Recreational scuba diving is a growing sport with some unique considerations for the sports medicine team.
The number of annual diving certifications has tripled in the past 20 years worldwide (38).
There are roughly 3 million sport divers in the United States alone (38).
Divers may seek medical care for a disorder acquired in a remote location with injuries or illnesses unique to diving and the underwater environment.
Improper diagnosis and treatment of some diving injuries can result in catastrophic outcomes, particularly involving the brain and spinal cord.
The sports medicine physician must be aware of “fitness to dive” recommendations for patients of all ages who are seeking medical clearance to dive.
In contrast to most other sports, recreational diving places athletes at increased risk of injury or illness primarily due to environmental extremes and hazards in the underwater setting.
The most significant environmental exposure in diving is the increased ambient pressure.
Pressure increases in a linear fashion with depth underwater (Table 90.1) (28).
Exposure to increased pressure can result in several pathophysiologic changes as described by the common gas laws outlined later (47).
Descent: Diving deeper involves increases in pressure of 1 atmosphere per 33 feet of sea water. Equilibration of pressure in gas-filled spaces is critical during this phase.
Bottom time: The amount of time spent underwater (traditionally referred to time spent at lowest depth). Bottom time influences amount of gas absorption in tissues.
Ascent: Moving up toward the surface involves decreases in pressure and the release of absorbed gas back into local tissues and the bloodstream.
Surface interval: Time between dives. This time allows the body to reacquire homeostasis, especially with respect to tissue gas concentration. Dive injuries may not present until the diver surfaces.
Decompression stop: A pause in ascent following a deep dive that allows for absorbed inert gas bubbles to be safely eliminated from tissues.
No-decompression dive: A dive profile that does not require decompression based on limited depth and bottom time. Most sport divers perform no-decompression dives to mitigate risk of decompression sickness.
Barotrauma is defined as the tissue damage that results from an inability to equalize pressure in a gas-filled space (e.g., middle ear).
During ascent and descent, the body is exposed to changes in ambient pressure.
According to Boyle’s law, as ambient pressure increases during descent, the volume of gas-filled spaces decreases.
In the ear, the tympanic membrane is deflected inward to the point of rupture unless air is allowed to enter the middle ear via the eustachian tube (24).
Middle ear barotrauma (“middle ear squeeze”) is the most common diving injury, occurring in 30% of first-time divers and 10% of experienced divers.
Manifests as acute onset of ear pain.
Is sometimes associated with vertigo and conductive hearing loss.
Clinical findings range from injection of the tympanic membrane to hemotympanum, with or without ruptured tympanic membrane (15).
Sinus barotrauma (“sinus squeeze”) is another common diving injury usually resulting from transient nasal pathology or chronic sinusitis.
A relative negative pressure in a sinus cavity is caused by blockage of the sinus ostium during descent.
Negative pressure is followed by engorgement and mucosal edema, which may cause bleeding into the sinuses.
Manifests as acute onset of facial pain with epistaxis (39).
Table 90.1 Effects of Depth on Ambient Pressure
fsw
ata
mm Hg
psi
0
(sea level)
1
760
14.7
33
2
1,520
29.4
66
3
2,280
44.1
99
4
3,040
58.8
132
5
3,800
73.5
ata, absolute pressure in atmospheres; fsw, feet of sea water; mm Hg, millimeters of mercury; psi, pounds per square inch.
SOURCE: Reproduced, with permission, from Lynch JH, Bove AA. Diving medicine: a review of current evidence. J Am Board Fam Med. 2009;22:399-407. Available from: doi:10.3122/jabfm.2009.04.080099. Copyright © 2012 American Board of Family Medicine. All Rights Reserved.
Treatment for middle ear and sinus barotrauma includes:
Decongestants and analgesics.
Systemic antibiotics for prophylactic treatment of otitis media may be considered in middle ear barotrauma with tympanic membrane perforation.
Tympanic membrane rupture must be allowed to heal completely prior to diving again.
Prevention of middle ear and sinus barotrauma consists of:
Careful attention to pressure equilibration using the Valsalva maneuver during descent.
Slow, feet-first descent.
Nasal and/or systemic decongestants such as oxymetazoline and pseudoephedrine prior to diving may be helpful. They must be used with caution to avoid the rebound effect sometimes associated with a reverse block during ascent at the end of the dive. As the medication effect diminishes, nasal passages may become congested and allow for sinus ostial blockage and pain with ascent (25).
Avoid diving with an upper respiratory infection or rhinosinusitis, which contribute to ostial insufficiency and may increase risk for barotraumas (14).
Inner ear barotrauma is a condition related to middle ear barotrauma.
Forceful attempts to equalize the middle ear with the Valsalva maneuver may rupture the round or oval window causing perilymph leakage.
Manifests as acute sensorineural hearing loss, tinnitus, and vertigo.
Treatment is not recompression therapy, but rather bed rest, head elevation, avoidance of straining, and referral to an otolaryngologist.
A detailed dive history is helpful in distinguishing inner ear barotrauma from inner ear decompression sickness (24).
According to Boyle’s law, during ascent, as ambient pressure is reduced, gas inside the lungs will expand.
If a diver breathing compressed air at depth does not allow the compressed air in the lungs to escape by exhaling, or if air empties slowly from a lung segment due to obstructive pulmonary conditions, then the gas will expand on ascent (as ambient pressure falls). This causes alveoli to rupture.
After alveolar rupture, the air under pressure will then escape the alveoli and rush into surrounding tissues resulting in mediastinal or subcutaneous emphysema or pneumothorax.
In the most severe cases, air will enter the bloodstream via pulmonary veins, traveling through the left heart as an arterial gas embolism (AGE).
Air bubbles distribute throughout the arterial circulation and reach the brain where they occlude blood flow, compromise the blood-brain barrier, and result in stroke-like events (36).
Almost all cases of AGE present within 5 minutes of ascent.
AGE manifests as gross neurologic deficits including stupor, bilateral or unilateral motor and sensory changes, unconsciousness, visual disturbances, vertigo, convulsions, and (in about 5%) complete cardiovascular collapse (Table 90.2) (37).
The greatest change in lung volume per change in depth occurs nearest the surface.
It is possible for divers breathing compressed air in a pool as shallow as 4 feet to develop pulmonary barotrauma if they ascend to the surface while breath-holding at maximum lung volume (7).
The majority of individuals with AGE fully recover with prompt recompression therapy (36).
Decompression sickness (DCS) is caused by bubble formation in blood and tissues.
As ambient pressure increases at depth, the partial pressures of inspired gases increase proportionately.
Inert gas, primarily nitrogen, is dissolved in tissues, creating a supersaturated state in the body.
If ascent is too rapid, the dissolved nitrogen in blood and tissues will become supersaturated and form bubbles.
Table 90.2 Summary of Diving-Related Conditions
Condition
Presentation
Dive History
Prevention/Treatment
Barotrauma
Middle ear
Acute ear pain, vertigo, tympanic membrane rupture
Usually during descent
Slow equalization on descent; decongestants, consider antibiotics for tympanic membrane perforation
Inner ear
Acute vertigo, nausea, vomiting, hearing loss
Usually during descent
Bed rest, elevated head, avoidance of Valsalva, otolaryngology consult
Sinus
Acute facial pain, epistaxis
Usually during descent
Slow equalization on descent; decongestants
Arterial gas embolism
Stupor, coma, focal weakness, visual disturbances
Immediately upon surfacing or during ascent
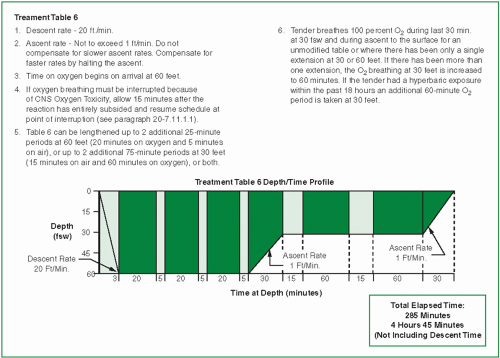
100% oxygen, supportive care, U.S. Navy Table 6 Algorithm
Decompression sickness
Type I
Poorly localized joint pain, rash, itching
Significant time at depth; 50% develop symptoms within 1 h of surfacing, 90% within 6 h
100% oxygen, supportive care, U.S. Navy Table 6 Algorithm
Type II
Numbness, dizziness, weakness, gait abnormality, hypoesthesia
Significant time at depth; 50% develop symptoms within 1 h of surfacing, 90% within 6 h
100% oxygen, supportive care, U.S. Navy Table 6 Algorithm
SOURCE: Reproduced, with permission, from Lynch JH, Bove AA. Diving medicine: a review of current evidence. J Am Board Fam Med. 2009;22(4):399-407. Copyright © 2012 American Board of Family Medicine. All Rights Reserved.
Bubbles cause tissue injury through mechanical effects, vascular occlusion, and activating the clotting cascade and inflammatory mediators.
Bubbles are often detected initially in the venous system and may pose a further risk for systemic injury by entering the arterial circulation through a patent foramen ovale (PFO), which produces a right-to-left cardiac shunt.
Bubbles entering the arterial circulation via a shunt will produce symptoms similar to AGE (48).
The incidence of DCS among recreational scuba divers is approximately 2-3 cases per 10,000 dives (41).
DCS manifests with a wide array of signs and symptoms and is typically classified into type I and type II DCS (see Table 90.2).
Type I (nonsystemic or musculoskeletal DCS) is characterized by the absence of neurologic and other systemic symptoms and usually manifests as:
□ Musculoskeletal symptoms, such as pain that is often dull or throbbing and poorly localized around a joint; the shoulder and elbow are the most common sites.
□ Cutaneous manifestations such as skin rash and pruritus. Less common is cutis marmorata or skin marbling, which may be a harbinger of more serious symptoms requiring recompression therapy.
□ In 95% of those affected, type I DCS presents within 6 hours of surfacing.
□ Treatment for type I or musculoskeletal DCS is recompression (see Fig. 90.1).
□ Joint pain is rapidly relieved with recompression therapy.
□ Cutaneous manifestations usually resolve spontaneously in 12-24 hours (31).
Type II (neurologic or systemic DCS) describes DCS, which affects the neurologic, vestibular, or pulmonary systems.
□ Neurologic involvement is most common among sport divers and can be due to either spinal cord or cerebral involvement.
Half of patients develop symptoms within 1 hour of surfacing, and 90% report symptoms within 6 hours.
The most common presenting neurologic symptoms include numbness, dizziness, weakness, gait abnormality, and hypoesthesia (37).
□ Inner ear DCS (the “staggers”) may be due to bubble formation in the semicircular canals and presents as acute vertigo, nystagmus, tinnitus, and nausea with vomiting.
□ Pulmonary DCS (the “chokes”) is a rare condition likely caused by a massive pulmonary gas embolism.
This usually follows a rapid or uncontrolled ascent.
Manifests as immediate substernal pain, cough, and cardiovascular shock resembling adult respiratory distress syndrome (ARDS) (20).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree