Fractures
Sarah Pettrone
Douglas P. Hanel
Sterile Instruments/Equipment
- Finger traps
- Sterile rope for on-table traction
- Small pointed reduction clamps (“Weber” clamps)
- Implants
- External fixator if necessary
- Small fragment plates and screws, locking or nonlocking (distal radius-specific helpful but not essential)
- Mini-fragment screws for free fragments
- Wrist fusion plate, 3.5-mm locking plates, or custom locking plate made specifically for spanning technique
- External fixator if necessary
- K-wires and wire driver/drill
Positioning
- Supine on a radiolucent hand table.
- Bring the patient to the lateral edge of the bed.
- Center the shoulder/elbow/hand on the hand table, with the shoulder abducted 90 degrees.
- Place a pneumatic tourniquet on the ipsilateral arm, if desired.
- A sterile traction device may be applied after draping (Fig. 9-1).
Figure 9-1. A sterile traction device for reduction assistance. Two “overhand” knots are tied at the ends of a 3 ft (100-cm) rope. One end is attached to finger traps, and 10 lb of weight is hung from the loop of the rope at the other end.
Reduction and Fixation Techniques
- Typical reduction maneuvers (described by Agee).
- Longitudinal traction to restore length.
- Palmar translation of the hand-carpus, relative to the forearm, restores palmar tilt and demonstrates volar instability, when present.
- Slight pronation of the hand relative to the forearm, combined with ulnar deviation, corrects the supination deformity of a great majority of distal radius fractures.
- Longitudinal traction to restore length.
- After reduction maneuvers, repeat fluoroscopic fracture assessment (AP, lateral, and oblique).
- Determine the fracture involvement of the three columns of the wrist (Rikli and Regazzoni).
- Medial—ulnar head.
- Intermediate—sigmoid notch, volar, and dorsal ulnar lunate fossa, lunate fossa dye-punch.
- Lateral—volar and dorsal scaphoid fossa, and radial styloid.
- Assess metaphyseal comminution.
- Medial—ulnar head.
- Determine the overall fracture stability.
- Stable fractures are generally defined prior to reduction.
- No articular step off or gap >2 mm
- No metaphyseal comminution >1/3 of AP width (on lateral projection)
- No involvement of the volar medial corner (Critical Corner)
- Stable distal radial ulnar joint (DRUJ)
- No articular step off or gap >2 mm
- All other fractures are considered unstable and are indicated for operative fixation.
- Also, consider whether there is adequate bone quality to allow pin implant purchase.
- Stable fractures are generally defined prior to reduction.
- Treatment of stable fractures.
- Cast or splint immobilization
- If fracture reduction tenuous, then long arm with forearm in supination, otherwise short arm.
- Wrist in neutral or slightly extended position.
- Check X-rays weekly for a minimum of 3 weeks.
- Compare the most recent X-ray with the immediate postreduction film.
- Comparing X-rays from one week to the next can result in failing to recognize gradual loss of reduction. Follow up X-rays must be compared to the initial reduction films.
- If reduction becomes unacceptable, then proceed to re-reduction and fixation.
- If fracture reduction tenuous, then long arm with forearm in supination, otherwise short arm.
- Cast or splint immobilization
- Three basic types of fixation for unstable fractures.
- Closed manipulation with percutaneous fixation, with or without external fixation.
- Open reduction with large plates for large fragments.
- Open reduction with fragment-specific implants, also referred to as “column specific” or “fragment specific.”
- Closed manipulation with percutaneous fixation, with or without external fixation.
- Closed techniques.
- Percutaneous K-wire (interfocal through fracture fragments)
- 1.5 mm or 0.062 inch
- At least two pins, one in the radial column and the other in the dorsal aspect of the intermediate column (either through Lister’s tubercle or between fourth and fifth dorsal compartments)
- 1.5 mm or 0.062 inch
- Percutaneous K-wire (intrafocal through fracture site)
- The Kapandji technique of intrafocal pinning involves placement of biplanar K-wires.
- Introduce a coronal plane K-wire into the fracture site in a radial to ulnar direction on the AP radiographic view.
- A second sagittal plane K-wire is placed into the fracture site in a dorsal to volar direction.
- Once in the fracture site, the wires are used as a lever to elevate the distal fragments, restoring the radial inclination, length and volar tilt.
- The wires are then driven into the opposite cortex of the radius.
- Supplemental K-wires may be inserted to secure the fracture reduction and improve the fixation stiffness (Fig. 9-2).
- The wires are then driven into the opposite cortex of the radius.
- Introduce a coronal plane K-wire into the fracture site in a radial to ulnar direction on the AP radiographic view.
- The Kapandji technique of intrafocal pinning involves placement of biplanar K-wires.
- Percutaneous K-wire (interfocal through fracture fragments)
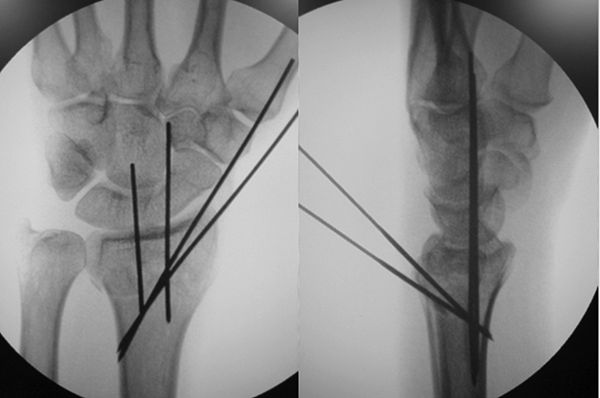
Figure 9-2. AP and lateral radiographs demonstrating the combined intrafocal and interfocal percutaneous pinning. Two pins were placed using the Kapandji technique to restore the volar tilt. Two additional percutaneous pins were placed in the radial styloid.
![]()
- Supplemental fixation (external fixation) is often required in older patients or in those with poor bone quality.
- Wrist joint spanning external fixation
- Bridging external fixation may be used as a temporizing measure or as a definitive fixation for distal radius fractures.
- Indicated for severe open fractures with soft tissue defects, as a temporizing measure in a polytrauma patient, unstable extraarticular fractures, and non-displaced intra-articular fractures.
- Spanning external fixation may be combined with internal fixation techniques to maintain length and added stability with internal fixation.
- Contraindicated as isolated fixation of displaced intra-articular fractures, unless those fractures are irreparable and serves as a preamble to fusion.
- The reduction maneuver described by Agee is performed (described above).
- Pin placement.
- Exposure to bone and soft protection is required.
- Most fixator systems have a drill guide to ensure placement of parallel, bicortical pins spaced 3 to 5 cm apart.
- Free hand systems also work well, although less convenient.
- Forearm pins are placed in the bare area of the radius just proximal to the muscle bellies of the abductor pollicus longus (AbPL) and extensor pollicus brevis (EPB).
- This is approximately 10 to 12 cm proximal to the radial styloid.
- A 3 to 5 cm dorsal radial incision is made just proximal to the EPB and AbPL.
- Using the interval between the extensor carpi radialis longus (ECRL) and the extensor carpi radialis brevis (ECRB), the superficial radial nerve is protected.
- The interval between the ECRL and BR can also be used but has an increased risk of injury to the superficial branch of the radial nerve.
- This is approximately 10 to 12 cm proximal to the radial styloid.
- Hand (distal) pins are placed in the second metacarpal, parallel to the proximal pins.
- The more proximal pin is placed through the metaphysis of the second metacarpal.
- If this pin does not have adequate purchase, advance it through a third cortex into the third metacarpal.
- The more distal pin is placed in the diaphysis of the second metacarpal.
- The more proximal pin is placed through the metaphysis of the second metacarpal.
- Exposure to bone and soft protection is required.
- Fracture length and wrist alignment are restored with traction and fixator clamps, and bars are applied.
- After the fixator is applied, examine the midcarpal and radiocarpal joints to be sure that the extremity is not overdistracted.
- The fingers should fully flex and extend without excessive tightness.
- Residual dorsal angulation is difficult to correct.
- But can be managed by palmar translation of the hand relative to the forearm, prior to tightening the clamps and bars.
- Increased traction often worsens the dorsal angulation.
- Supplemental K-wires used as joysticks may be necessary to achieve reduction.
- Increased traction often worsens the dorsal angulation.
- Intra-articular depression.
- Limited internal fixation may be necessary to reduce and maintain articular fragments (Fig. 9-3).
- Bridging external fixation may be used as a temporizing measure or as a definitive fixation for distal radius fractures.

Figure 9-3. Compression fracture involving all three columns, treated with closed reduction, percutaneous pin fixation, and external fixation. Final radiographs taken 2 years after injury demonstrated healing in accurate position.
![]()
- Nonspanning (joint sparing) external fixation
- Indicated for unstable extraarticular distal radius fractures.
- Contraindicated when the distal fragments are too small for pin placement.
- At least 1 cm of intact volar cortex is required for pin purchase.
- A small external fixation set is recommended with 2.5-mm threaded tip pins.
- A transverse incision is made over Lister’s tubercle, tendons adjacent to the tubercle are retracted.
- The dorsal cortex is predrilled and threaded tip pins introduced.
- The pins are placed slightly convergent in the sagittal (dorsal to palmar) plane.
- It is critical that the pins purchase the volar cortex.

Stay updated, free articles. Join our Telegram channel
- Indicated for unstable extraarticular distal radius fractures.

Full access? Get Clinical Tree