Digestive Organs
Gastric Catarrh (Gastritis)
Functional disorders of the epigastrium like dyspepsia and stomach spasms are very common. In addition, chronic inflammatory changes in the mucous membranes of the stomach are not rare either. Gastritis refers to an inflammation of the stomach, especially of the gastric mucosa. Acute gastritis arises mostly as the result of improper diet, especially excessive alcohol consumption, or less commonly as an accompanying symptom of infectious diseases or kidney failure.
Chronic gastritis always occurs when acute gastritis has not been cured properly. It diffusely affects the entire mucosa of the stomach and can arise as an independent disease, but also as an accompanying symptom of stomach ulcers, carcinomas or diseases of the liver, bile ducts, pancreas, and intestine.
Research has confirmed worldwide by now that type B chronic gastritis (antral gastritis) is triggered by colonization with Helicobacter pylori. This bacteria is an important pathogenic factor in the formation of ventricular and duodenal ulcers. Its significance as a high risk factor in stomach carcinomas is under discussion.
Symptoms
• Pressure and feeling of fullness in the upper abdomen, mostly after meals—ulcer-type complaints.
• Nausea, food intolerance.
• Heartburn, frequent belching.
• Pressure in the area of the heart, flatulence.
• Coated tongue.
The symptoms occur in alternation and are aggravated by bad eating habits, for example, hasty eating, substance abuse, medications, but also job-related or social pressures, psychological conflict situations, stress, neuroses, and depression. Allergic factors can also play a certain aggravating role.
Suggested Therapy
With evidence of Helicobacter pylori, combined treatment with chemotherapeutic drugs eliminates these bacteria completely and permanently. In patients with functional upper abdominal complaints, the numerous “mucosal protective agents” do bring symptomatic relief, but are not sufficient as cure.
 After ruling out organic stomach disease, the treatment of under- and over-acidification of gastric juices, of stomach spasms, and dyspepsia shows a good success rate when the suction cups are placed in the appropriate segments and in the solar plexus (Figs. 10.1 and 10.2).
After ruling out organic stomach disease, the treatment of under- and over-acidification of gastric juices, of stomach spasms, and dyspepsia shows a good success rate when the suction cups are placed in the appropriate segments and in the solar plexus (Figs. 10.1 and 10.2).
The following formula has proven effective:
• Every week, carry out three cupping treatments, to a total of 15 treatments. Follow up with treatments in 2-week intervals, to a total of 12 treatments.
• After this, you can carry out further cupping treatments once a month for a certain period of time, depending on success.
 Wet cupping on the left side in segments T2–T9.
Wet cupping on the left side in segments T2–T9.

Fig. 10.1 Dry cupping on the left side of the back in segments T2–T9, especially in areas of painful points; potentially also in segment C3.

Fig. 10.2 Dry cupping in the solar plexus.
Supplemental Therapy
One of the most important therapeutic measures is to soothe the patient and explain the pathophysiological connections. Patients often experience fear of cancer.
• Homeopathy. Gastritis responds reliably to homeopathic treatment. In the treatment of acute gastritis, we primarily take the cause of the disorder into consideration, in addition to the symptoms. Options are organotropic, but also constitutional remedies.
• Phytotherapy. Tea mixtures or patent preparations, according to syndrome—carminatives, spasmolytics, antiphlogistics, sedatives, bitterns.
• Dietetics. Patients should avoid foods that they believe to trigger symptoms.
Alternating Therapy
• Neural therapy. Subcutaneous injections with a neural drug above the solar plexus and in Head’s zones on the back.
• Baunscheidt therapy. Above cutivisceral reflexes.
Acute and Chronic Pancreatitis
We distinguish between two forms of pancreatitis, namely acute-reversible and chronic-progressive. Both forms are accompanied by pain and functional disturbances of varying intensity, but their causes differ.
Acute pancreatitis arises mostly after infectious disease, after diseases of the bile ducts, stomach, or intestine, or through intoxication or medications.
The causes of chronic pancreatitis are alcoholism and chronic inflammations of the stomach, intestine, and bile ducts; psychological traumas and allergies also need to be considered.
Symptoms
• In the acute stage, temperature of 38–39°C (102–104°F).
• Violent pain with sudden onset in the upper abdomen, predominantly on the left, aggravated in the shape of a half belt by movement.
• Cold sweat, nausea, and constipation as a result of intestinal atonia.
• In severe cases, redness of the face and typical drawn-up legs.
• In chronic forms, upper abdominal symptoms generally 2–3 hours after meals, increasing in the evening; pain not always on the left side.
• Belching, diarrhea, flatulence, aversion to fat, intolerances (to raw fruit, yeasted cake, sweets, and coffee), but very variable.
• Emaciation, delayed adaptation to darkness.
Suggested Therapy
A majority of our patients complain of pancreatic symptoms. Advanced pancreatitis not only results in impaired exocrine function, but occasionally also in symptoms of limited endocrine functions.
 Acute pancreatitis is a medical emergency and must be treated in a hospital.
Acute pancreatitis is a medical emergency and must be treated in a hospital.
In chronic pancreatitis or secretory pancreatic insufficiency, cupping is recommended after completed examinations and diagnosis (Figs. 10.3 and 10.4).
• Maintain intervals of 3 days over 6 weeks.
• Afterwards, due to the chronicity and unpredictability, treat over a longer period of time once per month after symptoms have subsided.
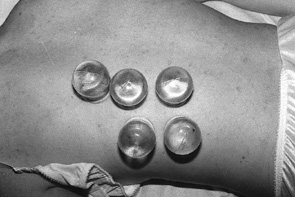
Fig. 10.3 Dry cupping on the back in segments T2–L1, especially in the areas of tender points.

