Michael J. Gardner
M. Bradford Henley
Sterile Instruments/Equipment
- Large external fixator
- 2.5 mm, 4.0 mm, or 5.0 mm Schanz pins, or large K-wires or Steinmann pins for manipulative joysticks
- Large pointed bone reduction clamps (Weber clamps)
- Large quadrangular ball-spike clamp
- Femoral distractor
- Ball-spike pushers
- Shoulder hook/bone hook
- K-wires and wire driver/drill
- Smilie knee retractors and “Z-retractors”
- Implants
- Nonlocking condylar buttress plate
- Locking plate
- Retrograde nail, if desired
- Blade plate
- Nonlocking condylar buttress plate
Patient Positioning
- The patient is usually placed in a supine position on a radiolucent table.
- A padded bump is placed under the ipsilateral hip to neutralize hip rotation.
- The lower extremity is elevated on a soft ramp cushion or other padded bolster to facilitate lateral radiographic imaging.
- A padded bump is placed under the ipsilateral hip to neutralize hip rotation.
- Alternatively, lateral positioning can be used for a lateral approach for direct ORIF.
- This is useful for ORIF of supracondylar distal femur fractures for periprosthetic injuries where the entire femur is to be plated.
- This is also useful for supracondylar nonunions.
- This is useful for ORIF of supracondylar distal femur fractures for periprosthetic injuries where the entire femur is to be plated.
- The C-arm is positioned on the contralateral side of the OR table, opposite the operative extremity.
Surgical Approaches
- Surgical approach is determined by the fracture pattern.
- The direct lateral approach may be utilized for the majority of supracondylar and intercondylar femur fractures (Fig. 17-1).
Figure 17-1. The direct lateral approach can be used effectively for most Type C1 and C2 distal femur fractures. The incision is made along the shaft of the femur, and often needs to be extended distally to the level of Gerdy’s tubercle.
![]()
- This approach avoids incision of the quadriceps tendon.
- The distal portion of the vastus lateralis is elevated off of the lateral intermuscular septum.
- It is preferred for its soft tissue sparing benefits.
- If visualization of the distal articular surface is necessary, split and retract the iliotibial band anterior to Gerdy’s tubercle and dissect towards the lateral border of the patellar tendon, then curving distally towards its insertion.
- Avoid an incision crossing the patellar tendon.
- The distal limb of the incision may be extended distally to the tibial tuberosity lateral to the tendon, to allow for an increased mobilization of the anteromedial soft tissues.
- Avoid an incision crossing the patellar tendon.
- Allowing temporary limb shortening at the supracondylar level by bayonet apposition of the shaft and metaphyseal portions of the fracture removes the tension from the extensor mechanism, allowing improved medial soft tissue retraction of the extensor mechanism and visualization of the distal articular surface, femoral trochlea, intercondylar notch, and medial femoral condyle, if required (Fig. 17-2).
- Hyperextending the knee with a bump under the heel can also relax the extensor mechanism to improve visualization.
Figure 17-2. By extending the incision into the lateral part of the fat pad (to the patellar tendon), the distal articular surface of both femoral condyles can be visualized.
![]()
- Alternatively, a lateral parapatellar approach may be used in cases with significant intercondylar comminution, and/or for associated coronal plane fractures (Fig. 17-3).
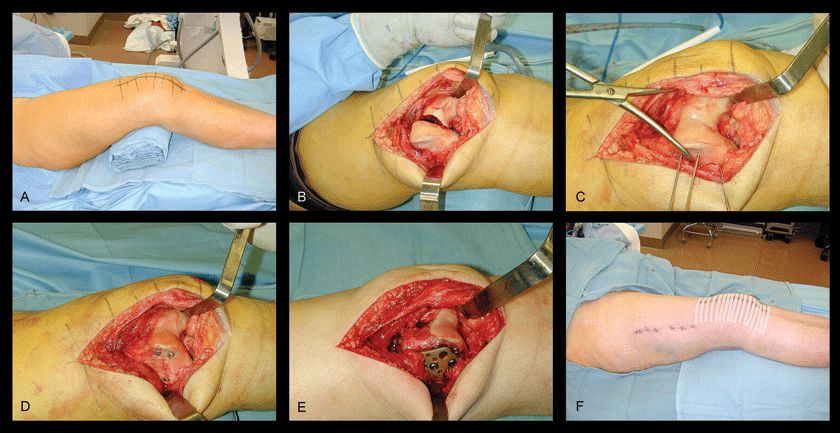
Figure 17-3. Using a lateral parapatellar approach through a midline or paramedian incision, the articular surface is visualized, and sagittal plane fracture reduction is facilitated (A,B). This approach is anterolateral and thus permits coronal plane fracture fixation (Hoffa fractures) with anterior-to-posterior screws, especially if these involve the medial condyle. The intercondylar articular displacement is then reduced under direct vision, and transcondylar K-wires are placed (C), followed by peripheral screws (D). This allows room for a locking plate to be placed unobstructed (E). The proximal screws may still be inserted percutaneously with this approach (F). (From Nork SE. Supracondylar femur fractures: open reduction and internal fixation. In: Master Techniques in Orthopaedic Surgery: Fractures. Philadelphia: Lippincott Williams Wilkins, 2006. With permission.)
![]()
- This approach sacrifices the superolateral geniculate artery to the patella and incises the quadriceps tendon.
- Rarely, a medial approach may be used in conjunction with a lateral approach, if necessary, for additional medial condyle access, or for placement of anterior to posterior screws for coronal plane Hoffa fractures.
- The most proximal of the screws should be placed proximally enough so that it is posterior in the femoral condyle, ensuring adequate fixation.
- This proximal screw can usually be inserted medial (and superior) to the femoral trochlea’s articular cartilage.
- This position is typically proximal to the articular surface (Fig. 17-4).
- The most proximal of the screws should be placed proximally enough so that it is posterior in the femoral condyle, ensuring adequate fixation.
Figure 17-4. K-wire and screw placement for medial Hoffa fracture. These may be placed percutaneously as cannulated screws, or through a small medial parapatellar arthrotomy.
Reduction and Fixation Techniques
- Articular reduction should be performed first.
- Typically, coronal plane (Hoffa) fractures are reduced and provisionally stabilized prior to sagittal plane fractures in the intercondylar region.
- This sequence may be reversed depending upon the complexity of each fracture.
- Coronal plane fractures of the lateral and medial condyles can be reduced and compressed with a large pointed reduction clamp.
- Medial condyle coronal plane fractures may be clamped through the lateral incision.
- One tine is placed just deep to the extensor mechanism on the anterior aspect of the medial femoral condyle, and the other tine is placed through the intercondylar notch on the posterior medial femoral condyle (Fig. 17-5).
- This sequence may be reversed depending upon the complexity of each fracture.
Figure 17-5. A,B: A large Weber clamp may be placed through the intercondylar notch through the lateral incision to access some medial femoral condyle coronal plane fracture patterns.
- Multiple anterior to posterior K-wires may be necessary to provisionally secure these fractures during screw placement.
- When using nonlocking lateral plates or polyaxial locking plates, Hoffa fractures should ideally be stabilized definitively with interfragmentary lag screws prior to plate placement.
- However, when using non-polyaxial locking plate implants, Hoffa fractures may require definitive stabilization after plate placement to avoid interference between the lateral-to-medial plate screws and the anterior-to-posterior Hoffa/condylar screws.
- Fracture location and obliquity in the lateral condyle determines the screw orientation, which should be perpendicular to the fracture plane.
- These are usually 2.7- or 3.5-mm cortical screws (countersunk, if placed through articular cartilage) or headless compression screws placed from anterior to posterior (Fig. 17-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




