Distal Humerus Fractures
Joaquin Sanchez-Sotelo
INTRODUCTION
The management of distal humerus fractures has been improved over the last few years due to (a) more common use of advanced imaging modalities such as computed tomography (CT), (b) understanding the benefits of parallel-plating techniques, (c) the recognition of the more complex patterns of shear fractures of the articular surface of the distal humerus, (d) the widespread use of precontoured periarticular plates, and (e) the selective use of elbow arthroplasty. However, these injuries continue to lead to persistent pain and disability in a substantial number of patients due to the severity of the injury, suboptimal management, or complications such as ulnar neuropathy, wound complications, and heterotopic ossification.
INDICATIONS AND CONTRAINDICATIONS
Open reduction and internal fixation is the treatment of choice for most distal humerus fractures.
Nonoperative treatment is seldom appropriate or successful for these injuries, except for the very elderly, frail patient with absolute contraindications to anesthesia and surgery.
Elbow arthroplasty is indicated only in a selective group of elderly patients with either preexisting articular pathology (i.e., rheumatoid or posttraumatic arthritis) or low comminuted fractures with osteopenia or severe damage to the articular surface.
PREOPERATIVE PLANNING
The general principles of evaluation for musculoskeletal injuries apply to distal humerus fractures, including assessment of the soft tissues (especially in open fractures), the neurovascular status of the upper extremity, identification of associated injuries, and adequate imaging studies. It is important to understand whether there was preexisting elbow pathology as well as the anticipated physical demands on the elbow, especially when arthroplasty is being considered as an alternative to internal fixation.
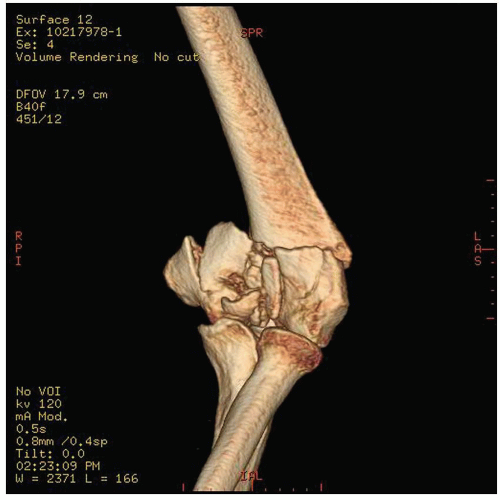
Anteroposterior and lateral radiographs of the elbow may be difficult to interpret because of fracture displacement and comminution (Fig. 8-1). Radiographs made with the upper extremity under traction are useful, but often cannot be obtained until the patient is under anesthesia and ready for surgery. Three-dimensional reconstructions rendered from a CT scan are extremely useful for understanding the fracture pattern and planning the internal fixation strategy (Fig. 8-2); in our institution, we obtain a CT with three-dimensional reconstruction prior to internal fixation routinely.
SURGICAL TECHNIQUE
Position
The patient is placed supine with the arm brought across the chest. Alternatively, the lateral decubitus position may be employed.
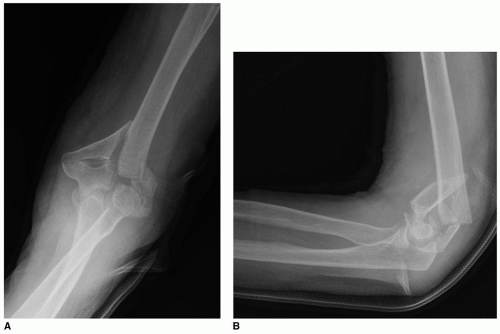 FIGURE 8-1 Anteroposterior (A) and lateral (B) radiographs show a displaced comminuted supraintercondylar fracture of the distal humerus. |
Exposure
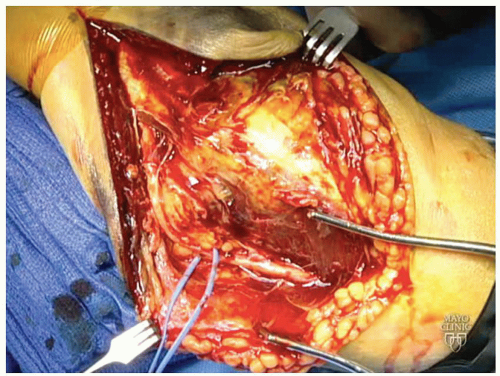
Fracture fixation is performed though a posterior midline skin incision slightly medial to the tip of the olecranon (Fig. 8-3). Controversy remains regarding the ideal management of the ulnar nerve at the time of fixation. We favor subcutaneous transposition in order to prevent contact of the nerve with the medial plate and protect the nerve during the procedure (Fig. 8-4). However, some recent
studies suggest a lower rate of postoperative neuropathy when the ulnar nerve is returned to its anatomic position at the end of the procedure.
studies suggest a lower rate of postoperative neuropathy when the ulnar nerve is returned to its anatomic position at the end of the procedure.
Deep Exposure Adequate exposure is critical for anatomic reduction of the articular surface as well as successful internal fixation. The best exposure for most fractures is through an olecranon osteotomy. We favor a chevron olecranon osteotomy aimed to the bare area of the articular surface of the proximal ulna (Fig. 8-5). The osteotomy is initiated with a saw and completed with an osteotome to create some irregularity and the osteotomy site, limit bone loss, and avoid inadvertent articular damage.
Simple fractures may occasionally be managed by exposing the distal humerus on both sides of the triceps; this approach is favored whenever possible. Alternatively, the extensor mechanism may be detached from its bony attachments using the Bryan-Morrey or triceps-reflecting anconeus pedicle approaches. These approaches are especially attractive when the decision to proceed with internal fixation or arthroplasty needs to be made intraoperatively, but exposure is more limited, and failure of triceps healing may lead to weakness in extension.
Internal Fixation Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree