Distal Chevron First Metatarsal Osteotomy
Harold B. Kitaoka
Hallux valgus is a commonly occurring disorder of the foot affecting adults and adolescents. There may be symptoms of pain over the medial eminence or bunion associated with hallux valgus. The pain is usually related to the use of enclosed shoes. The deformity may be flexible initially and, with the passage of time, become more rigid and more difficult to correct manually. There may be related forefoot disorders such as a hammer toe of the second, metatarsalgia of the second, soft corn in lateral hallux or medial second toe, and first metatarsophalangeal (MTP) degenerative arthritis. Most patients are improved with the use of appropriate footwear with a wider toe box, softer leather upper, and low heel and stretching the leather over the bunion with a ring and ball device. Convincing patients of the importance of footwear with these characteristics may be as challenging as the operative procedure. Some surgeons advocate shoe inserts with an arch support because there may be an associated flatfoot deformity. Patients may feel as though an orthotic further constricts the forefoot.
The distal metatarsal chevron osteotomy is the most popular operation for correction of mild and moderate hallux valgus deformities. There are reports of performing the operation for severe malalignment, featuring marked displacement of the distal metatarsal or combining the procedure with others, such as a proximal phalangeal osteotomy (1). Since the operation was described in early reports by Austin and Leventen (2) and by Johnson et al. (3), it has been modified in dozens of ways in numerous publications in the orthopedic and podiatric literature. These modifications include various shapes of medial capsular incisions, release of lateral capsular contractures, altering the position and angle of osteotomy in the sagittal plane (4), angling the axis of the osteotomy distally to maintain length, adding a closing wedge osteotomy component (biplanar osteotomy) (5), combining it with a proximal phalangeal osteotomy, addition of fixation with a percutaneous pin or
absorbable pin or with a staple or bone peg (6), fixation with a Herbert screw or compression screw or plate with screws or absorbable screws, and corrective soft dressing or slipper cast or short leg cast. It is conceivable that the same successful result may be achieved by different modifications of the basic procedure.
absorbable pin or with a staple or bone peg (6), fixation with a Herbert screw or compression screw or plate with screws or absorbable screws, and corrective soft dressing or slipper cast or short leg cast. It is conceivable that the same successful result may be achieved by different modifications of the basic procedure.
The chevron osteotomy presented was modified since its early description: The osteotomy is made with a more acute angle; the apex of the osteotomy is located distal to the center of the head, transarticular lateral capsulotomy, and internal fixation of the osteotomy. This chapter describes a chevron osteotomy with internal fixation using an absorbable pin to limit the potential for osteotomy displacement postoperatively. Although the chevron osteotomy has inherent stability, displacement can occur if the toe is traumatized, such as from a fall in the early postoperative period. Fixation ensures the metatarsal head will stay in the proper position and allows early weight bearing and range-of-motion exercises without osteotomy displacement.
INDICATIONS AND CONTRAINDICATIONS
Chevron osteotomy is indicated in patients with symptomatic mild to moderate hallux valgus deformity with no significant arthritis. Mild to moderate deformities are those with an intermetatarsal (IM) 1-2 angle of 16° or less in a weight-bearing anteroposterior radiograph of the foot (Fig. 1.1). More severe deformities may not be adequately corrected with this operation. It is preferable if the patient has a painless, mobile MTP joint that may be passively corrected to anatomic alignment. The chevron osteotomy is occasionally indicated in patients who have failed hallux valgus operations, such as simple bunionectomy with medial capsulorrhaphy.
Chevron osteotomy is not indicated for patients who have general or local conditions that preclude operative treatment, such as skin ulceration, local or remote infection, or dysvascular foot, or for patients who are unable to comply with required postoperative immobilization and protected weight bearing. Operating on patients with asymptomatic hallux valgus deformities is generally not advisable, nor is surgery because of anticipation of difficulty at some uncertain time in the future. Patients must understand that the consequence of returning to fashionable, constrictive footwear is a higher rate of recurrent deformity and symptoms. Significant MTP arthritis and severe hallux valgus with
an IM 1-2 angle of more than 16° are also contraindications for the operation. Neuropathy is a relative contraindication. The patient’s chronologic age is not as an important factor as physiologic age in considering this procedure. Although it was previously believed that the operation was not indicated in patients older than 50 years of age, this concept has been challenged by favorable clinical results in these patients. An MTP joint that is rigid, is tender, has painful motion, has crepitus with motion, and is not passively correctable to anatomic varus-valgus alignment has a worse prognosis.
an IM 1-2 angle of more than 16° are also contraindications for the operation. Neuropathy is a relative contraindication. The patient’s chronologic age is not as an important factor as physiologic age in considering this procedure. Although it was previously believed that the operation was not indicated in patients older than 50 years of age, this concept has been challenged by favorable clinical results in these patients. An MTP joint that is rigid, is tender, has painful motion, has crepitus with motion, and is not passively correctable to anatomic varus-valgus alignment has a worse prognosis.