Fig. 10.4 Dry cupping on the upper abdomen on the left side.
Supplemental Therapy
• Dietetics. Maintain easily digestible diet.
• Homeopathy. Diseases of the pancreas respond well to homeopathic treatment, if treatable. The number of possible remedies, however, is limited.
• Phytotherapy. Swedish bitters three times a day, one teaspoon in an herbal tea of yarrow and marigold. Harongan as patent medicine.
• In pancreatic insufficiency, enzyme substitution.
Alternating Therapy
• Neural therapy. Quaddle therapy with local anesthetics on the upper abdomen and paravertebral in segments T7–L1.
Liver Disorders (Liver Cirrhosis, Liver Congestion, Hepatitis, Fatty Liver)
The liver is an organ that switches between two organ systems—the digestive system and the circulatory system. Whenever there is a functional disturbance in one of the systems, sooner or later we are also bound to see disturbances in the liver. Conversely: if the liver is diseased,disorders of the stomach, intestine, and circulatory system result, especially heart problems.
Diseases of the liver are widespread and quite malicious. The patient initially has no complaints for a while because the liver itself does not hurt. Signs of the disease arise only in advanced stages. Because arising complaints are often atypical, it is not always easy to recognize liver disease. Nausea and a feeling of pressure in the upper abdomen first suggest stomach and/or intestinal disorders.
The most well-known symptom is jaundice, which can, however, also arise as a secondary symptom of diseases,for example, of the gallbladder, pancreas, or heart, or as a concomitant sign of infections (e.g., Weil disease).
Symptoms
Acute hepatitis. This is a viral infection, either in the framework of a generalized infection or of an infection limited to the liver. Chronic hepatitis develops from the acute form, especially when acute hepatitis is unrecognized and not treated in time. Both forms manifest with the following symptoms:
• In the acute stage, jaundice, beer-brown coloration of urine, fatigue, digestive problems.
• The liver is often enlarged.
• The chronic stage corresponds to acute hepatitis, with the difference that jaundice, liver swelling, and impaired liver functions last longer when they arise.
Liver cirrhosis can develop from an uncured case of acute or chronic hepatitis, but also as a result of chronic cholangitis, alcoholism, or persistent malnutrition. The following symptoms are indicative:
• Pressure in the upper abdomen.
• Lack of appetite.
• Nausea.
• Flatulence.
• Depressed mood.
• Fatigue.
• Intolerance to fat.
• Certain signs on the skin (spider nevi, pelmar erythema).
Liver congestion arises as a result of heart disease or disturbed blood circulation in the lung. It manifests in the following symptoms:
• Gastrointestinal complaints as a result of liver distention.
• Headache and exhaustion.
• Functional disturbances in the liver are further aggravated by certain medications. Therefore, naturopathic treatments should be given priority in the treatment of liver disorders.
Suggested Therapy
In liver disorders of all types and in every stage, treatment with cupping is recommended as basic treatment, because it increases the regenerative capacity of the liver (Figs. 10.5 and 10.6).
• Initially two to three treatments per week, to a total of 12 treatments. Afterwards, carry out 12 treatments in intervals of 14-21 days.
• Subsequently, over a long period of time, once a month.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





