Fig. 23.1
Right shoulder posterior view artwork demonstrating the two compression sites for the suprascapular nerve (Copyright Kevin D. Plancher MD 2015)
Anatomy Suprascapular Nerve
The suprascapular nerve has been classically thought to arise from the upper trunk of the brachial plexus (C5–C6) at Erb’s point; however, in 25 % of individuals, the C4 nerve root also contributes to this nerve [6, 7] (Fig. 23.2). As the nerve approaches the suprascapular notch, the accompanying suprascapular artery diverges [8]. At this point, the suprascapular nerve travels under the transverse scapular ligament as it enters the suprascapular notch. The suprascapular artery traverses over the transverse scapular ligament; however, in rare instances, the artery travels with the nerve [9]. As the nerve then courses laterally along the supraspinatus fossa, it approaches the posterior glenoid rim, travels around the scapular spine, and descends into the infraspinatus fossa after it passes under the spinoglenoid ligament (inferior transverse scapular ligament) [10] (Fig. 23.3). The suprascapular nerve then gives rise to 2–4 branches to the infraspinatus muscle belly.
Fig. 23.2
Right shoulder anterior view artwork of the suprascapular nerve arising from the upper trunk of the brachial plexus (Copyright Kevin D. Plancher MD 2015)
Fig. 23.3
The suprascapular nerve descending into the infraspinatus fossa passing under the spinoglenoid ligament (Copyright Kevin D. Plancher MD 2015)
Some authors have described two types of spinoglenoid ligaments: Type I, a thin indistinct band of tissue, and Type II, a well-formed ligament. We performed a cadaveric study and found that the spinoglenoid ligament was present in 100 % of specimens. We also found that it has attachments to the glenohumeral joint capsule which can contribute to compression of the suprascapular nerve at the spinoglenoid ligament upon internal rotation of the shoulder. The nerve itself is approximately 2.5 cm away from the glenoid rim (posterior superior) and is located approximately 4 cm from the posterolateral corner of the spine of the scapula [4]. The spinoglenoid ligament is quadrangular in shape and originates from the posterior glenoid neck and glenohumeral capsule to insert as a bilaminar “ligament” into the scapular spine (Fig. 23.4). Recent clinical studies together with previous anatomic dissections suggest that the suprascapular nerve contributes an appreciable sensory innervation to the shoulder AC joint. These sensory contributions may explain pain upon traction or compression of the nerve as well as upon repair of a massive rotator cuff tear with advancement [11].
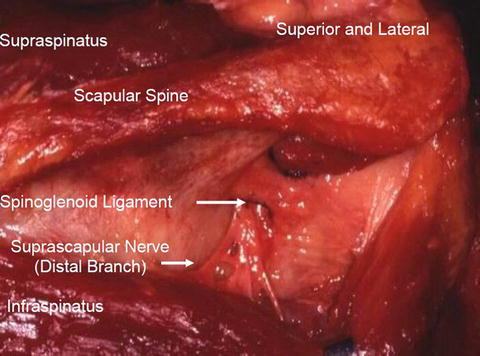
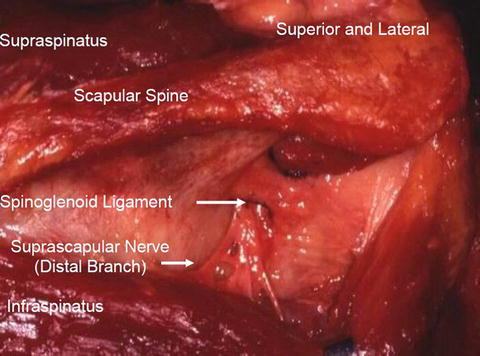
Fig. 23.4
The spinoglenoid ligament, quadrangular in shape, demonstrated in the posterior view of a right shoulder dissection. Note the distal branch of the suprascapular nerve compressed (Copyright Kevin D. Plancher MD 2015)
Pathophysiology
Isolated compression or injury to the suprascapular nerve may occur at the spinoglenoid ligament (Fig. 23.5). While the more common site of suprascapular entrapment neuropathy is at the transverse scapular ligament in the suprascapular foramen or notch, clinical presentation and diagnosis of compression at the most distal site have been well recorded (Fig. 23.6). Several mechanisms have been proposed and previously discussed above. While most commonly thought of in the overhead athletes, injury to this nerve may occur from repetitive traction and microtrauma [3, 4, 12–14]. The spinoglenoid ligament has also been demonstrated to tighten when the shoulder is in a position for overhead throwing, resulting in increased pressure on the suprascapular nerve [15] (Fig. 23.7). Early investigators speculated that injury to this nerve occurred by intimal damage from microemboli in the vasa nervorum [16]. While intriguing, there is no firm science to support this contention. A stenotic suprascapular notch, an ossified spinoglenoid ligament, or even superiorly oriented fibers of the subscapularis muscle may cause a suprascapular nerve compression [8, 17]. Compression of the nerve at the spinoglenoid ligament has been noted by many authors to be caused by a soft tissue mass or ganglion cyst as a result of some form of a labral or capsule injury. While previously treatment of a cyst-associated compression was labral repair [18, 19], the senior author recommends decompressing the ganglion from the posterior aspect of the shoulder without labral repair to yield excellent results (Fig. 23.8a–f). Compression by a ganglion cyst or soft tissue mass has been known to occur because of the relatively fixed position of the suprascapular nerve combined with the close proximity of the infraspinatus muscle to the glenohumeral joint. A ganglion cyst may form when the labral-glenoid junction tears and synovial fluid is transported into the soft tissues via a one-way valve effect. This mechanism is very similar to the formation of meniscal cysts in the knee [20].
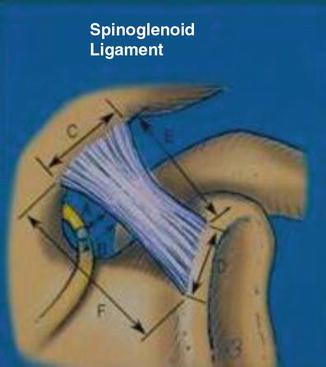
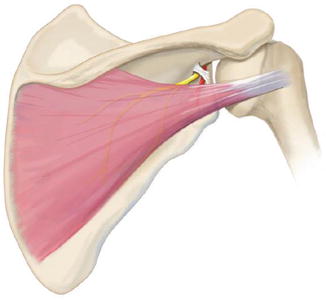
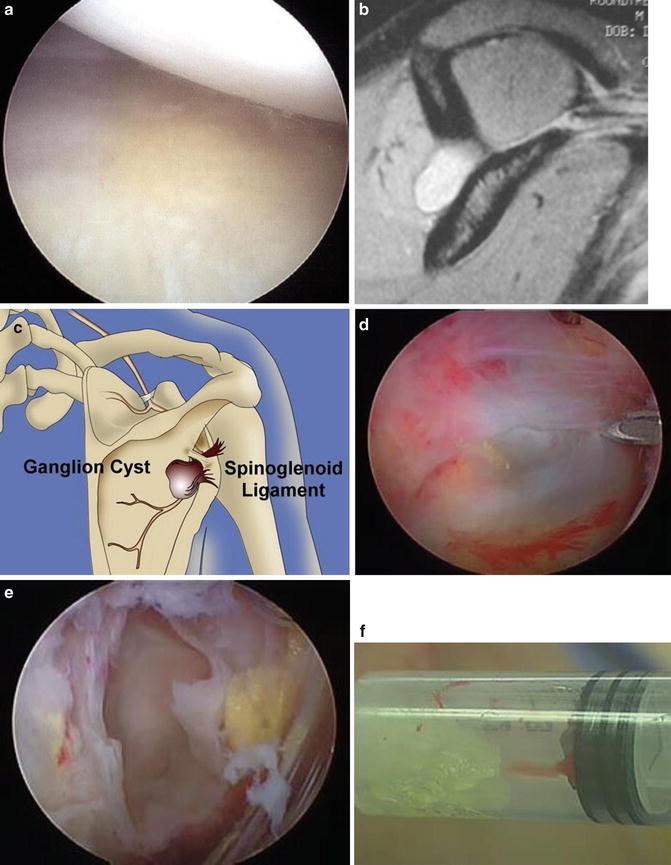
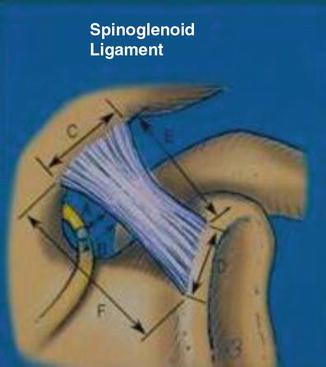
Fig. 23.5
Artwork demonstrating the relationship of the spinoglenoid ligament in a previous published study with investigation of space available between the suprascapular nerve and the spinoglenoid ligament. Note the attachment to the spine of the scapula (Copyright Kevin D. Plancher MD 2015)
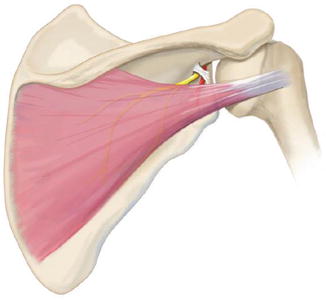
Fig. 23.6
Artwork demonstrating suprascapular nerve entrapment at the spinoglenoid ligament. Note the medial course of the nerve as it wraps around the spinoglenoid notch (Copyright Kevin D. Plancher MD 2015)
Fig. 23.7
The voltage change with throwing motion with intact spinoglenoid ligament. Note the follow-through or crossed-arm adduction position yields the highest pressure change at the spinoglenoid ligament [(Copyright Kevin D. Plancher MD 2015) Previously published in Plancher et al. Posterior shoulder pain: A dynamic study of the spinoglenoid ligament and treatment with an arthroscopic release of the scapular tunnel. Arthroscopy 23(9): 2007 991–998; Fig. 4]
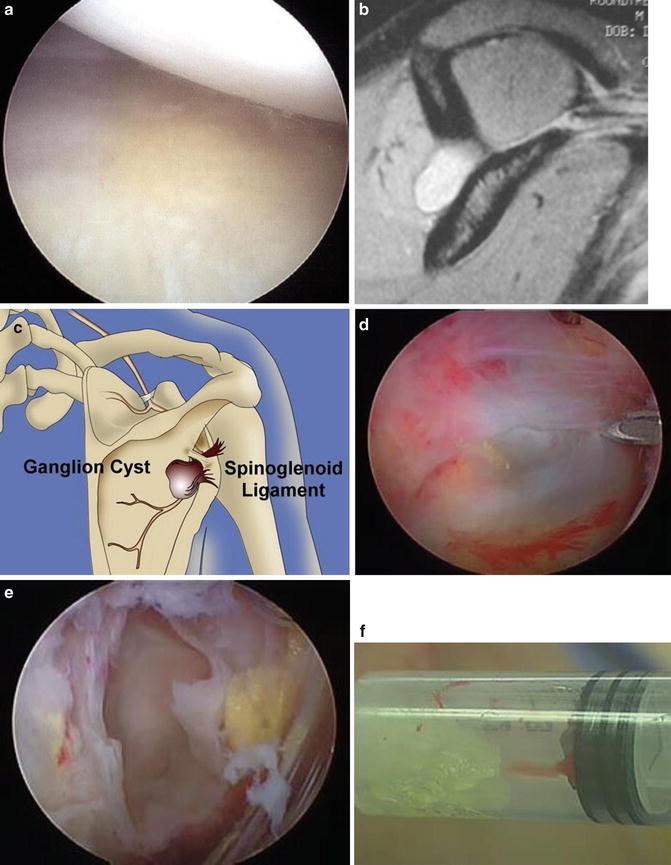
Fig. 23.8
(a) Arthroscopic view of a ganglion cyst decompressed from the outside emitting its contents intra-articularly through a posterior inferior perforation in the labrum. (b) Sagittal oblique MRI demonstrating a ganglion cyst compressing the suprascapular nerve at the spinoglenoid notch. (c) Artwork of posterior view of right shoulder demonstrating a classic ganglion compressing the spinoglenoid ligament at its notch. (d) Posterior view of bulging ganglion cyst located at the spinoglenoid notch. (e) Decompressed ganglion cyst at the spinoglenoid notch prior to complete excision of its root. (f) Syringe containing the contents of the ganglion cyst commonly seen on MRI compressing the suprascapular nerve at the spinoglenoid ligament (Copyright Kevin D. Plancher MD 2015) (Reprinted with permission from Jonathan Ticker, MD)
While rare, a patient may sustain a neuropathy from a parsonage Turner syndrome, although it is more common for this viral neuritis to attack other nerves. Whatever the mechanism, compression or injury to the suprascapular nerve at the spinoglenoid ligament will result in infraspinatus weakness. If sustained long term, atrophy of the infraspinatus muscle will ensue with little if any probability of return to normal muscle strength expected.
Patient Profile
History
Patients with compression of the suprascapular nerve at the spinoglenoid notch comprise a unique group of individuals, more commonly overhead athletes and laborers that perform a preponderance of their activities above the shoulder. These individuals are usually young, well developed, and complain of a diffuse ache around the posterior shoulder region. Their pain is more localized to approximately 4 cm medial to the posterolateral corner of the acromion as well as near the posterior aspect of the glenohumeral joint.
A patient may complain of weakness on attempts of external rotation and abduction which may confuse the examiner since no different than compression at the transverse scapular ligament, the patient with rotator cuff disease or even cervical disc disease may present in a similar fashion. However, patients with compression of the suprascapular nerve at the spinoglenoid ligament usually have more profound weakness on external rotation and a longer, protracted, chronic history, often the result of a missed diagnosis.
There are other unique possibilities that can result in suprascapular nerve compression. Forced, sudden humeral internal rotation, as seen in many racquet sports, can produce a stretch on the suprascapular nerve at the bony notch compression point, irrespective of the ligament dimensions. In such a scenario, activities across the body are often difficult, and the motion of a follow-through, whether throwing a baseball or spiking a volleyball, can be quite painful leading the athlete to avoid those movements. The position of follow-through or adduction in an extended position has been shown by our group to increase the tension and pressure within the spinoglenoid notch [3]. Common sports encompassing this motion include golf, volleyball, basketball, tennis, weight lifting, and swimming.
While sports activities may lead to suprascapular neuropathy, the heavy laborer may be plagued with this affliction as well because of all the repetitive overhead work duties they may perform, no different than those laborers with compression of the suprascapular nerve at the transverse scapular ligament. Compression at the spinoglenoid ligament is often insidious in onset, and a delay in diagnosis is the single biggest impediment to full restoration of muscle strength, alleviation of pain, and reversal of atrophy.
As stated previously, the suprascapular nerve at the spinoglenoid notch may be compressed by a ganglion cyst because the nerve is relatively immobile as it traverses the lateral edge of the scapular spine and is in close proximity of the posterior glenohumeral joint. Diagnosis by history can be difficult because the findings overlap considerably with rotator cuff and labral pathology. Certain findings though will help the clinician discern the diagnosis. One example is weakness on external rotation. The patient may complain that their infraspinatus fossa appears different in comparison to the opposite side. Often the chronic posterior ache or pain will increase and may even become constant and interrupt sleeping. Spinoglenoid compression, rather than compression at the transverse scapular ligament, is more commonly associated with complaints of catching, locking, or clicking because of the frequent association of a labral tear. As a final consideration, increased sports participation by females has caused the incidence of compression of the suprascapular nerve at the spinoglenoid ligament to have no appreciable gender bias.
