Dizziness and Vertigo (Case 57)
Lana Zhovtis Ryerson MD and Stephen Krieger MD
Case: A 34-year-old woman presents to the ED with dizziness. She states that 2 days ago she began to feel a “spinning sensation” and was walking around “as though she were drunk.” These symptoms worsened the day before admission, when she developed nausea and vomiting and had increasing difficulty walking. She has no significant past medical history. On exam she has beating nystagmus in all directions of gaze, worse when looking to the right. She has a slightly flattened right nasolabial fold. She has full strength and an intact sensory exam, but on coordination testing she has significant postural instability, as well as dysmetria in the right arm. She is unable to tandem walk, falling to the side.
Differential Diagnosis
Vertigo | Dizziness/presyncope/light-headedness |
Benign paroxysmal positional vertigo (BPPV) | Orthostatic hypotension |
Acute labyrinthitis/vestibular neuritis | Cardiac arrhythmia |
Meniere disease | Vasovagal disorder |
Cerebellar infarction or hemorrhage | Intoxication/medication side effects |
Perilymphatic fistula | Anxiety |
Speaking Intelligently
Although prevalence studies vary in their definition of the symptom, dizziness is common in all age groups, and its prevalence increases modestly with age. While peripheral vestibular etiologies are among the most common causes, as many as 25% of patients with risk factors for stroke who present to the emergency medical setting with the combination of vertigo, nystagmus, and postural instability may have a stroke affecting the cerebellum.
For most patients the symptom of dizziness resolves spontaneously, but an important minority of patients can develop chronic, disabling symptoms. Patients with chronic dizziness may benefit from an approach aimed at identifying and managing treatable conditions, whether etiologic or contributory. This approach may include correcting visual impairment, improving muscle strength, adjusting medication regimens, identifying and treating psychological comorbidities such as anxiety and depression, and instructing patients on vestibular exercises.
PATIENT CARE
Clinical Thinking
• Vertigo is an illusory sensation of motion of either oneself or one’s surroundings.
History
When evaluating a complaint of dizziness to establish if there is frank vertigo or presyncope, questions to consider include the following:
• Is there a true sensation of movement or spinning?
• Is there a feeling of faintness and light-headedness?
• Are there vague, persistent feelings of imbalance?
• What are the associated characteristics?
• Nausea/vomiting may accompany vertigo.
• The sensation of warmth, diaphoresis, and visual blurring may indicate presyncope.
• Palpitations, dyspnea, or chest discomfort can indicate a cardiac cause.
• What is the duration of the episodes, and what are any exacerbating factors (e.g., head movement)?
• Has syncope ever occurred during an episode?
• Do episodes occur only when the patient is upright, or do they occur in other positions?
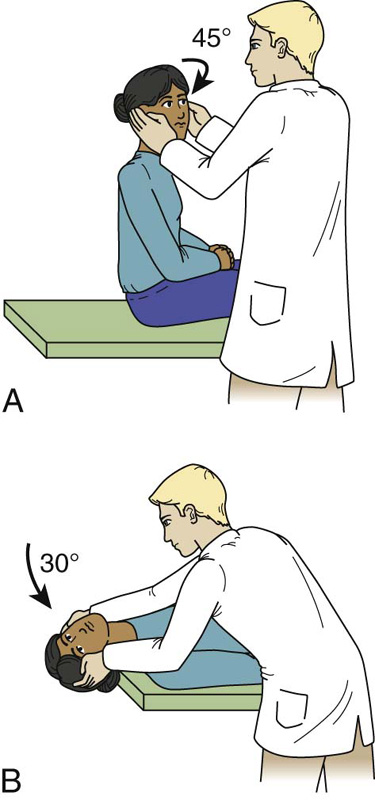
Physical Examination
Feature of Nystagmus | Peripheral (Labyrinth or Nerve) | Central (Brainstem or Cerebellum) |
Latency of nystagmus | 3–40 sec | None: immediate vertigo and nystagmus |
Fatigability of nystagmus | Yes | No |
Direction of nystagmus | Unidirectional, often rotatory | Can be bidirectional, unidirectional, or vertical |
Visual fixation | Inhibits nystagmus and vertigo | No inhibition |
Intensity of vertigo | Severe | Mild |
Tinnitus and/or hearing loss | Often present | Usually absent |
Associated CNS abnormalities | None | Extremely common (e.g., diplopia, hiccups, cranial neuropathies, dysarthria) |
Common causes | BPPV, vestibular neuritis, labyrinthitis, Meniere disease | Infarction, hemorrhage, multiple sclerosis, neoplasm |
Tests for Consideration
$11, $15, $185, $85 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



