, Paul D. Siney1 and Patricia A. Fleming1
(1)
The John Charnley Research Institute Wrightington Hospital, Wigan, Lancashire, UK
The fear of dislocation is undoubtedly the main reason why the small femoral head has not become universally popular (1978)
It was 15 years from the introduction of the operation and over 13,000 LFAs before Etienne, Cupic and Charnley [1] turned their attention to a detailed review of the incidence and causes of post-operative dislocation. The very low incidence was attributed to full exposure of the hip, preservation of the capsule, correct alignment of the components, secure re-attachment of the greater trochanter and the use of the abduction pillow post-operatively.
Monitoring of the results was routine. In an attempt to reduce the incidence of dislocation still further two changes were introduced: transverse reaming of the acetabulum and the change of the cup design to the long posterior wall (LPW) model. What was the clinical benefit of the changes? What was the effect on the already very low incidence of post-operative dislocation?
Transverse Reaming of the Acetabulum
Preparation of the acetabulum was a well defined sequence of steps; centering for the pilot hole, perforator then deepening and expanding reamers used alternatively. The acetabulum was reamed in cranial direction (Fig. 16.1).


Fig. 16.1
Reaming the acetabulum in proximal direction – guideline was the patient’s opposite shoulder
The new cavity prepared matched the shape of the cup reasonably well and this allowed some degree of cement containment and pressurisation. With the cup placed more cranially, however, some limb shortening or at least inability to restore leg length, was probably inevitable, and was considered to be one factor that could contribute to post-operative dislocation. This was the technique until November 1970 when transverse reaming of the acetabulum was established. The detail of the technique was to use the same set of instruments but directing them transversely in line with anterior superior iliac spines (Fig. 16.2).
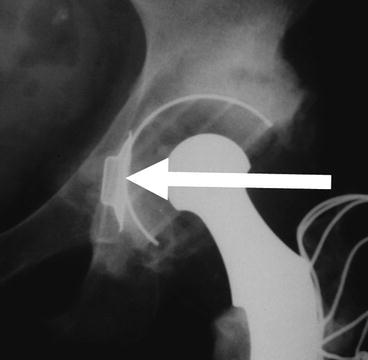
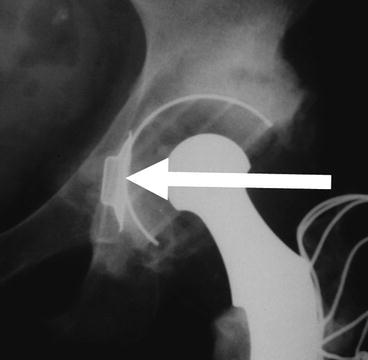
Fig. 16.2
Transverse reaming of the acetabulum – guideline was the anterior superior iliac spines
The centering ring and the reamers had their lower margin at the level of the “teardrop” the junction between the obturator foramen and the acetabulum. The centre of rotation was thus brought distally, the cup could be placed at the more anatomical level and thus contribute to leg length equalization.
Long Posterior Wall (LPW) Cup
The long posterior wall cup (LPW) (Fig. 16.3) was introduced in May 1972.
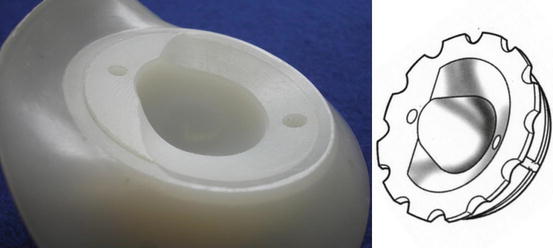
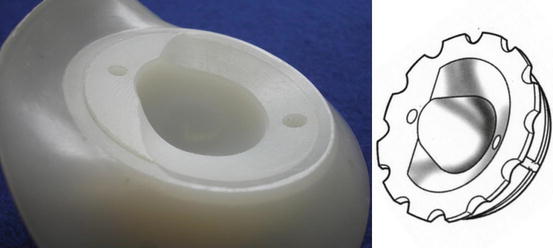
Fig. 16.3




The long posterior wall cup introduced in May 1972
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








