Distal Humerus Intra-articular Fractures: Open Reduction Internal Fixation
Gary L. Zohman
Indications/Contraindications
Intra-articular fractures of the distal humerus are uncommon injuries. Despite improved surgical techniques and implants, operative management does not guarantee an excellent clinical result. Indications for surgery include all displaced fractures in adults who are medically stable for surgery. Nonoperative management of displaced intra-articular fractures of the distal humerus are associated with unacceptably high rates of malunion, nonunion, and elbow joint stiffness, often leading to loss of independence and subsequent disability. The goal of surgery are identical to those of all intra-articular fractures: stable fixation to allow early joint motion in an anatomical position with healing of the fracture.
While early articular reconstruction is the treatment of choice for most fractures, some injuries in the osteoporotic elderly are probably best treated with primary elbow arthroplasty. Contraindications to surgery include selected grade-IIIB open fractures, active infection, extreme comminution such as found in gunshot wounds, lack of equipment, and surgeon inexperience.
Preoperative Planning
A thorough and meticulous examination of the upper extremity is performed. A detailed neurovascular examination as well as the status of the patient’s compartments are documented. In multiply injured patients, evaluation of the head, chest, abdomen, and spine are essential. In many patients, concomitant injuries take precedence over the distal humeral fracture(s).
Initial radiographs of the elbow and distal humerus invariably show the fracture. However, a complete understanding of the fracture is difficult secondary to collapse of
elbow anatomy caused by fracture displacement. In many cases, adequate radiographs may only be obtainable while patient is in traction and under intravenous sedation or anesthesia. Computed tomography (CT) is occasionally performed preoperatively. CT may reveal associated injuries of the radial head or neck that will alter the surgical plan. Coronal plane fractures of the anterior portion of the articular surface of the distal humerus are also identifiable by CT. As with plain radiographs, CT scans are most helpful when major fracture displacement has been corrected and the arm splinted. With the exception of open fractures, the vast majority of intra-articular fractures of the distal humerus are done semi-urgently.
elbow anatomy caused by fracture displacement. In many cases, adequate radiographs may only be obtainable while patient is in traction and under intravenous sedation or anesthesia. Computed tomography (CT) is occasionally performed preoperatively. CT may reveal associated injuries of the radial head or neck that will alter the surgical plan. Coronal plane fractures of the anterior portion of the articular surface of the distal humerus are also identifiable by CT. As with plain radiographs, CT scans are most helpful when major fracture displacement has been corrected and the arm splinted. With the exception of open fractures, the vast majority of intra-articular fractures of the distal humerus are done semi-urgently.
The AO/ASIF has shown that with complex peri-articular fractures, results can be improved with the creation of a surgical plan. This involves a written step-by-step surgical tactic outlining each step of the operation, including the placement of screws, plates, bone grafts, and so forth. The creation of a preoperative plan ensures that needed implants can be ordered and will be available. In addition, when a preoperative plan is utilized, surgery and tourniquet times can be reduced and the need for bone graft clarified.
Available implants for internal fixation should include small diameter screws (1.5 through 2.4 mm) for comminuted peri-articular fragments as well as 3.5-mm compression and reconstruction plates and screws. Peri-articular and/or locking plates can be extremely useful. In some patients, 3.5-mm screws directed from medial to lateral in the supra-articular region will exceed the 50-mm maximum length available in the standard, small fragment instrument tray. Therefore, supplemental screw lengths should be readily available along with an accompanying extra-long 2.5-mm drill bit.
Two, large, pointed, reduction tenacula are invaluable in the articular reconstruction. A medium, serrated, reduction clamp is helpful during medial plate application. In patients with extensive comminution, the iliac crest should be prepped and draped or bank bone graft should be available.
Surgery
Surgery is usually performed under general anesthesia, although regional anesthesia is occasionally employed. Prophylactic intravenous antibiotics are given before the procedure. Surgery can be done with the patient in the lateral or prone position. I prefer the lateral decubitus position. The arm is supported over a padded small-diameter post that will allow intraoperative flexion of the elbow to 110 degrees (Fig. 7.1). The entire upper extremity, flank, and iliac crest are prepped in the same field through the utilization of pairs of U-shaped split drapes. The arm is exsanguinated and a sterile tourniquet applied.
The tourniquet is later removed after the articular reconstruction is complete. A c-arm image intensifier must be available so fracture reduction and screw placement can be assessed.
The tourniquet is later removed after the articular reconstruction is complete. A c-arm image intensifier must be available so fracture reduction and screw placement can be assessed.
 Figure 7.1. The patient is placed in the lateral decubitus position with the arm draped over a padded roll; this position allows for intraoperative flexion of the ulna to 110 degrees. |
A posterior longitudinal incision is made beginning at the midpoint of the arm and extending over the dorsal surface of the ulna onto the proximal forearm. The incision is placed slightly medial or lateral to the tip of the olecranon (Fig. 7.2.). The ulnar nerve is identified and followed proximally to where it emerges from the medial intermuscular septum and distally to where it enters the flexor carpi ulnaris. The nerve is protected with a moistened Penrose drain (Fig. 7.3).
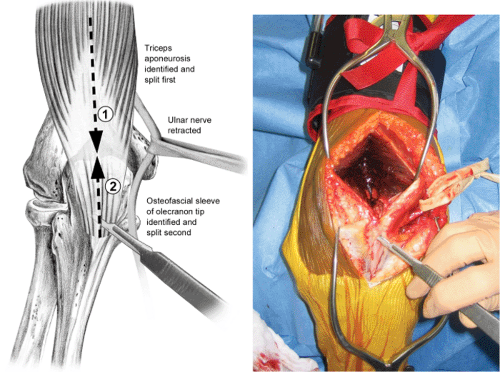
Exposure of the articular fracture fragments is done with either a formal olecranon osteotomy or a triceps slide. For most patients, I prefer a modified Morrey triceps-splitting approach; the split is extended longitudinally down the fascial sleeve of the proximal
forearm. This approach provides excellent access to the distal humerus and decreases some of the complications associated with an olecranon osteotomy. The extended triceps-splitting approach may be desirable when there is transverse disruption of the extensor mechanism (which often occurs in open fractures) and the distal humeral-shaft-fracture fragment protrudes posteriorly through the triceps tendon.
forearm. This approach provides excellent access to the distal humerus and decreases some of the complications associated with an olecranon osteotomy. The extended triceps-splitting approach may be desirable when there is transverse disruption of the extensor mechanism (which often occurs in open fractures) and the distal humeral-shaft-fracture fragment protrudes posteriorly through the triceps tendon.
 Figure 7.2. The anatomy is marked with ink pen on the skin. A longitudinal incision is made slightly lateral to the tip of the olecranon. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree