Distal Humeral Osteotomy
Thomas Duquin
Scott P. Steinmann
INTRODUCTION
Osteotomy of the distal humerus is a relatively uncommon and technically demanding procedure. Elbow anatomy and function are a complex interaction of the ulnohumeral, radiocapitellar, and proximal radioulnar joints. A clear understanding of the bony and soft tissue anatomy, as well as elbow kinematics, is necessary for a successful outcome following distal humeral osteotomy. This knowledge must include both normal elbow anatomy as well as the patient’s pathology.
Elbow functional range of motion is a 100-degree arc of motion between 30 degrees of extension and 130 degrees of flexion. The normal carrying angle of the elbow is between 7 and 14 degrees of valgus, with females having slightly higher valgus angles than males. The epicondylar axis is parallel to the articular surface in the coronal plane, and the distal humeral articular surface has a 30-degree anterior angulation in the sagittal plane. The epicondylar axis of the distal humerus is 3 degrees internally rotated in relation to the articular surface. Stability of the elbow joint is a complex interaction of bony, ligamentous, and muscular stabilizing forces. The primary stabilizers of the joint are the ulnohumeral articulation, the lateral ulnar collateral ligament, and the anterior band of the medial collateral ligament. Secondary stabilizers of the elbow include the radiocapitellar articulation as well as the tendon origins of the flexor and extensor muscles of the forearm.
Distal humeral deformities are often the result of malunited fractures in children and adults. In children, the deformity can often be well tolerated for several years. However, the abnormal alignment of the elbow results in growth disturbances, remodeling and wear of the remainder of the elbow joint that over time can lead to ligamentous insufficiency, and nerve dysfunction and degenerative changes in the elbow joint. The most common deformities are varus and extension of the distal humerus as a result of malunited supracondylar humerus fractures. Cubitus varus results in an abnormal vector of the triceps tendon that ultimately worsens the deformity and causes attenuation of the lateral ulnar collateral ligament leading to tardy posterolateral rotatory instability of the elbow.
INDICATIONS/CONTRAINDICATIONS
Patients with distal humeral malunions can present with a myriad of complaints. Typically these fall into three categories: the first is the patient who develops degenerative changes in the joint resulting in contractures and pain; while the second group develops instability and complains of progressive deformity and mechanical symptoms, the third group develops nerve-related symptoms as a result of the deformity. Symptomatic deformity of the distal humerus is the primary indication for an osteotomy, with the goal to restore alignment and joint biomechanics. In the face of instability, osteotomy to realign the joint forces is essential for success of the ligament reconstruction.
Clinical evaluation of the elbow alignment should be performed with the forearm supinated in and in full extension. The angle between the humeral shaft and ulnar shaft can be measured to determine the carrying angle of the humerus (Fig. 11-1). Care must be taken to avoid internal or external rotation of the shoulder as this can exacerbate or lessen the actual deformity, especially if a flexion contracture exists. Accurate assessment of range of motion, bony impingement, and stability of the elbow is essential. Signs of instability include catching or clicking with range of motion from flexion to extension as well as a positive posterolateral rotary drawer or pivot shift maneuver. Fluoroscopic evaluation allows for a dynamic examination of the elbow and aids in the assessment
of joint stability. Careful neurologic examination is important to assess for compression of the ulnar nerve in the cubital tunnel as a result of the deformity, instability, or a snapping medial triceps.
of joint stability. Careful neurologic examination is important to assess for compression of the ulnar nerve in the cubital tunnel as a result of the deformity, instability, or a snapping medial triceps.
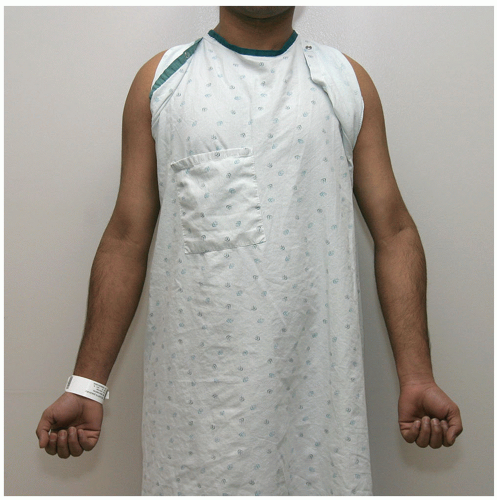 FIGURE 11-1 Clinical photograph of a patient with varus deformity of the distal humerus. Examination with the arm supination allows for accurate assessment of the deformity. |
Computer tomography (CT) scan with three-dimensional (3D) reconstruction can be helpful in characterization of the deformity as most malunions have deformity in more than one plane. Newer computer software can also be used as part of the preoperative planning to determine the exact location and orientation of the osteotomy cuts to allow for appropriate realignment of the distal humerus. Advances in 3D printing methods now allow for the creation of plastic models that can be very helpful in understanding the deformity and planning the corrective osteotomy.
The primary indications for a distal humeral osteotomy are pain relief and to restoration of function associated with a malunion of the distal humerus. Typically, a symptomatic varus deformity greater than 15 degrees is an indication for distal humeral osteotomy. In the case of instability, the alignment of the distal humerus should be corrected at the time of ligament reconstruction.
Contraindications for distal humeral osteotomy include the presence of infection, patient noncompliance, or unrealistic expectations. Caution should be advised in patients who actively use tobacco or who have impaired healing ability due to underlying medical conditions or poor nutrition. The use of prophylactic osteotomy in the asymptomatic patient with significant deformity is debatable, and careful patient selection should be advised prior to proceeding with the procedure. The presence of degenerative changes in the elbow joint may be an indication for total elbow arthroplasty instead of corrective osteotomy. There is little information as to the degree of arthritic change that can be accepted in the osteotomy patient. Alterative treatment options for patients with minor deformity-associated degenerative changes and contracture include a debridement procedure with capsular release and recontouring ostectomy of the distal humerus to improve range of motion. In the face of instability associated with deformity in the elderly, low-demand patient-isolated ligament reconstruction may provide stability with less morbidity than an osteotomy. If the patient’s symptoms are isolated to the ulnar nerve, decompression or transposition of the nerve may be all that is needed. Careful preoperative evaluation is needed to assess which aspects of the patient’s pathology are actually symptomatic.
PREOPERATIVE PREPARATION
The development of a clear understanding of the patient’s deformities and anatomy is essential for a successful osteotomy. Full-length radiographs of bilateral upper extremities are useful for determining the degree of varus angulation of the humerus. The alignment or carrying angle of the arm can be assessed radiographically by determining the angle between the long axis of the humerus and the ulna (Fig. 11-2). The contralateral extremity alignment is helpful as a template for the desired degree of correction. The lateral radiograph can be examined for extension or flexion malunions by using drawing the anterior cortical line that should bisect the capitellum on the lateral radiograph.
A CT scan with 3D reconstruction is extremely valuable in understanding the degree and location of the deformity, especially with regard to rotational deformities of the distal humerus (Fig. 11-3A and B). We routinely obtain a CT scan prior to the surgery, and newer computer software allows for
templating of the proposed osteotomy, which is easier than the traditional paper cutouts that were used historically. In difficult cases with extreme deformities, a 3D model of the humerus can be obtained to allow for actual preoperative performance of the osteotomy on the model.
templating of the proposed osteotomy, which is easier than the traditional paper cutouts that were used historically. In difficult cases with extreme deformities, a 3D model of the humerus can be obtained to allow for actual preoperative performance of the osteotomy on the model.
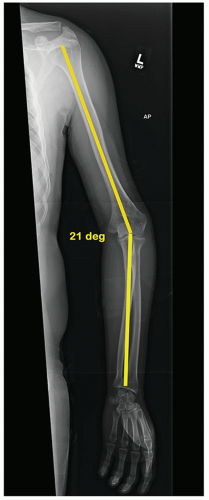 FIGURE 11-2 Bone length radiograph of the left upper extremity demonstrating the measurement of the varus deformity of 21 degrees. |
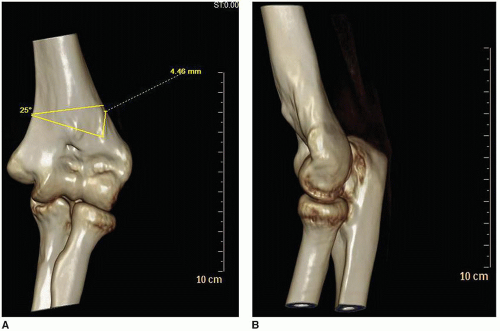 FIGURE 11-3 Three-dimensional CT scan images of distal humeral fracture malunion. A: AP view demonstrating varus deformity. B: Lateral view demonstrating extension deformity. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








