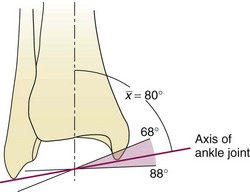
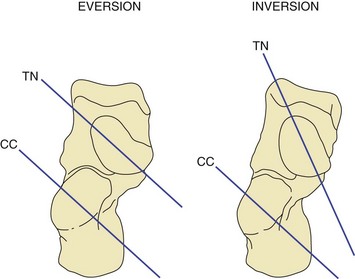
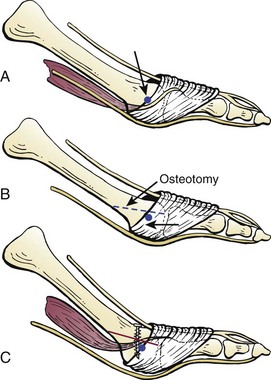
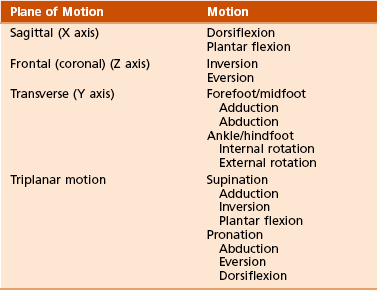
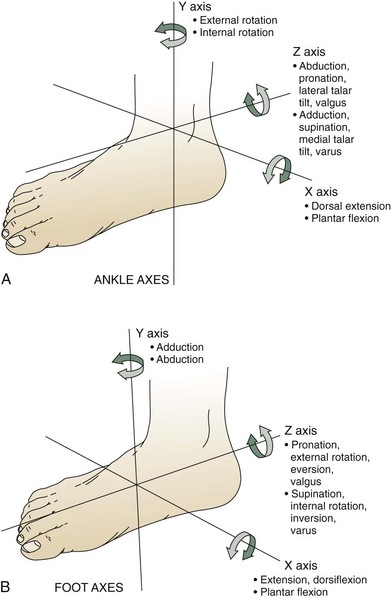
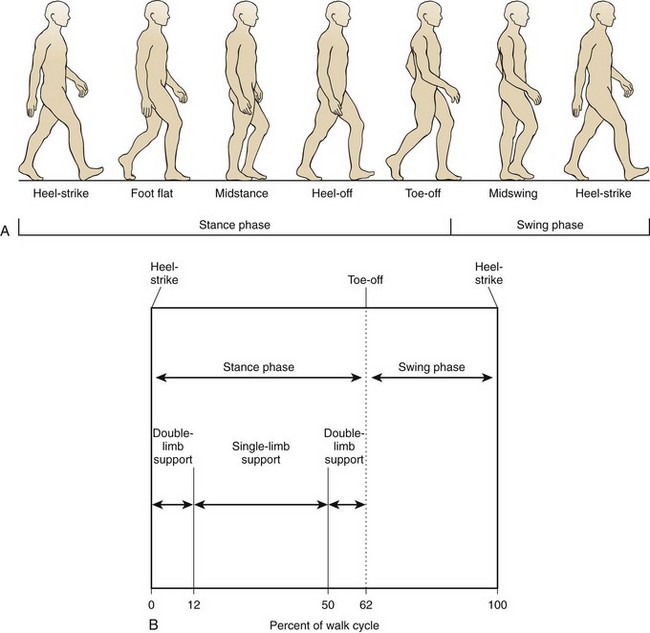
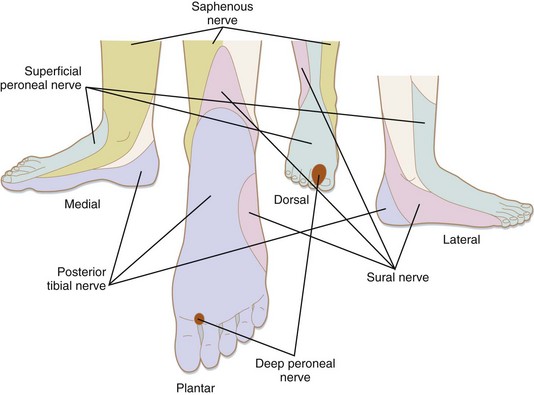
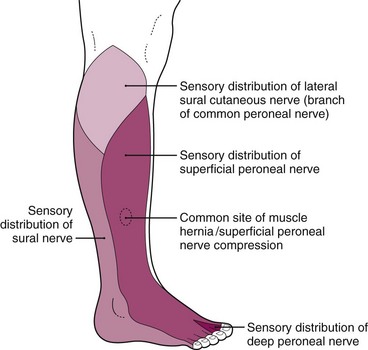
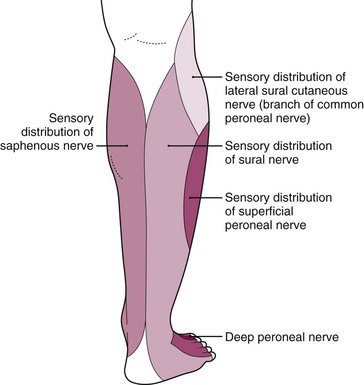
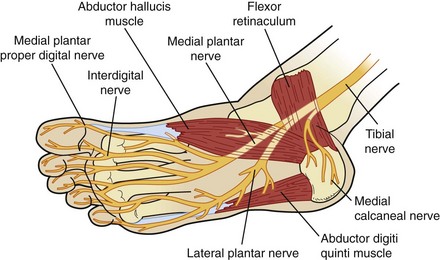
Chapter 6 SECTION 1 BIOMECHANICS OF THE FOOT AND ANKLE SECTION 2 PHYSICAL EXAMINATION OF THE FOOT AND ANKLE SECTION 3 RADIOGRAPHIC EVALUATION OF THE FOOT AND ANKLE SECTION 5 JUVENILE AND ADOLESCENT HALLUX VALGUS SECTION 7 LESSER-TOE DEFORMITIES SECTION 8 HYPERKERATOTIC PATHOLOGIES SECTION 11 NEUROLOGIC DISORDERS I. Interdigital Neuritis (Morton Neuroma) IV. Anterior Tarsal Tunnel Syndrome V. Sequelae of Upper Motor Neuron Disorders VI. Charcot-Marie-Tooth Disease III. First Metatarsophalangeal Joint Injuries IV. Tarsometatarsal Fractures and Dislocations (Lisfranc Injury) V. Midfoot Injuries (Excluding Lisfranc Injuries) IX. Peritalar (Subtalar) Dislocations This chapter provides a review of adult foot and ankle disorders and deformities. Pediatric and congenital deformities are covered in Chapter 3, Pediatric Orthopaedics. The primary functions of the foot and ankle are to provide support and forward ambulation. 1. Ankle mortise is formed by the tibial plafond, medial malleolus, and lateral malleolus (Figure 6-1). 2. Mortise articulates with the dome of the talus. 3. Mortise widens and ankle becomes more stable in dorsiflexion due to shape of talar dome (wider anteriorly). 4. A simplified model of the ankle joint has a horizontal axis from anteromedial to posterolateral and a coronal axis from superomedial directed distally and laterally to the tip of the fibula (between the malleoli) (Figure 6-2). 5. Responsible for most sagittal plane motion of the foot and ankle 6. 23 to 48 degrees plantar flexion 7. 10 to 23 degrees dorsiflexion 1. Distal fibula—convex medial surface 2. Incisura fibularis—concave surface of distal lateral tibia 3. Fibula rotates (~2 degrees) within incisura during ankle motion and ambulation. Ankle dorsiflexion results in external rotation and proximal translation of the fibula. 4. Mortise widens 1 to 1.5 mm during motion from plantar flexion to dorsiflexion. C Ligamentous anatomy (Figure 6-3) 1. The lateral ankle ligaments function as a restraint to varus forces at the ankle. 2. The distal tibiofibular joint (ankle syndesmosis) and fibula provide stability against lateral talar translation. 3. Deltoid ligament complex—main stabilizer of the ankle during stance 1. The hindfoot includes the talus, calcaneus, and cuboid. The subtalar, calcaneocuboid (CC), and talonavicular (TN) joints are included (Figure 6-4). The hindfoot functions in inversion and eversion. E The midfoot begins at the articulation between the navicular and the cuneiforms along with cuboid and the fourth and fifth metatarsals. The midfoot also includes the tarsometatarsal (TMT) joints. F The forefoot includes all structures distal to the TMT joints (Figure 6-5). G The CC and TN joints are collectively referred to as the midtarsal, transverse tarsal, or Chopart joint. 1. This joint is important for providing stability of the hindfoot and midfoot to produce a rigid lever at heel-rise. 2. During heel-strike (hindfoot valgus, forefoot abduction, and dorsiflexion of the ankle), the transverse tarsal joints are parallel and supple, adapting to the uneven ground. 3. During toe-off (hindfoot varus, forefoot adduction, and plantar flexion of the ankle), these joints become divergent and lock, providing stiffness to the foot for forward propulsion (Figure 6-6). H The collective TMT joint complex is referred to as the Lisfranc joint. I The foot is also divided into three columns. 1. The medial column includes the first metatarsal, the medial cuneiform, and the navicular. 2. The middle column includes the second and third metatarsals, the middle cuneiform, and the lateral cuneiform. 3. The lateral column includes the fourth and fifth metatarsals and the cuboid. 4. The lateral column has the most sagittal mobility, and the middle column has the least. 5. The sagittal mobility of the lateral column imparts the flexibility necessary for walking on uneven ground. 6. The rigidity of the middle column allows for a rigid lever arm during push-off. J The foot has longitudinal and transverse arches. Stability of these arches is provided by a combination of the bony architecture, ligamentous attachments, and muscle forces. K Ligamentous stability to the midfoot is provided through longitudinal and transverse ligaments on the plantar and dorsal aspects of each joint. 1. The plantar ligaments are thicker and stronger than their dorsal counterparts. 2. The primary stabilizer of the longitudinal arch is the interosseous ligaments and not the plantar fascia. The plantar fascia is a secondary stabilizer. L The Lisfranc joint complex has a specialized bony and ligamentous structure, providing stability to this joint. 1. The middle cuneiform ends more proximally than the medial and lateral cuneiforms. The second metatarsal therefore extends more proximally than the surrounding metatarsals. This “keystone” effect imparts inherent bony stability. 2. Dorsal and plantar ligaments extend from the second metatarsal to each of the three cuneiforms. 3. The largest and strongest of these ligaments is the Lisfranc ligament, traveling from the medial cuneiform to the base of the second metatarsal. M The midfoot provides an important bridge between the hindfoot and forefoot. It provides both flexibility and stability necessary for normal gait and other activities. A The bony forefoot comprises the metatarsals and phalanges. B The first metatarsal is the widest and shortest and bears 50% of the weight during gait. C The second metatarsal is usually the longest and experiences more stress than the other lesser metatarsals. D The lesser toes are controlled by a balance among them. E The intrinsic tendons pass plantar (providing a flexion force) to the MTP joint axis proximally and pass dorsal to the axis distally (providing an extension force). 1. Plantar migration of this axis after a Weil (oblique shortening) osteotomy of the metatarsal leads to a “cock-up” toe. The tendons are now relatively dorsal to the MTP axis of rotation (Figure 6-7). 