Double-Bundle Anterior Cruciate Ligament
Kevin N. Jiang
Christopher D. Murawski
Freddie H. Fu
DEFINITION
Anterior cruciate ligament (ACL) tears have been described in detail in Chapter 49.
Any patient with functional instability or pivoting of the knee is considered to have an ACL insufficiency.
Anatomic ACL reconstruction is defined as the functional restoration of the ACL to its native dimensions, collagen orientation, and insertion sites.18
ANATOMY
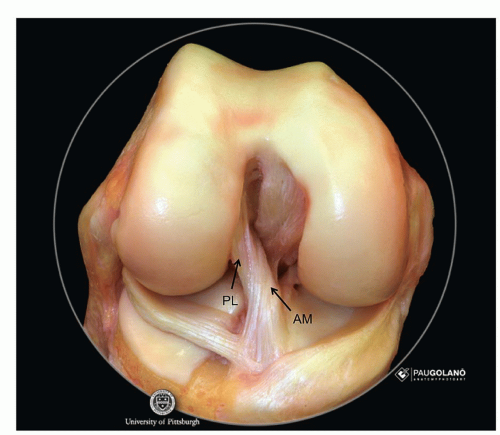
The ACL is an intra-articular, extra-synovial ligament of nonparallel collagen fibers that arise from the posterior aspect of the lateral femoral condyle and insert on the tibial plateau between the medial and lateral tibial spines2,7,8 (FIG 1).
To fully understand the principles of ACL reconstruction, it is important to understand the complex anatomy of the ACL, which is composed of two major bundles, the anteromedial (AM) and posterolateral (PL) bundles, named according to their relative insertion sites on the tibia.12,15
At the femoral insertion site, the lateral intercondylar ridge (“residents ridge”) represents the upper (anterior) limit of the ACL, whereas the lateral bifurcate ridge divides the AM and PL bundle insertion sites and is perpendicular to the intercondylar ridge.9,10
The AM and PL bundle are synergistic according to knee flexion angle and control anterior and rotational stability of the knee. The AM bundle remains constant through knee flexion but attains peak tension between 45 and 60 degrees of knee flexion. The PL bundle is tightest in extension and loosens with knee flexion, thereby allowing rotation.6,11
PATHOGENESIS
The majority of ACL ruptures, approximately 70%, occur via a noncontact injury mechanism.
Females are approximately seven times more likely to suffer an ACL injury than males.17
NATURAL HISTORY
The natural history of an ACL rupture is multifactorial and depends on patient age, activity level, concomitant injury, and degree of functional instability.
The majority of athletic patients suffering an ACL rupture will be unable to perform cutting and/or pivoting activities without surgical reconstruction of the ACL.
A small percentage of carefully identified patients may be able to undergo successful nonoperative rehabilitation. However, the patient should be aware that repeated episodes of instability is likely to induce secondary damage to the knee in the form of meniscal and/or cartilage pathology.
In the long-term, patients are likely to develop some form of osteoarthritis after an ACL rupture regardless of conservative or surgical treatment.
PATIENT HISTORY AND PHYSICAL FINDINGS
A noncontact valgus pivoting injury followed by an effusion of the knee is highly suspicious of an ACL rupture. If an ACL rupture has occurred, patients are typically unable to return to the same athletic competition.
The physical examination and methods for examination of the ACL are covered in Chapter 49.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs should include the following views:
Thirty-degree flexion weight-bearing posteroanterior (PA) view
Lateral
Sunrise (Merchant) view of the patella
Long-leg alignment view in the case of suspected coronal angular deformity
Magnetic resonance imaging (MRI) should be ordered to confirm a suspected ACL tear and evaluate potential rupture pattern, including partial ACL tears. MRI is also used to evaluate potential associated injuries of the chondral surfaces, menisci, and other ligamentous structures.
The sagittal MRI can be used to measure the length of the tibial insertion site of the ACL in the AP dimension as well
as the inclination angle and length of the ACL. These measurements can be used in individualized ACL reconstruction and are discussed in the following text. Moreover, the thickness of both the quadriceps and patellar tendons can be used to provide the surgeon with an approximation for graft size prior to harvest.
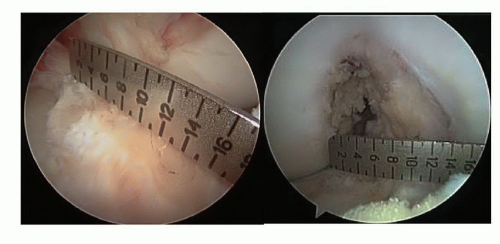
FIG 2 • The tibial insertion site of the ACL (left) and intercondylar notch width are measured intraoperatively using an arthroscopic ruler.
Computed tomography scan should be ordered in revision cases to assess for factors such as tunnel widening. The images can also be reconstructed three-dimensionally for an accurate assessment of primary tunnel placement for preoperative planning of revision surgery.
An instrumented laxity test (eg, KT-1000 arthrometer) to assess anteroposterior knee laxity can be performed to determine absolute translation and side-to-side translation difference.
DIFFERENTIAL DIAGNOSIS
Contusion
Meniscal tear
Osteochondral injury
Patellar dislocation, which may mimic the initial presentation of an ACL injury
Collateral ligament injury (eg, medial collateral ligament, lateral collateral ligament)
Multiple ligament injury
NONOPERATIVE MANAGEMENT
Potential nonoperative treatment candidates and rehabilitation protocol are detailed in Chapter 49.
SURGICAL MANAGEMENT
Indications
The indications for anatomic double-bundle ACL reconstruction are similar to those for traditional single-bundle reconstruction.
Patients with recurrent instability or episodes of giving way or those who are unable to return to activities of daily living or sports are appropriate for surgical reconstruction.
Patients with complaints of instability and a single-bundle or “partial” tear may benefit from single-bundle augmentation or double-bundle reconstruction in the event that the remaining bundle is incompetent.
Measurements of the tibial footprint (FIG 2) and notch preand intraoperatively help guide individualized ACL reconstruction to better reproduce native anatomy.
Tibial footprint length
14 mm or less—single-bundle reconstruction
14 to 18 mm—single- or double-bundle reconstruction
More than 18 mm—double-bundle reconstruction
Notch width
12 mm or less—single-bundle reconstruction
More than 12 mm—double-bundle reconstruction
Contraindications
Tibial footprint length 14 mm or less
Notch width 12 mm or less
PREOPERATIVE PLANNING
Graft Options
Anatomic double-bundle reconstruction can be performed using quadriceps tendon autograft with patella bone block, or soft tissue graft, including hamstrings autograft and allograft. Bone-patellar tendon-bone (BPTB) grafts cannot be used for double-bundle reconstruction.
The quadriceps tendon can be used for a single-bundle graft or split longitudinally through a natural plane into its rectus femoris and vastus interomedialis portions to create a double-bundle graft.
The smaller rectus portion is used to reconstruct the PL bundle and the larger vastus portion for the AM bundle.
Soft tissue grafts
Two separate tibialis anterior or tibialis posterior tendon allografts can be used.
These grafts are usually 24 to 30 cm in length, and we fold each tendon graft to obtain 12 to 15 cm doublestranded grafts.
The AM tendon double-stranded graft is typically 8 mm and the PL graft is 7 mm. These sizes can be individualized to the patient based on the native anatomy.
Semitendinosus and gracilis autografts can be harvested (see Chap. 49) and used for reconstruction.
ACL graft preparation is done during the arthroscopic procedure on the back table.
Exam under Anesthesia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree