Musculoskeletal injuries are the second most common cause of presentation to emergency departments. Distal radius fractures are an especially common injury pattern that often require evaluation and fracture management in an emergency department. This article reviews the evaluation of distal radius fractures including physical examination and radiographic review. Also discussed is management of distal radius fractures including splinting in the setting of an emergency department consultation.
Key points
- •
Diagnosis of a distal radius fracture can be made readily with plain radiographs and does not routinely require advanced imaging with computed tomography or MRI.
- •
Findings that may warrant urgent surgical management include an open fracture, vascular injury, or acute carpal tunnel syndrome.
- •
Indications for emergency department reduction include significant deformity, joint dislocation or subluxation, and radiographic parameters that include more than 20 degrees of dorsal tilt.
- •
On reduction, casting should be avoided and ace compression wrapping over the splint should be applied loosely allowing for early and free finger motion.
- •
Outpatient surgical indications are based on a variety of factors including patient demographics, age, concomitant injuries, fracture alignment, and fracture stability.
Introduction
Musculoskeletal injuries, such as distal radius fractures of the wrist, are a common presentation to an emergency department (ED). In the United States, these injuries are second only to respiratory illnesses in frequency of ED visits, accounting for 20% of chief complaints. However, despite the frequency of presentation, education in musculoskeletal injuries is often considered deficient in medical education. The volume of orthopedic presentations to an ED prompted further study of musculoskeletal education in emergency medicine training. Comer and colleagues provided a validated 25-question orthopedic examination published in 1998 by Freedman and Bernstein to emergency medicine residents and attendings at all levels of training. The results found a 61% overall passing rate (65% for residents and 57% for attendings). As a result of the frequency of musculoskeletal injuries, it is important for all practitioners who evaluate or treat patients in the ED to be well-educated in these injuries.
Distal radius fractures are the most common upper extremity fracture affecting all patient populations, but are particularly prevalent in the young and elderly. Among patients older than 65 years of age, distal radius fractures account for 18% of all fractures. This injury is seen by orthopedic surgeons with an incidence of 195.2 per 100,000 patients per year. The active elderly are disproportionately affected because the common mechanism of the fracture is a standing level fall onto an outstretched hand. The health burden of this injury pattern is substantial because there were 640,000 reported distal radius fractures in the United States in 2001. There is also a significant economic burden because distal radius fractures contribute significantly to the approximate $1.1 billion cost of osteoporotic fractures in the Medicare population. Furthermore, the incidence of this injury pattern has been on the rise in the United States and internationally, with a disproportionate increase in patients 65 years and older. As life expectancy continues to rise and people remain active later in life, distal radius fractures will be an increasingly significant clinical problem.
This article provides an evidence-based guide of early management of distal radius fractures. This is intended for practitioners who would treat this injury in an ED. We discuss the typical presentation of distal radius fractures, radiographic findings, and early management strategies, and focus on what emergent situations require immediate orthopedic intervention.
Introduction
Musculoskeletal injuries, such as distal radius fractures of the wrist, are a common presentation to an emergency department (ED). In the United States, these injuries are second only to respiratory illnesses in frequency of ED visits, accounting for 20% of chief complaints. However, despite the frequency of presentation, education in musculoskeletal injuries is often considered deficient in medical education. The volume of orthopedic presentations to an ED prompted further study of musculoskeletal education in emergency medicine training. Comer and colleagues provided a validated 25-question orthopedic examination published in 1998 by Freedman and Bernstein to emergency medicine residents and attendings at all levels of training. The results found a 61% overall passing rate (65% for residents and 57% for attendings). As a result of the frequency of musculoskeletal injuries, it is important for all practitioners who evaluate or treat patients in the ED to be well-educated in these injuries.