2. Loss of intrinsic function as seen in hereditary and motor sensory neuropathy or diabetic neuropathy predictably leads to claw toes. III FOOT POSITIONS VERSUS FOOT MOTIONS A Foot positions are defined in a manner different from that of foot motions. C Foot motions in the three axes of rotation are illustrated in Figure 6-8 and summarized in Table 6-1. 1. The critical assessment is to determine the relationship of the forefoot to the hindfoot. 2. If the heel is in a neutral position (subtalar neutral), the forefoot should be parallel with the floor to meet the ground flush (plantigrade). A One full gait cycle, from heel-strike to heel-strike, is termed a “stride.” 1. Each stride is composed of a stance phase (heel-strike to toe-off, 62% of the cycle) and a swing phase (toe-off to heel-strike, 38% of the cycle) (Figure 6-10). 2. Walking is defined by a period of double-limb support in addition to always having one foot in contact with the ground throughout the gait cycle. 3. Ground reaction forces are approximately 1.5 times body weight during walking and 3 to 4 times body weight during running. 4. As the speed of gait increases, the stance phase decreases. B Soft tissue contributions to gait mechanics A The foot and ankle should be inspected for 2. Callouses—areas of abnormally increased pressure 3. Signs of peripheral vascular disease—lack of hair, increased skin pigmentation (hemosiderin deposition) 4. Swelling—symmetric (likely systemic etiology) versus asymmetric (trauma, venous thrombosis, cellulitis, osteomyelitis, focal musculoskeletal etiology) (Figure 6-12) 5. Ecchymosis—plantar ecchymosis associated with tarsometatarsal injury (Lisfranc injury) (Figure 6-13) B The patient’s gait should be evaluated. A Palpate the dorsalis pedis and posterior tibial pulses. If they are not present, consider noninvasive studies. A The sensory examination should assess the following five cutaneous nerves that supply the feet (Figure 6-17). 1. Saphenous—medial ankle and hindfoot 2. Superficial peroneal (Figure 6-18) 3. Deep peroneal—first dorsal web space 4. Sural—posterolateral border of the leg and the lateral border of the foot (Figure 6-19) 5. Tibial—plantar foot (Figure 6-20) B Inability to sense a Semmes-Weinstein 5.07 monofilament is consistent with neuropathy. A When assessing strength, keep in mind the relation the tendon has to the axis of the ankle. For example, if it passes medially and posteriorly, the function of that structure will be to provide plantar flexion and inversion (tibialis posterior). B When assessing motor function of the foot and ankle, the following muscles should be tested. 1. Tibialis anterior—ankle dorsiflexion, L3-4 2. Extensor hallucis longus—great-toe extension, L4-5 3. Peroneus longus and brevis—hindfoot eversion, L5-S1 4. Posterior tibialis—hindfoot inversion, L4-5 C It is important to remember that neurologic deficits can be secondary to more proximal pathology (e.g., central nervous system, spinal cord, nerve root). A Palpation of the tendinous and bony anatomy of the foot and ankle is facilitated by its subcutaneous nature. A detailed examination can typically reproduce the patient’s source of pain, allowing the examiner to identify the cause without the need for supplementary studies.
Disorders of the Foot and Ankle
section 1 Biomechanics of the Foot and Ankle
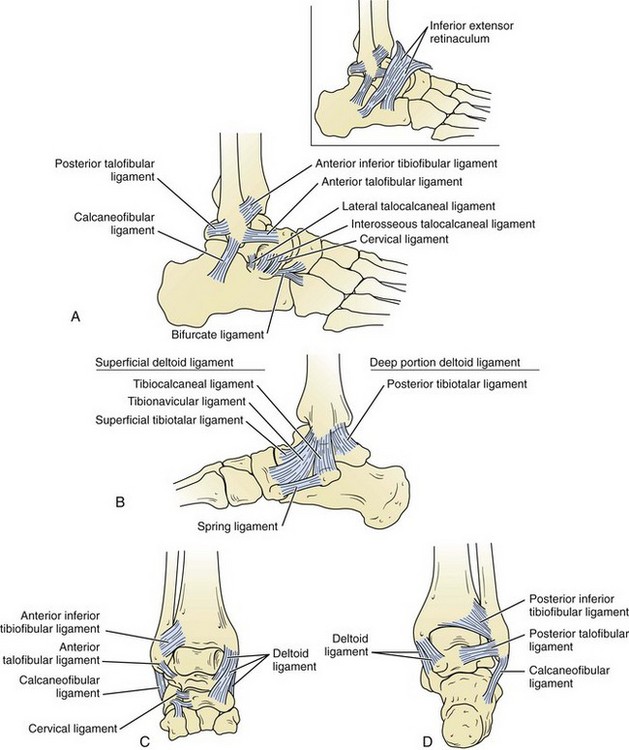
 The anterior talofibular ligament originates from the anteroinferior aspect of the lateral malleolus, 1 cm proximal to its tip, and extends to the lateral aspect of the talar neck.
The anterior talofibular ligament originates from the anteroinferior aspect of the lateral malleolus, 1 cm proximal to its tip, and extends to the lateral aspect of the talar neck.
 The calcaneofibular ligament extends from the tip of the lateral malleolus to the lateral aspect of the calcaneus.
The calcaneofibular ligament extends from the tip of the lateral malleolus to the lateral aspect of the calcaneus.
 The posterior talofibular ligament extends from the posterior lateral malleolus to the posterolateral talus.
The posterior talofibular ligament extends from the posterior lateral malleolus to the posterolateral talus.
 The anterior talofibular ligament is the weakest ankle ligament, and the posterior talofibular ligament is the strongest.
The anterior talofibular ligament is the weakest ankle ligament, and the posterior talofibular ligament is the strongest.
 The deep deltoid ligament extends from the apex of the medial malleolus to the medial talar body. It functions primarily to resist lateral talar translation.
The deep deltoid ligament extends from the apex of the medial malleolus to the medial talar body. It functions primarily to resist lateral talar translation.
 The superficial deltoid ligament extends from the distal medial malleolus to the navicular bone, sustentaculum tali of the calcaneus, medial talus, and spring ligament. It functions primarily to resist valgus ankle force (i.e., talar tilt).
The superficial deltoid ligament extends from the distal medial malleolus to the navicular bone, sustentaculum tali of the calcaneus, medial talus, and spring ligament. It functions primarily to resist valgus ankle force (i.e., talar tilt).