Physical Examination
Clinical examination often has nonspecific findings in the early stages of this disease process. Symptoms are often less severe with suprascapular neuropathy at the spinoglenoid notch as opposed to more proximal compression. Some athletes present with isolated painless wasting of the infraspinatus. Surprisingly, palpation at the spinoglenoid notch can be very painful. Some patients may describe micro-instability as a part of their complaints although confirmatory physical findings will not be found.
Completion of a cervical spine examination and a standard exam of both shoulders with a full neurological assessment must be completed. The patient, when placed in a shoulder gown with the complete scapula in full view, may demonstrate subtle or severe atrophy to the infraspinatus fossa (Fig. 23.9). Atrophy though in a well-developed individual who participates in a weight-training program may at times be difficult to discern due to the overlying trapezius and large bulk of the deltoid muscle.


Fig. 23.9
Clinical photo and posterior view of the right shoulder demonstrating severe atrophy in a 21-year-old female tennis player with chronic wasting of the infraspinatus since age 9 with no apparent diagnosis (Copyright Kevin D. Plancher MD 2015)
Range of motion and strength must be assessed. There may be only a subtle loss of external rotation as well as abduction strength in young, overhead athletes. Strength of external rotation should be tested with the arm at the side, and weakness will often be present without any significant pain. The painless strength deficit is due to the fact that the sensory portion of the suprascapular nerve may be unaffected at the spinoglenoid notch. We have found that in long-standing disease, the teres minor and serratus anterior muscle may hypertrophy as compensation for the loss of the infraspinatus, hiding any strength deficit.
Provocative tests for labral pathology must be performed as labral tears with associated paralabral cysts may be found in conjunction with a suprascapular neuropathy at the spinoglenoid ligament.
A cross-arm adduction test, as described above, must be performed and recorded and correlated with a Zanca view X-ray in order to rule out acromioclavicular (AC) joint arthritis (Fig. 23.10a, b). If cross-body adduction reproduces the patient’s symptoms with the arm extended or internally rotated and the pain is primarily felt in the posterior aspect of the shoulder but the X-ray is negative, then the diagnosis of AC joint arthritis can be ruled out with an injection of lidocaine. A diagnosis of suprascapular nerve entrapment can now be claimed [21].
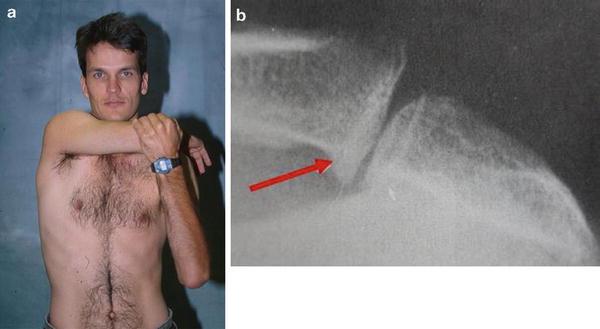
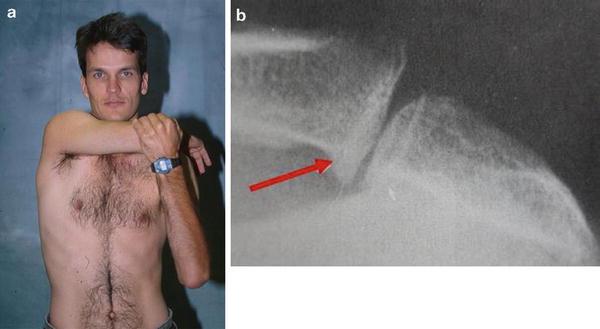
Fig. 23.10
(a) Clinical photo of the cross-arm adduction test. (b) Zanca view of a left shoulder showing classical osteoarthritis of the acromioclavicular joint with an osteophyte which would preclude a diagnosis of suprascapular nerve entrapment (Copyright Kevin D. Plancher MD 2015)
The differential diagnosis for suprascapular neuropathy at the spinoglenoid notch includes the same conditions considered for compression of the nerve at the transverse scapular ligament, i.e., cervical disc disease, a brachial neuritis, Parsonage–Turner syndrome, rotator cuff tendinopathy, labral pathology with or without a ganglion cyst, mild adhesive capsulitis, osteoarthritis of the glenohumeral joint, subacromial bursitis with or without impingement syndrome, AC degeneration disease, posterior glenohumeral instability, quadrilateral space syndrome, triangular space and interval disease or thoracic outlet syndrome, and the rare Pancoast tumor. The astute clinician recognizes that the lack of reproducible signs on physical exam for other common diagnoses and the overlapping symptoms with other shoulder problems often leads to a correct diagnosis.
Radiographic Examination
Plain radiographs including an anteroposterior (AP), axillary lateral, and the Y or supraspinatus outlet view should always be obtained (Fig. 23.11a–c). Special views such as a Stryker notch view can be ordered when necessary [5]. This plain series will identify any fracture or significant trauma to the scapula, clavicle, coracoid, or glenoid neck.
Fig. 23.11
(a) Artwork demonstrating the difference and correct way to obtain a true versus routine anteroposterior (AP) view of the shoulder. (b) Supine axillary view artwork demonstrated. (c) Artwork demonstrating the direction of the X-ray beam to obtain an X-ray of the acromioclavicular joint with a Zanca view (Copyright Kevin D. Plancher MD 2015)
Magnetic resonance imaging (MRI) and identification of soft tissue masses such as a ganglion cyst are critically important when evaluating compression of the suprascapular nerve at the spinoglenoid ligament (Fig. 23.12). The MRI can identify a true ganglion with a homogenous signal, low T1 intensity, with high T2 intensity and rim enhancement if contrast is utilized [22]. The MRI will also detect labral tears arising from the posterosuperior quadrant of the glenoid with the ganglion cyst attached (Fig. 23.13). Controversy exists as to whether the cyst truly arises from associated labral tears. Those that believe that this is the case insist on treatment to the labrum to minimize recurrence, while others advocate leaving the labrum alone after the cyst has been excised or decompressed.
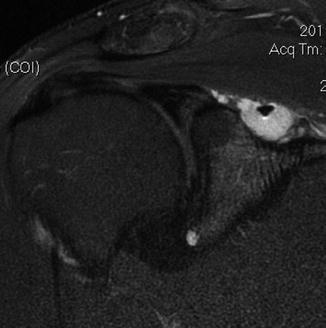

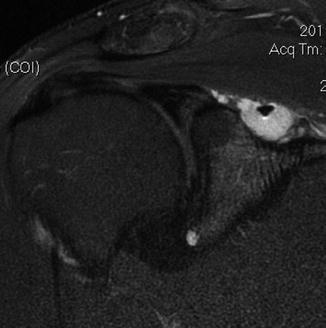
Fig. 23.12
MRI coronal view demonstrating ganglion cyst displacing the suprascapular nerve at the spinoglenoid notch (Copyright Kevin D. Plancher MD 2015)

Fig. 23.13
MRI axial view demonstrating labral tear as well as ganglion cyst compressing the suprascapular nerve at the spinoglenoid notch (Copyright Kevin D. Plancher MD 2015)
The presence of a soft tissue mass or ganglion cyst on MRI does not necessarily indicate suprascapular neuropathy. However, abnormal signal intensity within the infraspinatus muscle will indicate significant suprascapular nerve compression at the spinoglenoid notch. Some patients will demonstrate increased signal intensity on T2 fast spin echo with fat saturation with a normal muscle mass implying subacute denervation of the muscle leading to neurogenic edema. Chronic denervation, seen best on T1 spin echo with increased signal intensity within the muscle mass, will demonstrate muscle atrophy with fatty infiltration (Fig. 23.14).
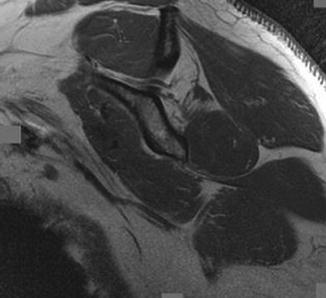
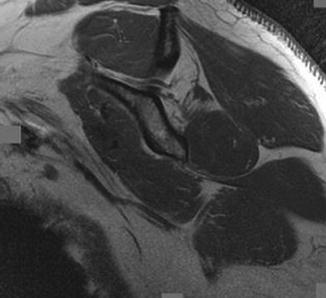
Fig. 23.14
Oblique MRI demonstrating isolated infraspinatus atrophy in this volleyball player. Note the course of the nerve in this T2-weighted image (Copyright Kevin D. Plancher MD 2015)
Newer modalities such as ultrasound may be helpful as well to identify ganglion cysts. This operator-dependent test can be very helpful not only in making a diagnosis but in assisting surgeons to complete an ultrasound-guided aspiration of the ganglion cyst. Compression sites can be readily visualized and aid in making a definitive diagnosis.
Selective Injections
A 1 % lidocaine anesthetic injection may be placed into the spinoglenoid notch to confirm the diagnosis of suprascapular nerve entrapment (Fig. 23.15). The needle is placed 4 cm medial to the posterolateral corner of the acromion. The patient is then asked if there is any change in the chronic ache that may have been present prior to injection. A cross-arm adduction test is then performed, and, if preinjection symptoms dissipate, the test is considered positive.


Fig. 23.15
Clinical photo of a lidocaine injection to be placed at the spinoglenoid ligament, 4 cm medial to the posterolateral corner of the acromion (Copyright Kevin D. Plancher MD 2015)
We have found pain relief to be dramatic and almost immediate with properly placed injections. Ultrasound may be used as an adjunct to guide the needle to ensure accuracy. This injection technique is simple; one feels the spine of the scapula and drops inferior to it by 1–2 cm and then, while aspirating, easily falls into the spinoglenoid notch. A negative injection test in conjunction with the absence of atrophy, a negative EMG, no evidence of a labral tear or ganglion cyst, yet weakness and pain, mandates at least a 6-month course of nonoperative treatment before considering any type of operative intervention.
Electrodiagnostic Testing
Electrodiagnostic testing replete with electromyography (EMG) and nerve conduction studies can help to confirm compression of the suprascapular nerve at the spinoglenoid notch. When the suprascapular nerve is compressed by a ganglion cyst or soft tissue mass at the spinoglenoid notch, the nerve will show decreased innervation of the infraspinatus muscle with normal innervation of the supraspinatus muscle. The stimulation point is typically performed at Erb’s point. Motor distal latency and motor response amplitude at the supraspinatus and infraspinatus muscles are measured. An increased latency beyond 3.3 ms (range 2.4–4.2 ms) is considered definitive for compression to the infraspinatus [23].
A classic positive electrodiagnostic study that detects compression at the spinoglenoid notch will demonstrate a dramatic motor loss to the infraspinatus if atrophy is present without changes in the supraspinatus muscle. Patients without visible atrophy present may still have compression of the nerve to the infraspinatus and hopefully on EMG will demonstrate a delayed terminal latency to the inferior branch of the suprascapular nerve. Side-to-side electrodiagnostic measurement differences are important [24]. Evaluation of the sensory velocities is less useful as the sensory innervation of this nerve is not as well defined.
Some investigators report that the only early finding may be increased nerve conduction time of the suprascapular nerve. This positive finding will allow the physician to discern that the neural compression is not in the cervical spine but rather located distally. This finding will enable the clinician to identify the compression point with selective injections and hopefully avoid irreversible damage to the suprascapular nerve. Decreases in the amplitude and spontaneous or marked polyphasicity of the evoked potentials are significant findings in confirming the presence of suprascapular entrapment at either the transverse scapular ligament or spinoglenoid ligament [5].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