Distal radius fractures are the most common upper extremity fracture affecting all patient populations, but are particularly prevalent in the young and elderly. Among patients older than 65 years of age, distal radius fractures account for 18% of all fractures. This injury is seen by orthopedic surgeons with an incidence of 195.2 per 100,000 patients per year. The active elderly are disproportionately affected because the common mechanism of the fracture is a standing level fall onto an outstretched hand. The health burden of this injury pattern is substantial because there were 640,000 reported distal radius fractures in the United States in 2001. There is also a significant economic burden because distal radius fractures contribute significantly to the approximate $1.1 billion cost of osteoporotic fractures in the Medicare population. Furthermore, the incidence of this injury pattern has been on the rise in the United States and internationally, with a disproportionate increase in patients 65 years and older. As life expectancy continues to rise and people remain active later in life, distal radius fractures will be an increasingly significant clinical problem.
This article provides an evidence-based guide of early management of distal radius fractures. This is intended for practitioners who would treat this injury in an ED. We discuss the typical presentation of distal radius fractures, radiographic findings, and early management strategies, and focus on what emergent situations require immediate orthopedic intervention.
History and physical examination
When assessing the patient who sustains a wrist injury, history and physical examination are an important diagnostic tool. The classic presentation of distal radius fractures is the elderly female with a fall onto an outstretched hand. However, unlike these relatively low-energy injuries that typically occur from falling from a standing level, higher-energy injuries can also result in distal radius fractures with a higher prevalence in younger populations. A full trauma assessment of these patients is often necessary because the wrist fracture may not be an isolated injury.
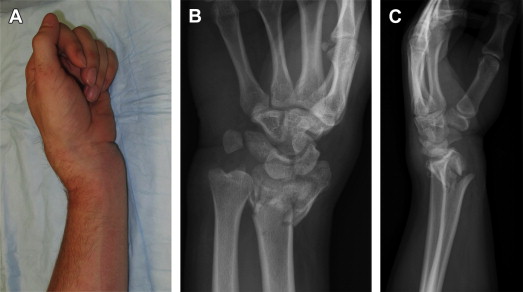
The first step in physical examination is assessment for any obvious deformity. Most displaced fractures present with a wrist that is swollen and potentially deformed and angulated ( Fig. 1 ). Concurrently, the skin and soft tissue should be examined for any defects that could generate concern for an open fracture ( Fig. 2 ). Patients with an open fracture should also be treated with tetanus prophylaxis (based on patient’s immunization status) and intravenous antibiotics immediately.
Vascular examination is the next component of the examination. The hand and wrist is well perfused with robust vascular anatomy. Capillary refill of the finger tips is a common technique used to evaluate blood flow of the hand but has low sensitivity in confirming perfusion. Moreover, it is commonly delayed because of swelling and deformity, but radial and ulnar pulses should be palpable. If pulses are not palpable, the deformity can be improved and the vascular examination can be repeated. Alternatively, consider using a Doppler ultrasound. If pulses are still not present and/or if there is concern for a vascular injury, such as ischemic changes to the hand, rapidly enlarging hematoma, or the presence of arterial bleeding, consider emergent evaluation by an orthopedic surgeon or a vascular surgeon.
Neurologic examination is often difficult to assess in the setting of an acute fracture because of pain. Moreover, patient discrimination between subjective pain, numbness, and paresthesia may be highly variable. Nonetheless, a thorough examination of the hand with careful assessment of sensory and motor function of the radial, median, and ulnar nerves is critical. The radial nerve can be tested for sensation on the dorsal aspect of the first webspace of the hand, whereas motor function is assessed by thumb and finger extension testing. Sensation in the ulnar nerve can be tested on the palmar aspect of the small finger and motor innervation is tested by assessing finger abduction. Sensation in the median nerve can be tested on the palmar aspect of the index finger ( Fig. 3 A ) and motor innervation is tested by assessing thumb abduction, specifically the abductor pollicis brevis (see Fig. 3 B). Although neurologic examination may be limited secondary to pain and swelling, the median nerve is at particular risk of injury with a displaced distal radius fracture and its dysfunction must be readily recognized ( Fig. 4 ). Median nerve dysfunction may be a result of nerve contusion or acute carpal tunnel syndrome. Median nerve contusion is a nonemergent condition consisting of nonprogressive numbness in the sensory distribution of the median nerve. Conversely, patients with an acute carpal tunnel syndrome present with a rapidly progressive median neuropathy with worsening painful parasthesias in its sensory distribution. This acute compressive neuropathy results from immediate postinjury swelling in the carpal tunnel and is an emergent situation that requires immediate surgical decompression of the median nerve in the carpal tunnel and fracture reduction.
Radiographic analysis
Plain radiographs are the mainstay of diagnosis of distal radius fractures. Standard posteroanterior, lateral, and oblique radiographs are typically sufficient (see Fig. 1 ). There are several radiographic parameters that are important to analyze in distal radius fractures. Variations from these normal parameters may confirm the presence of a fracture. Furthermore, the extent of variation from these parameters can dictate surgical or nonsurgical management of distal radius fractures. These parameters are radial inclination, radial length, volar tilt, ulnar variance, and the scapholunate angle ( Fig. 5 ). The normal values for these measurements are approximately 23 degrees for radial inclination, 12 mm for radial length, 10 degrees for volar tilt, and −0.6 mm for ulnar variance. Common concomitant injuries to the wrist should also be considered when evaluating radiographs for a possible distal radius fracture, and include other carpal fractures, such as of the scaphoid, distal ulna fractures, disruption of the distal radioulnar and radiocarpal joints, and intercarpal ligament injuries, such as a scapholunate ligament tears or perilunate dislocations ( Fig. 6 ).
Advanced imaging is typically not indicated in the acute setting. However, computed tomography scan may be used for preoperative planning of comminuted fractures with articular involvement. MRI can be useful to assess for additional internal derangement of the wrist, such as a suspected concomitant ligamentous injury.
Open fracture management
An open fracture of the distal radius should be initially managed as any other open fracture in the ED setting. The patient should be provided with tetanus prophylaxis, receiving either a tetanus toxoid booster or a combination of the booster with human tetanus immunoglobulin, depending on the patient’s tetanus prophylaxis history.
Early administration of antibiotics is critical because open fractures are by definition contaminated. Appropriate antibiotics should ideally be administered within 3 hours of the injury to lower infection rate. Specific antibiotic therapy depends on the extent of soft tissue injury, which is commonly classified with the Gustilo-Anderson system. Gustilo I fractures require cefazolin every 8 hours for three doses, Gustilo II fractures require cefazolin and tobramycin or piperacillin/tazobactam for 24 hours after wound closure, and Gustilo III fractures require cefazolin and tobramycin or piperacillin/tazobactam with the addition of intravenous penicillin if the wound is contaminated with soil (anaerobic coverage) for a minimum of 3 days after wound closure ( Table 1 ).
| Classification | Criteria | Description | Antibiotics a |
|---|---|---|---|
| Gustilo I | Wound <1 cm No contamination Simple fracture No periosteal stripping | Local skin coverage No neurovascular injury Low energy No soft tissue damage | First-generation cephalosporin for 24 h after closure |
| Gustilo II | Wound >1 cm Moderate contamination Moderate comminution No periosteal stripping | Local skin coverage No neurovascular injury Moderate energy No extensive soft tissue damage | First-generation cephalosporin for 24 h after closure |
| Gustilo III | |||
| IIIA | Large injury zone Extensive contamination Severe comminution or segmental fracture Periosteal stripping | Local skin coverage No neurovascular injury High energy Extensive soft tissue damage | First-generation cephalosporin and aminoglycoside (gram-negative) for 24–72 h after debridement |
| IIIB | Large injury zone Extensive contamination Severe comminution or segmental fracture Periosteal stripping | Requires soft tissue coverage (flap) No neurovascular injury High energy Extensive soft tissue damage | First-generation cephalosporin and aminoglycoside (gram-negative) for 24–72 h after debridement |
| IIIC | Large injury zone Extensive contamination Severe comminution or segmental fracture Periosteal stripping | Local skin coverage Neurovascular injury requiring arterial repair High energy Extensive soft tissue damage | First-generation cephalosporin and aminoglycoside (gram-negative) for 24–72 h after debridement |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





