Distal Radius Fractures: Open Reduction Internal Fixation
George S.M. Dyer
Jesse B. Jupiter
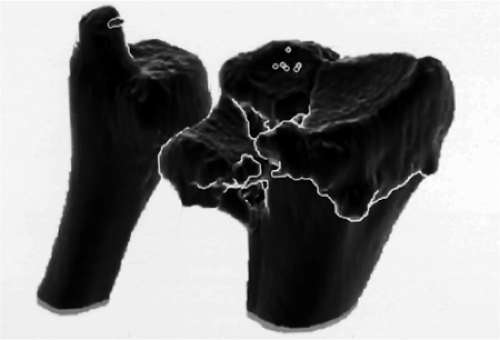
The past decade has witnessed widespread enthusiasm for operative treatment of distal radial fractures (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17). A number of factors have contributed to this changing perspective. Among these include a greater recognition of the wide variation in fracture patterns (18,19,20). The availability of computed tomography (CT) has permitted a three-dimensional projection of the fracture morphology (Fig. 13.1) (5,21). In fact, distal radial fractures differ to the extent that only the distal nature of the injury is in common among them (Fig. 13.2). Fractures that involve a shearing mechanism displacing part of the articular surface along with the carpus (Barton’s and reverse Barton’s fracture) (22,23,24,25), radiocarpal fracture-dislocations, displaced articular fractures associated with high-energy trauma and metaphyseal-diaphyseal comminution, articular compression fractures involving rotation of a volar lunate facet component, and some unstable extra-articular fractures are all amenable to open reduction and internal fixation.
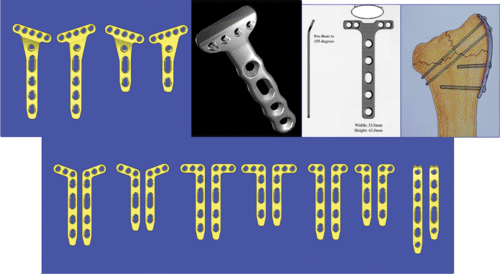
Along with a greater understanding of the variety of fracture patterns has been an expanded appreciation for the structural anatomy of the distal radius. Rikli and Regazzoni (26) divided the distal radius into a strong, cortical radial “column”; an intermediate column, which contains the articular surfaces of both the lunate facet as well as the sigmoid notch; and the distal ulna column with its firm attachment to the radius through the triangular fibrocartilage complex (Fig 13.3). Recognition of this unique anatomical orientation and patterns of articular injury has led to the development of a method of operative treatment coined “fragment-specific fixation,” through which small strategically-placed implants are used to support the critical structural components of the fracture (Fig. 13.4).
A third factor that has led to the operative treatment of certain fractures involves those injuries associated with intercarpal injury (27,28). Fracture patterns involving compression or shearing of the radial styloid and/or scaphoid facet of the distal radius are recognized to have the potential of accompanying injuries to the scapholunate ligament as well as the lunate facet and the lunotriquetral ligament (Fig 13.5).
Associated instability of the distal radioulnar joint (DRUJ) has also stimulated more operative intervention. DRUJ instability following stabilization of the radius fracture,
especially in the presence of a large ulnar-styloid fracture, is best treated by operative fixation of the ulnar styloid.
especially in the presence of a large ulnar-styloid fracture, is best treated by operative fixation of the ulnar styloid.
Interest in operative intervention has been further generated by the development of a variety of technologically advanced implants that are specific to the distal radius. These new pieces have features, such as locking screws that enhance fixation in osteopenic bone, that have led to interest in the volar approach to internal fixation of dorsally displaced fractures. A volar approach would limit the potential for problems involving the overlying extensor tendons on the dorsal surface.
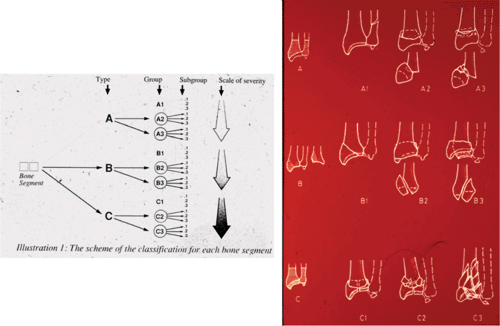 Figure 13.2. The comprehensive classification of the AO/ASIF demonstrates three major types, nine groups, and twenty-seven subgroups reflecting the enormous variation of fracture patterns. |
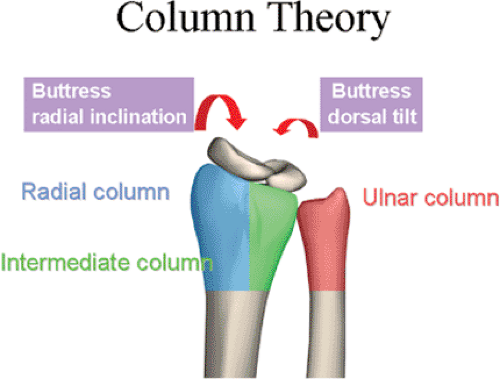 Figure 13.3. The column concept, developed by Rikli and Regazzoni (26), includes the radial, intermediate, and ulnar columns. |
 Figure 13.5. Fractures involving compression or shearing of the articular surface may be accompanied by intercarpal ligament injury. |
Table 13.1. Definite Indications for Open Reduction and Internal Fixation | |
|---|---|
|
Indications/Contraindications
A number of factors are considered when surgeons decide on operative fixation of distal radius fractures: specific aspects of the fracture itself, the presence of associated soft-tissue injury such as median nerve dysfunction; associated ipsilateral limb injury, and the overall physical and medical condition of the patient. With the advent of fixed-angle locking screw-plate constructs, underlying osteopenia is no longer a contraindication to internal fixation.
Definite Indications for ORIF
Fracture patterns including volar or dorsal radiocarpal subluxations or dislocations, displaced radial-styloid fractures, articular fractures involving a displaced and rotated volar lunate-facet component, and those displaced fractures presented 3 weeks after the injury (Table 13.1).
Relative Indications
Relative indications for ORIF include a host of different fractures. These include bilateral displaced fractures, fractures associated with ipsilateral limb trauma, some fractures with associated progressive swelling or nerve dysfunction, open fractures, fractures associated with DRUJ instability, or unstable extra or intra-articular fractures that were not reduced after closed reduction and cast immobilization (Table 13.2).
Relative Contraindications
Patients with medical conditions that prohibit the use of anesthesia, with poor compliance, or with local soft-tissue conditions, such as active infection or complex regional pain syndrome, may not benefit from internal fixation for their fracture (Table 13.3).
Preoperative Planning
As with any musculoskeletal injury, a careful evaluation of the patient’s overall condition, as well as that of the involved limb and hand, must be made before a decision is rendered to proceed with operative intervention. The fracture characteristics are not always easily appreciated before the fracture is reduced and repeat x-rays are taken. Furthermore,
additional x-ray views, including oblique views to focus on the articular surface, or CT studies may further influence the decision about intervening operatively.
additional x-ray views, including oblique views to focus on the articular surface, or CT studies may further influence the decision about intervening operatively.
Table 13.2. Relative Indications for ORIF |
|---|