Discoid lateral meniscus is a common abnormal meniscal variant in children. Detailed history and physical examination combined with an MRI of the knee predictably diagnose a discoid meniscus. The clinical presentation varies from being asymptomatic to snapping, locking, and causing severe pain and swelling of the knee. Because of the pathologic anatomy and instability, discoid menisci are more prone to tearing. Treatment options for symptomatic patients vary based on the type of anomaly, the age of the patient, stability, and the presence or absence of a tear. Improvements in arthroscopic equipment and technique have resulted in good to excellent short-term outcomes for saucerization and repair.
Key points
- •
Discoid lateral meniscus is a common abnormal meniscal variant in children. A detailed history and physical examination, when combined with an MRI of the knee, can predictably diagnose a discoid meniscus. The discoid meniscus was typically classified as type I (complete), type II (incomplete), or type III (Wrisberg variant).
- •
It is now imperative to assess and determine the instability, and the newer classification based on stability of the peripheral rim is more relevant clinically and from the surgical perspective.
- •
The clinical presentation varies from being asymptomatic to snapping, locking, and causing severe pain and swelling of the knee. Because of the pathologic anatomy and instability, discoid menisci are more prone to tearing, which is often the cause of these presenting mechanical symptoms.
- •
Treatment options for symptomatic patients vary based on the type of anomaly, the age of the patient, stability, and the presence or absence of a tear. Most surgeons prefer arthroscopic partial central meniscectomy and stabilization to the capsule (if unstable) and repair of the tear if any rather than complete or subtotal meniscectomy.
- •
Improvements in arthroscopic equipment and technique have resulted in good to excellent short-term outcomes for saucerization and repair. Prospective studies with larger number of patients that assess the long-term outcome are required to define the perfect treatment strategy.
Introduction
The discoid lateral meniscus is the most common abnormal meniscal variant in children. The morphology of a discoid meniscus varies but it typically covers a greater than normal area of the tibial plateau. The incidence of discoid lateral meniscus is estimated to be 0.4% to 17% in the lateral meniscus where it is most common. Medial discoid menisci are extremely rare. A discoid lateral meniscus can be unstable causing pain and mechanical symptoms in younger children and is more likely to present as a tear in older children. Improvements in arthroscopic techniques have led to greater attempts to saucerize, repair, and stabilize the torn discoid lateral meniscus and recent literature suggests good short-term results. This article reviews the anatomy, classification, clinical presentation, imaging studies, and management including surgical options for discoid lateral meniscus in the pediatric population.
Anatomy and classification
The meniscus is completely vascular at birth with blood supply entering from the periphery of the meniscus. By the ninth month of life, the central third becomes avascular. Meniscal vascularity gradually diminishes to the peripheral 10% to 30% by age 10 years, at which time it resembles the adult meniscus. Increased blood supply and recent evidence suggesting regeneration of a discoid meniscus after saucerization suggests increased potential for repair and regeneration of the meniscal tissue especially in the pediatric population and better reparative potential than the adult meniscus.
Recent case reports discuss regeneration of discoid meniscus after partial meniscectomy in younger patients perhaps implying that a discoid meniscus arises through variant morphogenesis and also raises concerns of regrowth after partial meniscectomy.
Normal menisci are fibrocartilaginous structures in the knee joint that are C-shaped in the axial plane and wedge-shaped in the coronal plane and help increase the contact surface area between the tibia and the femur. A discoid meniscus has a completely filled-in central area or a very small void in the central area in contrast to a normal semilunar-shaped meniscus. The outer rim of a discoid meniscus is also much thicker than a normal meniscal rim. These anatomic variations alter the normal mechanical relationship and predispose the meniscus to injury and tearing. The exact cause of a discoid meniscus has not been determined, but is believed to be multifactorial. The normal meniscus is not formed from a discoid precursor. Because the menisci have a semilunar shape from the beginning of their formation, the discoid meniscus may likely represent a congenital anomaly. There is also a genetic or familial factor that is believed to play a role in the development of discoid menisci.
Watanabe classified the discoid menisci as complete, incomplete, or Wrisberg ligament type depending on the presence or absence of a normal posterior attachment and the degree of tibial plateau coverage ( Fig. 1 ). The most common type of discoid meniscus is the complete type, which is characterized by a much thickened lateral meniscus that fills the entire lateral compartment. The thickened cartilage, because of its anatomic properties, is more prone to tear with sports activities when compared with a normal meniscus ( Fig. 2 A). The second type is the incomplete type, because the meniscus is smaller than type I. Both type I and II have normal peripheral attachments and are stable to arthroscopic probing (see Fig. 2 B).
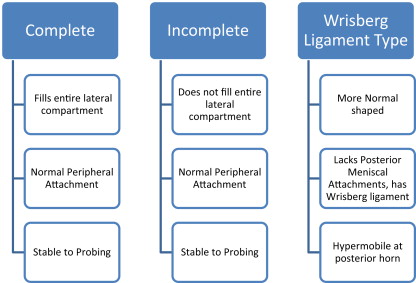
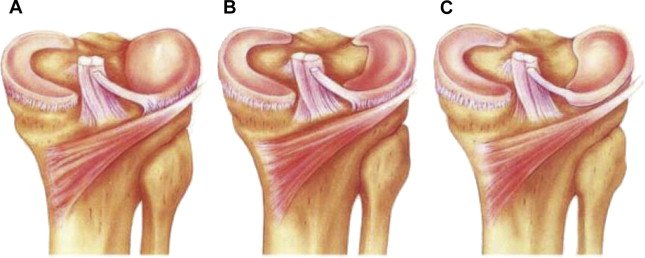
The Wrisberg type (least common, type III) is a more normally shaped meniscus that lacks usual posterior meniscal attachments, including the meniscotibial (ie, coronary) ligament. It does have a ligament of Wrisberg that connects the posterior horn of the lateral meniscus to the lateral surface of the medial femoral condyle (see Fig. 2 C). Hypermobility of the lateral meniscus at the posterior horn allows the meniscus to displace with knee extension and is postulated to cause the classic snapping knee syndrome.
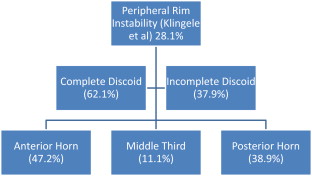
Although this is a frequently used classification, its utility for surgical decision making is questionable. Because of its variability, Klingele and colleagues described the peripheral rim instability patterns in discoid menisci. In their series of 128 discoid lateral menisci, 62.1% were complete discoid and 37.9% were incomplete. Peripheral rim instability was noted in 28.1% of cases. Instability most commonly occurred in the anterior horn of the meniscus (47.2%), followed by the posterior third (38.9%), and the middle third (11.1%). These findings suggest a newer classification system based on the size, stability, and presence or absence of a meniscal tear ( Fig. 3 ).
Clinical features
- •
Asymptomatic: Children often have no symptoms from a discoid lateral meniscus.
- •
Symptoms referable to a discoid meniscus typically stem from either a tear of the meniscus or from an unstable discoid variant.
- •
The typical presentation in a young child with a symptomatic discoid meniscus is that of a popping or snapping of the knee that is heard and felt by the child or parent. The onset of the snapping or popping is usually insidious without any specific traumatic cause, classically between the ages of 5 and 10 years.
- •
The snapping knee may have associated pain, giving way, effusion, quadriceps atrophy, limitation of motion or asymmetric extension, clicking, or locking.
- •
The older child may also present with more acute symptoms, such as significant pain, knee locking, and inability to put weight on the affected extremity. These mechanical symptoms are more likely caused by tearing of the discoid meniscus. Physical examination findings include lateral joint line tenderness and snapping as the knee is flexed or extended. Frequently, McMurray test and Apley grinding test produce pain and an audible and palpable loud click or snap. This occurs because of the translation of the femoral condyle over a thickened posterior rim of the lateral meniscus.
- •
Patients with unstable discoid meniscus may present with complaints of knee instability because of a defect in the posterior meniscofemoral ligament.
Investigations
Plain radiographs of the knee should be obtained in all children with an acute injury. These views include the anteroposterior, lateral, tunnel, and sunrise or Merchant views.
- •
Tunnel views: to rule out osteochondritis dissecans (OCD) lesions as the source of knee pain. The typical anatomic location of an OCD lesion is the lateral aspect of the medial femoral condyle. However, lateral OCD lesions should raise the concern for a discoid meniscus as the underlying cause. Patellar dislocation may result in a chondral loose body displaced from the lateral trochlea, which can result in mechanical symptoms mimicking a meniscal tear.
- •
Sunrise or Merchant radiograph: to rule out patellar subluxation, trochlear dysplasia, and osteochondral loose bodies.
- •
Radiographs are often normal in patients with a discoid meniscus, but may show subtle widening of the lateral joint space especially when compared with the contralateral knee. A squared-off appearance of the lateral femoral condyle, cupping of the lateral tibial plateau, and tibial eminence flattening can also occasionally be seen indicating severe discoid menisci.
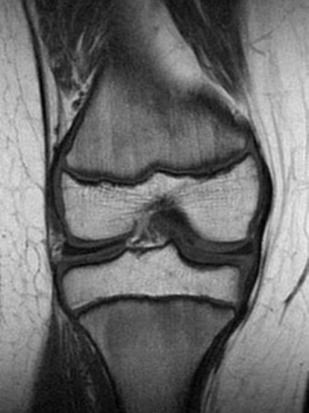
MRI is the modality of choice for confirming the diagnosis of a discoid meniscus ( Fig. 4 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