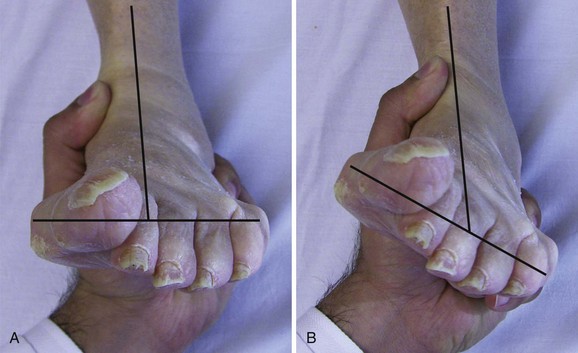
 If the first ray is elevated, the forefoot is in varus position. If the first ray is flexed, the forefoot is in valgus position. This should not be confused with hindfoot varus or valgus.
If the first ray is elevated, the forefoot is in varus position. If the first ray is flexed, the forefoot is in valgus position. This should not be confused with hindfoot varus or valgus.
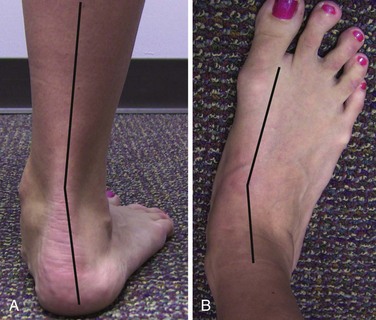
 For example, in a long-standing flatfoot deformity the heel is valgus and the forefoot has compensated by going into varus or supinating to keep the flat to the ground.
For example, in a long-standing flatfoot deformity the heel is valgus and the forefoot has compensated by going into varus or supinating to keep the flat to the ground.
 This difference is due to the increased load after the float phase of running, in which there is no foot in contact with the ground.
This difference is due to the increased load after the float phase of running, in which there is no foot in contact with the ground.
 Anterior tibialis—contracts eccentrically
Anterior tibialis—contracts eccentrically
 Controls the rate at which the foot strikes the ground. In patients with footdrop, the rapid strike of the foot can result in a loud “slap” during heel-strike.
Controls the rate at which the foot strikes the ground. In patients with footdrop, the rapid strike of the foot can result in a loud “slap” during heel-strike.
 Gastrocnemius-soleus complex—concentric contraction
Gastrocnemius-soleus complex—concentric contraction
 In addition, as the foot progresses from heel-strike to toe-off, the following changes allow the foot to convert from a flexible shock absorber to a rigid propellant.
In addition, as the foot progresses from heel-strike to toe-off, the following changes allow the foot to convert from a flexible shock absorber to a rigid propellant.
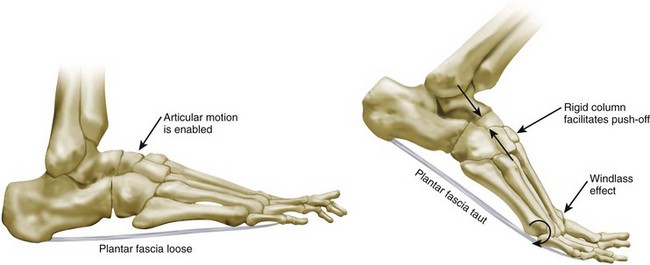
 The plantar fascia, which attaches to the plantar medial heel and runs the length of the arch to the bases of each proximal phalanx, is tightened as the MTP joints extend. The longitudinal arch is accentuated.
The plantar fascia, which attaches to the plantar medial heel and runs the length of the arch to the bases of each proximal phalanx, is tightened as the MTP joints extend. The longitudinal arch is accentuated.
 The hindfoot supinates, with firing of the posterior tibial tendon.
The hindfoot supinates, with firing of the posterior tibial tendon.
 The transverse tarsal joint locks and provides a rigid lever arm for toe-off.
The transverse tarsal joint locks and provides a rigid lever arm for toe-off.
section 2 Physical Examination of the Foot and Ankle
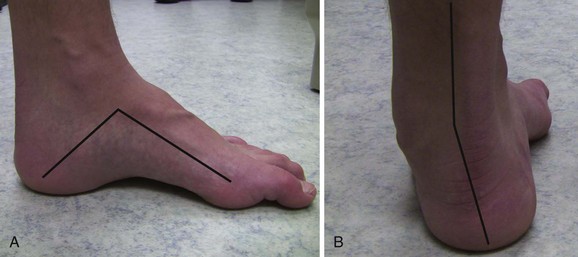
 Cavovarus—elevated longitudinal arch with hindfoot varus and plantar-flexed first ray (Figure 6-14)
Cavovarus—elevated longitudinal arch with hindfoot varus and plantar-flexed first ray (Figure 6-14)
 Pes planus—flat longitudinal arch with hindfoot valgus (Figure 6-15)
Pes planus—flat longitudinal arch with hindfoot valgus (Figure 6-15)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Disorders of the Foot and Ankle