Chapter 7 Dizziness, visual and sensorimotor control disturbances following whiplash injury
After pain, symptoms of dizziness, unsteadiness and visual disturbances are some of the next most frequent complaints, with between 40% and 75% of those with persistent whiplash reporting these symptoms.1 In addition, altered head position and movement sense, problems in maintaining and performing postural stability tasks,1–4 and deficits in eye movement control5–7 have also been demonstrated in individuals with chronic whiplash. A better understanding of the causes and relationships of such persistent problems following a whiplash injury is vital to establish appropriate diagnostic measures and relevant rehabilitation.
Aetiology of dizziness, visual disturbances and sensorimotor control disturbances in whiplash associated disorders
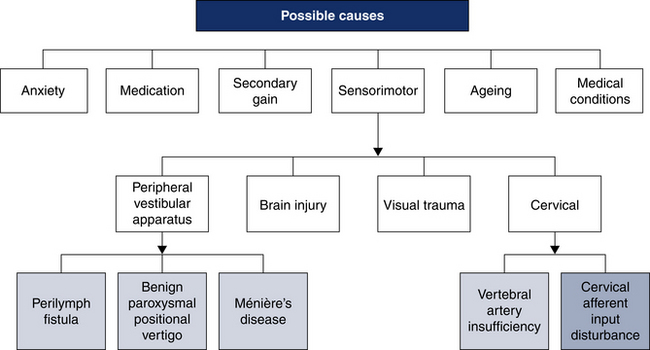
A myriad of causes have been suggested to underlie the symptoms of dizziness and visual disturbances in whiplash associated disorders (WAD). Anxiety, malingering and medication use have been raised as factors contributing to the persistence of these symptoms.8 However, disturbances to the sensorimotor control system appear to be the most likely causative factors of these symptoms, due to traumatic damage to one or more of the three main systems providing input to the sensorimotor control system: vestibular, visual or neck receptors, or damage directly to the central nervous system (CNS).9, 10 Structural damage to the vertebral artery is also possible following a whiplash injury.11 Nevertheless, in those with a pure whiplash injury (i.e. no head injury), there is reasonable evidence to suggest that the disturbances are primarily of a cervical origin from both damaged or functionally impaired neck joint and muscle receptors. Secondary vestibular hypo- or hyperfunction may also occur due to disturbed cervical afferents.9, 10, 12 Thus, the focus of this chapter is on cervical-related causes of such disturbances. Nevertheless, as people with persistent whiplash may be taking medications, anxious or seeking compensation, may or may not have had a mild head injury, may have had some peripheral vestibular or vertebral artery damage, and have neck pain and associated musculoskeletal damage, each of these factors should be considered in the differential diagnosis (Fig 7.1).
Anxiety
Elevated levels of anxiety have been recorded in subjects with persistent whiplash.13 Anxiety is well recognised as a cause of dizziness14 and has been implicated in balance disturbance, with some evidence for a neurological relationship between anxiety and the vestibular apparatus.15 Interestingly, it has also been suggested that a causal or perpetuating link may exist between anxiety and associated increased muscle tension and neck-related causes of dizziness.16 Stress may also influence cervical muscle spindle sensitivity via activation of the sympathetic nervous system.17
However, a series of studies have found no differences in anxiety levels between participants with whiplash who did and did not complain of dizziness. In addition, both general anxiety levels and anxiety at the time of testing did not appear to influence between group differences of the sensorimotor deficits.1, 5, 18 However, it is possible that anxiety may play a secondary or exacerbating role in the production of these symptoms and signs in some with persistent WAD.
Secondary gain
Assertions that people are exaggerating symptoms for secondary gain have, for many years, been a common thread in the literature related to persistent complaints of symptoms, such as pain and dizziness, following a whiplash injury.19 Despite this, there is no evidence to demonstrate significant differences in symptomatic complaints, or response to treatment between patients who are or are not involved in compensation claims.20 In recent studies, there was also no evidence that compensation status was associated with complaints of dizziness and/or any of the deficits seen in sensorimotor control in individuals with persistent whiplash.1, 5, 18 In addition, in a recent study, the pattern of balance disturbances in asymptomatic people instructed to feign balance deficits was found to be significantly more exaggerated when compared to disturbances seen in those with whiplash.21
Medications
Medications, such as anti-inflammatory, antipsychotic and narcotic drugs, are commonly prescribed to patients with persistent whiplash, and may adversely affect postural sway.22 Similarly, antidepressants, muscle relaxants or vestibular depressants may create gaze-evoked nystagmus and influence oculomotor function.22 Thus, some of the signs and symptoms seen in whiplash could also be a side-effect of these medications. Despite this occurrence, recent studies have found no evidence that medications were associated with whiplash symptoms. The results indicated no differences in either the frequency of dizziness and/or deficits in balance, head or eye movement control in participants who were routinely taking medication up to 24 hours prior to testing, compared to those not taking these medications.1, 5, 18
Vertebral artery insufficiency
Vertebral artery insufficiency is another possible cause of dizziness and visual disturbances following a whiplash injury. It is possible that cervical trauma may result in damage to the vertebral vessels,23 but the evidence suggests that this rarely occurs (0.5–4%) in survivors of blunt cervical or head trauma.24 This would suggest that the incidence of vertebral artery injury following a whiplash injury is low, albeit possible.25 Isolated case reports have been identified, with symptoms usually occurring within a few minutes of the injury,26, 27 although longer delays have been reported.28
Only one study has looked specifically at vertebral blood flow in patients following a whiplash injury.29 Few patients in this study reported vascular symptoms, despite a relatively high incidence of abnormal vertebral artery blood flow.29 Evidence from studies of those with traumatic vertebral artery dissection post cervical fracture would also suggest that, in the majority of cases, there are minimal clinical signs and symptoms,23 and the symptom of dizziness is uncommon.30 It is unlikely that in people with persistent signs and symptoms following a whiplash injury, the symptom of dizziness is due to trauma to the vertebral artery. However, owing to the considerable danger such an event poses, it should be noted as a possibility and should always be considered in the differential diagnosis.
Disturbances to structures influencing sensorimotor control
The forces generated during a whiplash injury can potentially cause definitive damage to many neck structures,31 and thus be a primary source of altered proprioceptive input to the sensorimotor control system.32 The forces may also be sufficient to produce CNS and/or peripheral vestibular dysfunction. Relatively slow crash speeds, of up to 15 kilometres per hour, have been shown to generate 8g of force on the head and neck.33 In a controlled study involving primates, the forces that were artificially reproduced resulted in cerebral concussion, and brainstem and cranial nerve stretch in 50% of the cases.34 However, in other crash testing, humans have been exposed to 10g without apparent effects on the CNS or peripheral vestibular apparatus.35 It is thought that higher forces of up to 25g are necessary to cause damage to these structures in humans.36 Thus, disturbance of the cervical afferents is considered the most likely primary source of dizziness, visual disturbances and sensorimotor control disturbances, particularly in slow-speed, impact collisions that cause a whiplash injury.
Brain injury
A brain injury may occur concomitantly with a whiplash injury, especially when the forces are strong and result in a direct blow to the head. However, it is generally felt that brain injury is unlikely with a pure whiplash injury.37 Studies using various technologies have been relatively unsuccessful in identifying the presence of brain injury in people with whiplash not reporting an associated mild head injury.10, 37–39 Although some correlations between cognitive deficits, anxiety and pain have been demonstrated, no actual deficits in neuropsychological testing relating to altered brain function have been substantiated.39 Gimse et al.40 demonstrated reading difficulties in patients with whiplash without any evidence of brain injury, and concluded that cognitive and reading problems were likely to be due to abnormal afferent input from the cervical spine rather than a brain injury. Wenngren et al.41 investigated the prevalence of brain/brainstem dysfunction following a whiplash injury and concluded that in only a small proportion of patients with very severe symptoms could these be explained by lesions to the brain/brainstem.
Damage to the peripheral vestibular apparatus
Forces generated during a whiplash injury, especially when there is concomitant mild head injury, could result in at least three possible peripheral vestibular causes of dizziness and disturbances to postural control: benign paroxysmal positional vertigo (BPPV), damage to the endolymphatic sac which could cause hydrops (Ménière’s disease), or rupture of the otic capsule window resulting in a perilymph fistula. In a retrospective review,36 it was estimated that 35% of people had some combination of these conditions as a consequence of inner ear concussion associated with a whiplash injury.
Debate continues as to the frequency of vestibular disorders following a whiplash injury. High percentages (up to 85%) of peripheral vestibular dysfunction have been reported.42 However, these studies often lacked control groups and the conclusion that vestibular dysfunction was the cause was based on clinical patterns rather than definitive objective measures. In studies where objective measures have been used, reports of BPPV and perilymph fistula have been suggested to occur in as little as 5% to in as much as 25% of patients.43 Isolated reports of acute vestibular pathology occurring shortly after a pure whiplash injury have also been documented.44
Fischer et al.12 reported normal vestibular test results in most of their subjects with whiplash, although vestibular hyperactivity was seen in 53% of subjects. They proposed that this could be due to limited neck movement, secondary to neck pain, with subsequent vestibular–ocular reflex enhancement. Fischer et al.45 also found that 38% of subjects hyperventilated, suggesting a possible relationship between stress, anxiety and vestibular findings. Solarino et al.46 recently suggested that increased latency in vestibular evoked potentials in those with a whiplash injury may be a result of a primary disorder of the vestibulocollic reflex rather than actual peripheral vestibular dysfunction.
Recent studies have also compared symptoms and sensorimotor deficits in those with whiplash compared to those with a discrete unilateral peripheral vestibular dysfunction and demonstrated that subjects with whiplash had differences in performance in both balance tests and eye movement tests. Additionally, they reported different characteristics of dizziness.47 Secondary adaptive changes in the vestibular system are possible, but these findings suggest that these are not the primary cause of the deficits in patients following a whiplash injury.
Damage to vision—post-trauma visual syndrome
Damage to the ambient visual system has also been suggested as a possibility following a whiplash injury.48 The ambient visual system is important for knowledge of where you are in space rather than what you are looking at (focal vision) and provides general information needed for balance, movement, coordination and posture. Photophobia, convergence insufficiency, accommodation insufficiency and eye alignment malfunctions, such as cross eyes, rotation and one eye up one down, are thought to be due to altered ambient vision and have been demonstrated in some people following a whiplash injury.49, 50 Together these symptoms have been labelled as post-trauma visual syndrome, which is thought to result in symptomatic complaints of dizziness, visual disturbances and alterations in head and eye movement and postural stability.48 Research into this area is in its infancy and currently lies in the domain of behavioural optometry.
Damage to cervical afferents
Afferent input from nociceptors and mechanoreceptors in the cervical region, as with those throughout the body, mediates pain, temperature, pressure, touch and proprioceptive information to the nervous system. The abundant cervical receptors in the muscles and joints of the cervical spine, as well as their central and reflex connections to the vestibular, visual and postural control systems, suggest that these receptors have an important role in providing information for general sensorimotor control affecting balance, and head and eye movement control.51, 52 Conflict between the converging input from the different sensory systems or a sensory mismatch is the mechanism thought to be responsible for disturbances in sensorimotor control following interference to the cervical afferents, such as could occur following a whiplash injury.
Cervical receptors
Cervical receptors are important for sensorimotor control. Muscle receptors, particularly muscle spindles, are considered to be of most significance as they are found in high densities in the cervical region. Muscle spindle density is highest in the muscles of the suboccipital region, particularly in the deeper part of these muscles, with up to 240 muscle spindles per gram of muscle.53, 54 In a study of human neck muscles, distinct morphological features and the composition of the muscle spindles in the deep neck muscles were considered to demonstrate their influence on both movement precision and proprioceptive information for the control of head position and eye–head coordination.55 Others also believe that these small deep muscles may not function as traditional muscles but rather as monitors of proprioceptive function.53
While there are higher numbers of mechanoreceptors in the upper cervical compared to the lower cervical joints, their numbers are much lower in comparison to those in the muscles, and it has been suggested that joint receptors only supplement information from the abundant muscle spindles.56 Nevertheless, joint and ligament receptors are thought to be important for control of feed-forward muscle activity, by way of complex sensory feedback mechanisms involving both ascending pathways and reflex activity via the gamma muscle spindle system.57 Thus, joint and ligament receptors are likely to impact on sensorimotor control through their influence on the muscle spindle system.58
Reflex and central connections
The neck is not unique in having central connections that contribute to local proprioception and neuromuscular control but, compared to other areas of the body, the receptors also play an important role in the mediation of postural reflex responses and the subsequent connections between the visual and vestibular apparatus. Neck afferents have been shown to project to the medial and lateral vestibular nuclei59 and the superior colliculus, a reflex centre for coordination between the ambient visual system and neck movement.60 It has been suggested that cervical afferents can also influence the sympathetic system via beta receptors in the cervical muscles and vice versa.61 Recently, this link between the cervical afferents and the sympathetic nervous system suggests an association between elevated psychological stress and altered sensorimotor control.17
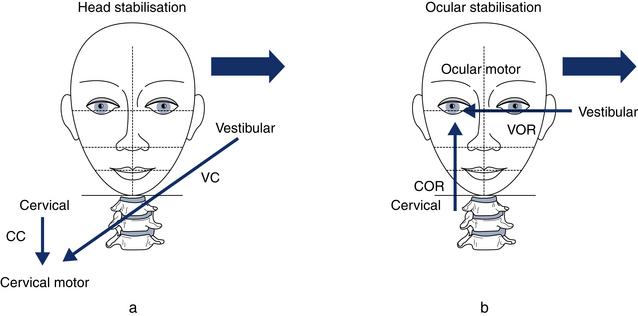
Synaptic connections from the cervical receptors to other areas also play an important role in neck reflex activity. The neck afferents are involved in three posturally related reflexes influencing head and eye movement and postural stability, the cervicocollic reflex (CCR), the cervico-ocular reflex (COR) and the tonic neck reflex (TNR). These reflexes work in conjunction with other reflexes acting on the neck and eye musculature, stimulated by vestibular and visual input, for coordinated stability of the head and eyes (Fig 7.2).
The CCR causes reflex activation of neck muscles when the muscles are stretched with movement of the head in relation to the body. The CCR integrates with the vestibular system via the vestibulocollic reflex (VCR) to assist in the maintenance of head position and minimise head rotation.62
The COR works together with the vestibular ocular reflex (VOR) and optokinetic reflex (OKR) to act on the extraocular muscles (via the extraocular nuclei) and assist in maintaining eye position, such that head movement results in equal but opposite movement of the eyes. Through this connection, clear vision is maintained during head movement. The COR is evoked through stretching the neck muscles and acts on the extraocular muscles via their nuclei.63
Cervical afferents are also thought to influence the OKR through the convergence of information from the cervical and optokinetic systems on the vestibular neurons. In turn, eye movements can generate activation of the cervical muscles while the head is still. A close relationship between the deep cervical extensors/rotators and horizontal eye movement has also been observed,64 and it is thought that this synergy is mediated by tecto-reticulo-spinal nuclei at the brain stem.65
The TNR mediates alterations in limb muscle activity when the body moves with respect to the head and acts to maintain a stable posture. It is integrated with the vestibulospinal reflex (VSR) to achieve postural stability.66 Again, it is thought that neck muscle spindle afferents primarily generate the signals for this reflex.67
Effects of artificial disturbance of cervical afferentation on postural control
The association between artificial disturbances to cervical afferentation and disturbances to sensorimotor control has been demonstrated in several ways. Sectioning of the cervical dorsal root ganglions or injections of anaesthetic into deep neck structures has also been shown to cause nystagmus and severe ataxia.68, 69 Less invasive techniques, such as neck muscle vibration, which is considered to primarily stimulate the muscle spindle afferents, has been shown to induce prolonged eye position changes, and visual and head illusory movements,70, 71 produce increased body sway,72 and to influence velocity and direction of gait and running.73, 74 Similarly, experimentally induced pain, muscle fatigue and restriction of range of motion have also demonstrated altered sensorimotor control.75, 76 The induced sensorimotor changes are similar to those seen in people following a whiplash injury, which provides further support for the neck as a primary cause of the disturbances.
Mechanisms responsible for altered sensorimotor control due to disturbed cervical afferentation
Conflict between the converging input from the different sensory systems or a sensory mismatch is the mechanism thought to be responsible for disturbances in sensorimotor control following interference to the cervical afferents, such as could occur after a whiplash injury.14 Since information from the muscle spindles is of primary importance for cervical afferent information, and this input interacts with vestibular and visual information, a changed or disturbed sensitivity of the muscle spindles may result in the complaint of dizziness and visual disturbances, as well as altered cervical joint position and movement sense, knowledge of head position, eye–head coordination and/or balance following a whiplash injury.
There is also some evidence that the neck may directly influence the function of the VOR and VCR.46 It is proposed that altered neck input could give rise to a mismatch of sensory input, as well as asymmetry of these reflexes.12, 46
Mechanisms of cervical afferent disturbance
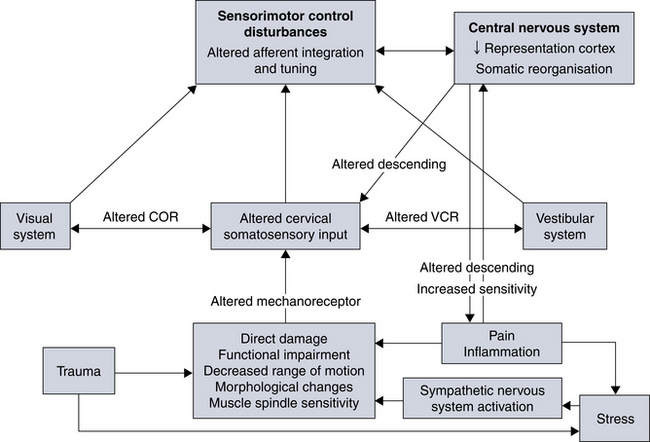
There appears to be evidence that sensorimotor control disturbances may result from either a decrease or an increase in cervical afferent activity. The crucial factor appears to be that afferent input is altered and abnormal. Studies where anaesthetics are applied to the cervical region suggest that a decrease in afferent activity is responsible for the symptoms.69 However, others suggest that ‘over’-excitation of the cervical afferents may create problems.77 Of specific relevance to whiplash has been the postulation that the injury may cause a perpetual cycle of incorrect afferent information.78, 79 The sudden barrage of input from the cervical proprioceptors to the sensorimotor control system could create incorrect afferent information followed by compensatory muscle tension generated by the sensorimotor control system to restore postural stability. This, in turn, could lead to further altered neck afferent input, perpetuating the cycle. The situation may be complicated further by the effects of pain and inflammation resulting from damage to neck structures.
Causes of abnormal cervical afferent input following a whiplash injury
The combined influence of direct trauma and/or functional impairment of the receptors as well as the role of changed reflex activity and somatosensory reorganisation within the CNS should not be underestimated in the role of sensorimotor control disturbances following a whiplash injury (Fig 7.3).
Alterations in the neuromuscular control of muscles, through desensitising the mechanoreceptors, are likely to be particularly important causes of ongoing disturbances to sensorimotor control.80 Neuromuscular control can become impaired in those with neck pain via several mechanisms, including inhibition of the deep stabilising musculature,81 altered feed-forward preparatory muscle activity,82 compensatory increased activity in the superficial muscles,83 and altered neuromuscular efficiency and fatigability.83 Similarly, morphological changes in cervical muscles, particularly the suboccipital muscles, in those with whiplash may also alter their proprioceptive capabilities.84, 85 It is possible that such changes occur in the acute stages and persist despite the patient reporting recovery from pain.86 Recent studies have demonstrated the direct deleterious effects of neck extensor muscle fatigue or pain on standing balance.75, 87 Specifically, McPartland et al.88 determined a significant correlation between poor balance control and fatty infiltration of the rectus capitis posterior minor muscle.
Altered reflex responses have also been suggested as possible causes of sensorimotor control disturbances following a whiplash injury. Decreased range of motion,89 voluntary guarding or increased superficial muscle activity83, 90 in participants with persistent WAD could possibly lead to an alteration in the gain of the CCR and perhaps secondary changes to VCR activity.46 Further, evidence of altered COR activity and lack of compensatory changes with the VOR have also been noted in some people with persistent whiplash, and are thought to be factors contributing to altered sensorimotor control.91
Inflammatory mediators released following the injury may also activate chemosensitive nerve endings in joints and muscles, leading to altered muscle spindle activity.92, 93 In addition, the effects of inflammation on nociceptors and mechanoreceptors locally, at the spinal cord and within the CNS can also influence the modulation of afferent input and, thus, both neuromuscular and sensorimotor control.57, 94
At the local level, an increase in nociceptor input occurs as a result of a peripheral release of chemical mediators following injury. This increase in nociceptive input may also cause a decrease in non-nociceptive input; that is, an alteration of afferent input to the sensorimotor control system. Such changes may also result in perpetuating pain, as non-nociceptive input normally has an inhibitory effect on pain modulation.95
Increased nociceptive input from the periphery can also lead to altered processing in the spinal cord and brain.96 In chronic pain, mechanical receptors can continue to be pain-sensitive, possibly due to changes in the CNS and decreased central inhibition.97 This generalised sensitivity to a variety of stimuli often occurs at both local and remote regions to the original injury and has been shown to be a particularly early feature in some subjects with whiplash, as well as one of the predictive features for chronicity.98 In turn, this may lead to further prolonged disruption of afferent input from the cervical region.
Experimental pain has also been shown to influence muscle function.94 Experimental neck pain in rats has demonstrated a direct and long-lasting influence on muscle spindle activity via excitation of chemosensitive afferents.92, 93 This can also alter reflex muscle activity and adversely affect postural stability.75 Pain has also been shown to alter spinal inhibitory effects, through the effect on the somatosensory cortex and other subcortical levels.94 There is also evidence to suggest a possible role for pain in subcortical and cortical reorganisation at many levels of the somatosensory system in humans, and that both the removal of afferent inputs and the enhancement of nociceptive inputs could contribute to this neural reorganisation.99
Further, it is not uncommon for subjects with persistent whiplash to have elevated general and specific anxiety related to the accident.100 Recently, it has been suggested that psychological stress may also influence cervical muscle spindle sensitivity via activation of the sympathetic nervous system and, thus, also contribute to altered cervical afferent input following a whiplash injury.17
In summary, several mechanisms could disturb cervical afferents in patients with neck pain following a whiplash injury. These include inflammation, direct damage, functional impairment and/or morphological changes to musculature, pain and psychological distress. These may alter proprioceptive capabilities, joint mechanics, CNS representation and muscle spindle sensitivity, and thus affect cervical afferent input to the sensorimotor control system. This, in turn, may also influence reflex connections to the visual and vestibular systems and subsequently cause secondary disturbances. Evidence to date would suggest altered cervical afferent input and its effect on the sensorimotor control system is the most likely primary cause of dizziness, unsteadiness, visual disturbances and altered balance, eye and head movement control that has been demonstrated in those following a whiplash injury, especially when there has been no associated mild head injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree