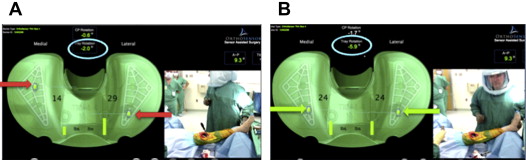
Through incorporating intraoperative sensors, surgeons can set the rotation of the components using any method of their choosing. When the components are in place, any remaining tibiofemoral rotational incongruency can be corrected for using the location of femoral contact points, as shown dynamically on-screen by the sensor system.
With the placement of an anterior-medial or lateral pin to control for potential translation of the tray across the tibial plateau with trialing, the surgeon adjusts the tibial tray rotation until alignment of the femoral contact points is achieved ( Fig. 5 ). These adjustments are evaluated and confirmed in real time. Central patellar tracking is then confirmed and the tray is pinned and stabilized. Optimal congruency is important to define before kinetic rollback and soft tissue balance are assessed. It is also seen that when the femoral condyles are relocated to the central tibial plateau and the femoral contact points are below 5° of rotation, soft tissue tension commonly equalizes. The belief is that this mechanism will improve anterior knee pain and stability through a full range of motion.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