PREOPERATIVE PLANNING
Planning for a chevron osteotomy includes a history, examination of the foot, general health evaluation, radiologic interpretation, and consideration of expectations. An ideal patient for a chevron osteotomy describes the symptoms in realistic terms and has appropriate expectations. When the pain is excruciating, involves areas of the foot and ankle other than the bunion, or is present even without the use of shoes, a chevron osteotomy may not be the answer.
Besides noting the presence of the hallux valgus deformity, the foot examination should include measurement of MTP joint movement in dorsiflexion and plantarflexion relative to the plantar foot. Many patients with hallux valgus are unaware of their restricted MTP motion preoperatively, but they may recognize the limitation after the operation. It is also useful to determine flexibility of the hallux in the varus-valgus plane and notice whether the toe deformity is easily correctable. A deformity that is not passive correctable may be an indication of an arthritic joint or a laterally facing distal articular surface of the metatarsal (i.e., increased distal metatarsal articular angle) that is not effectively treated with a conventional chevron osteotomy. The neurovascular status of the foot should be documented. If posterior tibial and dorsalis pedis pulses are not palpable, additional investigation is warranted, such as a Doppler examination or noninvasive vascular studies.
The foot should be examined for any difficulties with lesser toe deformities or callus formation beneath the second metatarsal head, because they may be a source of symptoms after hallux valgus surgery. An adjunctive procedure for a lesser metatarsal is occasionally indicated with a chevron osteotomy of the first metatarsal. However, restoring the hallux alignment and first metatarsal head in an improved weight-bearing position with the chevron osteotomy may decrease the overloading of the second metatarsal and reduce in callus formation and pain.
A general health evaluation is important to anticipate difficulties that may occur. The presence of diabetes mellitus, peripheral vascular disease, peripheral neuropathy, and selected medications such as prednisone all have specific implications.
Radiologic evaluation should include weight-bearing anteroposterior and lateral views. The IM 1-2 angle is measured as the angle between lines drawn from the center of the head to the center of the base for the first and second metatarsals. This angular measurement may in some instances underestimate the magnitude of deformity, as occurs in feet with metatarsus adductus. The hallux valgus angle measured between the first metatarsal axis and the shaft of the proximal phalanx is also determined. Degenerative arthritis at the MTP joint can be evaluated on the anteroposterior and lateral radiographs.
A chevron osteotomy is usually performed under ankle block anesthesia as outpatient surgery. Patients who are particularly anxious can still tolerate an ankle block anesthetic with some degree of parenteral sedation. An ankle block can be performed bilaterally, although occasionally patients may prefer general anesthesia.
SURGICAL TECHNIQUE
Ankle block anesthesia is administered. The patient is positioned supine on the surgical table.
A 4-inch rubber Esmarch bandage is applied around the foot and ankle for exsanguination and is wrapped several times around the ankle for hemostasis. Applying a double-thickness stockinette over the skin before application of the Esmarch bandage provides padding to the skin and increases patient acceptance of the compression at the ankle.
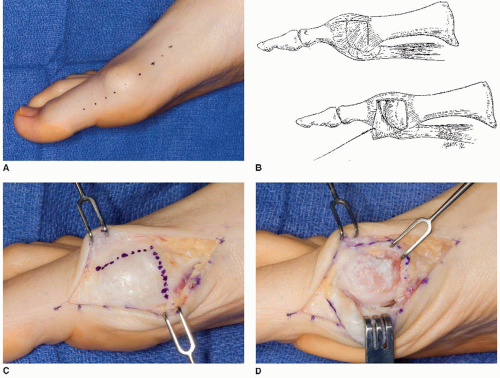
A longitudinal skin incision is placed medially and centered over the medial eminence (Fig. 1.2A).
The subcutaneous tissue and bursal tissues are elevated from the capsule over the medial eminence, taking care to protect the dorsomedial sensory nerve and the plantar-medial nerve to the great toe.
When the medial capsule has been exposed, an inverted L-shaped incision is made with the horizontal limb dorsal-medially along the dorsal margin of the distal metatarsal and vertical limb several millimeters proximal to the medial eminence (Fig. 1.2B and C).
The capsular structures are dissected off the medial eminence but not from the dorsal metatarsal (Fig. 1.2D).
Excessive stripping of soft tissues from the lateral aspects of the metatarsal head may deprive the metatarsal head of part of its extraosseous blood supply and is not indicated.
Releasing lateral joint contracture by perforating the lateral capsule under direct vision may aid in the realignment of the hallux. Multiple clinical and vascular anatomic studies (7,8) demonstrate that the distal chevron osteotomy with lateral capsulotomy may be accomplished without sacrificing the extraosseous blood supply to the metatarsal head and creating subsequent osteonecrosis.
The MTP joint is exposed with the L-shaped flap only enough to allow resecting the medial eminence without traumatizing the capsular tissue, which is important for later capsular repair.
Starting medial to the sagittal groove, the medial eminence is removed in a plane parallel to the metatarsal diaphysis (Figs. 1.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree