Abstract
Objectives
To assess the diagnostic value of clinical tests for degenerative rotator cuff disease (DRCD) in medical practice.
Methods
Patients with DRCD were prospectively included. Eleven clinical tests of the rotator cuff have been done. One radiologist performed ultrasonography (US) of the shoulder. Results of US were expressed as normal tendon, tendinopathy or full-thickness tear (the reference). For each clinical test and each US criteria, sensitivity, specificity, negative predictive value and positive predictive value, accuracy, negative likelihood ratio (NLR) and positive likelihood ratio (PLR) were calculated. Clinical relevance was defined as PLR ≥2 and NLR ≤0.5.
Results
For 35 patients (39 shoulders), Jobe (PLR: 2.08, NLR: 0.31) and full-can (2, 0.5) test results were relevant for diagnosis of supraspinatus tears and resisted lateral rotation (2.42, 0.5) for infraspinatus tears, with weakness as response criteria. The lift-off test (8.50, 0.27) was relevant for subscapularis tears with lag sign as response criteria. Yergason’s test (3.7, 0.41) was relevant for tendinopathy of the long head of the biceps with pain as a response criterion. There was no relevant clinical test for diagnosis of tendinopathy of supraspinatus, infraspinatus or subscapularis.
Conclusions
Five of 11 clinical tests were relevant for degenerative rotator cuff disease.
Résumé
Objectif
Évaluer la valeur diagnostique des tests cliniques pour tendinopathies dégénératives de la coiffe des rotateurs (TDCR) en pratique médicale.
Méthodes
Des patients avec TDCR ont été inclus de façon prospective. Onze tests cliniques de la coiffe des rotateurs ont été pratiqués. Un échographiste réalisait les échographies d’épaule en insu. Les résultats échographiques étaient exprimés en tendon normal, tendinopathie et rupture transfixiante. Sensibilité, spécificité, valeurs prédictives positive et négative, exactitude, ratio de vraisemblance (RV) positif et négatif ont été calculés pour chaque test et chaque diagnostic échographique. La valeur diagnostique a été admise à partir d’un RV positif et négatif, ≥ 2 et ≤ 0,5.
Résultats
Trente-cinq patients et 39 épaules ont été inclus. Le test de Jobe (RV positif: 2,08, RV négatif: 0,31) et le full-can test (2, 0,5), avec pour réponse la faiblesse, atteignaient le seuil de valeur diagnostique pour la rupture du supra-épineux, la rotation latérale en position 1 (2,42, 0,5) pour celle de l’intra-épineux et le lift-off test (8,50, 0,27) pour celle du subscapulaire. Le test de Yergason (3,7, 0,41) atteignait ce seuil pour la tendinopathie du long biceps. Aucun test clinique n’atteignait ce seuil pour les tendinopathies des supra-épineux, infra-épineux et subscapulaire.
Conclusions
Ce travail montre la valeur diagnostique de 5 des 11 tests cliniques de la coiffe évalués.
1
English version
1.1
Introduction
Shoulder pain is common in adults and the frequency increases with age . In primary care, shoulder disorders are the third most common reason for consultation for musculoskeletal complaints . Degenerative rotator cuff disease is the main shoulder condition . It includes tendinopathy, partial- and full-thickness tendon tear of the supraspinatus, infraspinatus or suscapularis tendon and can be associated with tendinopathy of the long head of the biceps tendon.
Clinical history and careful physical examination are essential to ensure accurate diagnosis and choose the appropriate therapy . Many clinical tests have been used to explore the rotator cuff. A rigorous description of clinical tests is therefore crucial. Each test has its own initial description and interpretation . However, the description of several tests are close and may be confused with each other. All the tests cannot reasonably be performed at each clinical examination. Therefore, clinical tests of the rotator cuff should be selected on the basis of their diagnostic performance. However, few studies have investigated their performance with sound methodology and their results are partly controversial . Such discrepancies can be explained by differences in methods and study populations. Most patients in these studies were from surgical departments, and their characteristics should not be representative of the population seen in general or in medical practice.
Therefore, to select the most relevant tests, we evaluated 11 clinical tests with ultrasonography (US) findings as a reference in patients with degenerative rotator cuff disease from a rehabilitation unit of a rheumatology department.
1.2
Methods
This was a cross-sectional descriptive study. Response criteria for clinical tests, diagnostic references and data collection were planned before the study start. The study was carried out under conditions of usual care in our unit. Participants gave their written informed consent to be in the study.
1.3
Patients
Patients attending the unit for ambulatory physiotherapy treatment for degenerative rotator cuff disease were considered for inclusion. They were prospectively recruited from consultation in a rehabilitation unit from single rheumatology clinic in an urban university hospital in France. Inclusion criteria were age >40 years, shoulder pain duration of at least 1 month, and diagnosis of degenerative rotator cuff disease. We excluded patients with limited passive range of motion, tendon calcification on radiographs, previous surgery, shoulder instability, humeral fracture, local steroid injections in the preceding 30 days, inflammatory joint disease and neoplastic disorders. Other exclusion criteria were evidence of neurological or cervical disease on physical examination, not signing a written consent and not undergoing US examination.
1.4
Clinical examination
Clinical data collected for all patients at inclusion were gender, age, dominant side, pain duration, any trauma triggering symptoms, levels of pain and disability, and results of rotator cuff tests. Pain was assessed on a 0- to 100-point Visual Analog Scale (VAS). Disability was assessed on a 0- to 100-point VAS and the 0- to 100-point Disabilities of the Arm, Shoulder and Hand (DASH) outcome measure . A physician trained in shoulder diseases performed the physical examination for all the patients. He was blinded to US results.
1.5
Clinical tests for the supraspinatus tendon
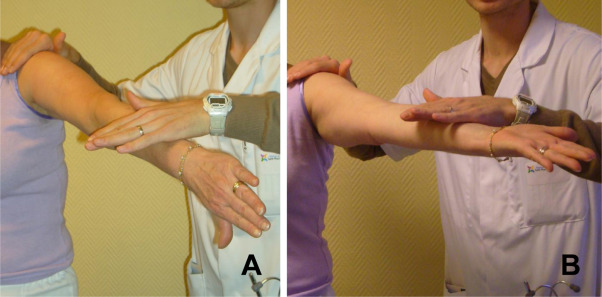
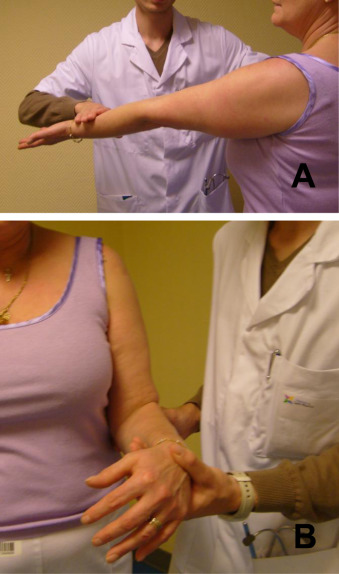
Clinical tests were the Jobe and full-can tests. The Jobe test, also known as the empty-can test, was performed with the arm at 90 degrees of abduction, 30 degrees of forward flexion and full internal rotation with the thumbs down ( Fig. 1 A) . The full-can test was performed with the same position as the Jobe test except for a 45-degree lateral rotation of the arm ( Fig. 1 B) . For these 2 tests, both pain and weakness against resistance when the physician pulled down on the arm were response criteria.
1.6
Clinical tests for the infraspinatus tendon
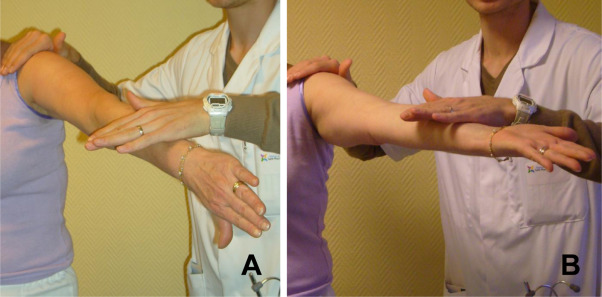
Clinical tests were the hornblower, dropping, gate and Patte tests and shoulder strength in resisted lateral rotation at 0 degrees of abduction. For the hornblower test, the patient raised the hand to the mouth. The result was positive if the patient had to raise the elbow above the hand to reach the mouth ( Fig. 2 A) . For the dropping test, the elbow was flexed at 90 degrees with the arm by the side while the shoulder was laterally rotated at 45 degrees by the physician ( Fig. 2 B). The patient was asked to maintain this position. The result was positive if the patient was unable to maintain this position and the arm returned to the neutral position after the examiner released it . For the gate test, the elbow was flexed at 90 degrees with the arm by the side and in neutral rotation. The patient was then asked to medially rotate the arm against the resistance of the examiner ( Fig. 2 C). The result was positive if the patient could not maintain this position and the forearm hit the belly after the physician released it . Patte test was performed with the arm at 90 degrees of elevation in the plane of the scapular wing, with 90 degrees of lateral rotation, and the elbow flexed at 90 degrees ( Fig. 2 D). The patient was then asked to laterally rotate the arm while the examiner, holding the elbow, applied a medial rotation force . Both pain and weakness were registered. Weakness corresponded to the inability to laterally rotate the arm against the resistance applied by the physician. Shoulder strength in resisted lateral rotation at 0 degrees of abduction was assessed with the elbow flexed at 90 degrees with the arm by the side and in neutral rotation ( Fig. 2 E). The patient was asked to laterally rotate the arm against the resistance of the physician. Both pain and weakness were registered.
1.7
Clinical tests for the subscapularis tendon
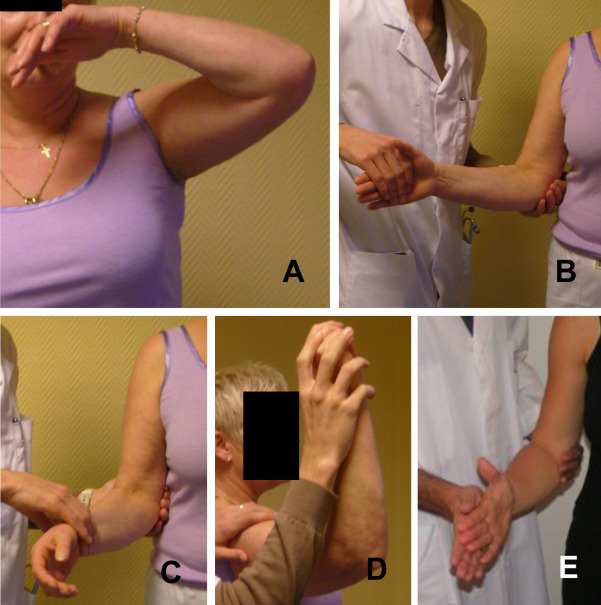
Clinical tests were the lift-off and belly-press tests. For the lift-off test, the arm was medially rotated, with the dorsum of the hand placed in the midlumbar region ( Fig. 3 A) . The patient was then asked to lift the hand off the back. The result was positive if the patient was unable to lift the hand in this position. A variant of the lift-off test was bringing the patient’s arm passively behind the body in maximal medial rotation . A “lag sign” was present and the result was positive if the patient was unable to actively maintain this position once the examiner released the patient’s hand. In such cases, the hand drops to the back and the patient is unable to lift it off actively without extending the elbow. For the belly-press test, the patient pressed the abdomen with the hand flat while maintaining the arm in maximum medial rotation ( Fig. 3 B). The result was positive if the elbow dropped toward the side. The medial rotation cannot be achieved and pressure is exerted by extension of the shoulder and flexion of the wrist.
1.8
Clinical tests for the long head of the biceps tendon
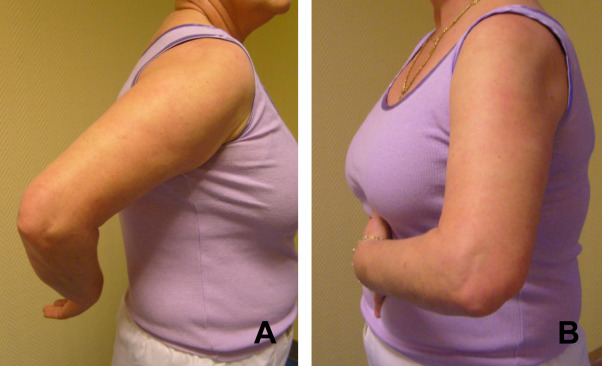
Clinical tests were the palm-up and Yergason’s tests. The palm-up test, also known as Speed’s test, was performed with the arm elevated anteriorly against resistance while the elbow was in extension and the forearm supinated ( Fig. 4 A) . Yergason’s test is a forearm supination test against resistance . The elbow was flexed at 90 degrees with the arm by the side and the forearm in pronation ( Fig. 4 B). The patient was then asked to perform an active supination against the resistance of the physician’s hand placed on the wrist. Results of these 2 tests were positive when they triggered pain localized to the bicipital groove.
1.9
Ultrasonography
US was the reference method for diagnosis and classification of rotator cuff tendon abnormalities. It is a valid non-invasive imaging method suitable for a non-surgical study population . US involved use of a dedicated 7- to 15-MHz probe. A radiologist trained in musculoskeletal diseases and US and blinded to results of the physical examination performed US for all patients. For the supraspinatus, infraspinatus and subscapularis tendons and the long head of the biceps tendon, US classification was as follows: normal tendon, tendinopathy including partial-thickness tear, and full-thickness tear. Effusion in sub-acromial bursa or in the long head of the biceps sheath was also recorded. A normal tendon corresponded to a normal-shaped homogenous hyperechogenic tendon . Tendinopathy was considered in cases of thickened or heterogenous tendon with or without partial tear. Full-thickness tear corresponded to discontinuation of the tendon or to its flatness with loss of the normal convexity of its superior aspect.
1.10
Statistical analysis
Indeterminate results were not allowed for US or clinical tests. With missing data, the shoulder data were excluded from analysis, completely excluded with missing US data and only partially – available data were analysed – with missing clinical testing data. A preliminary study for 1-week interval reproducibility of clinical tests indicated 74 to 100% concordance in 27 of our patients: Jobe 85% (pain) and 89% (weakness), full-can test 88 and 74%, resisted lateral rotation 93 and 81%, Patte 85 and 74%, hornblower 96%, dropping 100%, gate 96%, belly-press test 100%, lift-off test 100% (lag sign) and 93% (weakness), palm-up test 70%, and Yergason’s test 74%. Sensitivity, specificity, positive predictive value and negative predictive value, positive likelihood ratio (PLR) and negative likelihood ratio (NLR), and accuracy were calculated for each response criteria of clinical tests and for each US diagnosis of tendinopathy or full-thickness tear as a reference. Results were presented with 95% confidence intervals (95% CI). The accuracy was the agreement between clinical examination and US. The LRs indicated by how much a test result would increase or reduce the pretest probability of the disease. Thus, minimal clinical relevance was considered a positive test result observed twice more often in patients with the disease (PLR ≥2) and a negative test result twice less often (NLR ≤0.5) .
1.11
Results
1.11.1
Characteristics of patients
We considered 44 patients (48 shoulders) for inclusion. Six patients (6 shoulders) refused to participate. Three additional patients were excluded: 1 had previous surgery, 1 had adhesive capsulitis, and 1 did not undergo US. We finally included 35 patients (39 shoulders; 8 men). The mean age was 59 (S.D.: 11) years and mean duration of shoulder symptoms 31 (62) months, with 29 cases involving the dominant side. A triggering trauma was found for 9 shoulders. Scores on the VAS for pain and disability were 53 (22) and 54 (24), respectively. Mean DASH score was 48 (18).
1.11.2
Ultrasonography findings
Accordingly to the non-invasive nature of US, no adverse events occurred during the examination. The number of cases with normal tendons, tendinopathy and full-thickness tear are shown in Table 1 . Overall, 3 shoulders (8%) had a full-thickness tear of the 3 tendons; 5 (13%) had a full-thickness tear of both supraspinatus and infraspinatus tendons, and 1 shoulder had a full-thickness tear of both supraspinatus and subscapularis tendons. Overall, 15 shoulders (38%) showed effusion in the sub-acromial bursa, which was the only lesion in 1 shoulder. The long head of the biceps tendon was normal in 32 shoulders (82%); 6 shoulders (15%) showed tendinopathy and 1 shoulder had a full-thickness tear. Effusion in the long head of the biceps sheath was detected in 3 shoulders (8%).
| Tendons and clinical tests | Clinical responses | Ultrasonography findings | |||
|---|---|---|---|---|---|
| Normal, n (%) | Tendinopathy, n (%) | Tear, n (%) | Total, n | ||
| Supraspinatus | 12 (31) | 6 (15) | 21 (53) | 39 | |
| Jobe test | Pain | 10 (29) | 6 (17) | 19 (54) | 35 |
| Weakness | 5 (21) | 2 (8) | 17 (71) | 24 | |
| Full-can test | Pain | 6 (22) | 3 (11) | 18 (67) | 27 |
| Weakness | 4 (20) | 2 (10) | 14 (70) | 20 | |
| Infraspinatus | 26 (67) | 5 (13) | 8 (21) | 39 | |
| Hornblower test | Weakness | 1 (50) | 0 | 1 (50) | 2 |
| Dropping test | Weakness | 0 | 0 | 0 | 0 |
| Gate test | Weakness | 1 (33) | 0 | 2 (67) | 3 |
| Resisted lateral test | Pain | 16 (66) | 4 (17) | 4 (17) | 24 |
| Weakness | 8 (62) | 0 | 5 (38) | 13 | |
| Patte test | Pain | 20 (65) | 5 (16) | 6 (19) | 31 |
| Weakness | 7 (54) | 2 (15) | 4 (31) | 13 | |
| Subscapularis | 30 (77) | 4 (10) | 5 (13) | 39 | |
| Belly-press test | Pain | 7 (64) | 2 (18) | 2 (18) | 11 |
| Weakness | 0 | 0 | 3 (100) | 3 | |
| Lift-off test | Weakness | 0 | 0 | 2 (100) | 2 |
| Lag sign | 3 (50) | 0 | 3 (50) | 6 | |
| Long head of biceps | 32 (82) | 6 (15) | 1 (3) | 39 | |
| Palm-up test | Pain | 21 (81) | 5 (19) | 0 | 26 |
| Yergason’s test | Pain | 6 (60) | 4 (40) | 0 | 10 |
1.11.3
Results of clinical tests
The lift-off test could not be performed in one shoulder because of pain. Clinical testing was well tolerated in all other patients. The distribution of clinical test results by US findings is in Table 1 . Clinical test results did not reach clinical diagnostic relevance when tendinopathy and full-thickness tear data were pooled as a single reference. Therefore, we display the diagnostic performance of clinical tests separately with tendinopathy ( Table 2 ) and full-thickness tear ( Table 3 ) as references.
| Clinical tests | Response criteria | Se (%) | Sp (%) | PPV (%) | NPV (%) | PLR | NLR | Ac (%) |
|---|---|---|---|---|---|---|---|---|
| Supraspinatus | ||||||||
| Jobe | Pain | 100 [54.1; 100] | 12.1 [3.4; 28.2] | 17.1 [6.6; 33.6] | 100 [39.8; 100] | 1.14 [0.61; 1.3] | 0 [0; 3.95] | 25.6 [13; 42.1] |
| Weakness | 33.3 [4.3; 77.7] | 33.3 [17; 51.8] | 8.3 [1; 27] | 73.3 [44.9; 92.2] | 0.5 [0.14; 1.13] | 2 [0.81; 3.86] | 33.3 [19.1; 50.2] | |
| Full-can | Pain | 50 [11.8; 88.2] | 27.3 [13.3; 45.5] | 11.1 [2.3; 29.2] | 75 [42.8; 94.5] | 0.69 [0.25; 1.22] | 1.83 [0.61; 4.21] | 30.8 [17; 47.6] |
| Weakness | 33.3 [4.3; 77.7] | 45.4 [28.1; 63.6] | 10 [1.2; 31.7] | 78.9 [54.4; 93.9] | 0.61 [0.17; 1.44] | 1.47 [0.62; 2.58] | 43.6 [27.8; 60.4] | |
| Infraspinatus | ||||||||
| Hornblower | Weakness | 0 [0; 52.2] | 94.1 [80.3; 99.3] | 0 [0; 84.2] | 86.5 [71.2; 95.5] | 0 [0; 10.31] | 1.06 [0.52; 1.16] | 82 [66.5; 92.5] |
| Dropping | Weakness | 0 [0; 52.2] | 100 [89.7; 100] | [0; 100] a | 87.2 [72.6; 95.7] | [0; infinity] a | 1 [0; infinity] | 87.2 [72.6; 95.7] |
| Gate | Weakness | 0 [0; 52.2] | 91.2 [76.3; 98.1] | 0 [0; 70.8] | 86.1 [70.5; 95.3] | 0 [0; 6.48] | 1.1 [0.54; 1.22] | 79.5 [63.5; 90.7] |
| Resisted lateral rotation | Pain | 80 [28.4; 99.49] | 41.2 [24.6; 59.3] | 16.7 [4.7; 37.4] | 93.3 [68; 99.8] | 1.36 [0.61; 2.06] | 0.49 [0.08; 1.73] | 46.1 [30.1; 62.8] |
| Weakness | 0 [0; 52.2] | 61.8 [43.6; 77.8] | 0 [0; 24.7] | 80.7 [60.6; 93.4] | 0 [0; 1.23] | 1.62 [0.77; 2.09] | 53.8 [37.2; 69.9] | |
| Patte | Pain | 100 [47.8; 100] | 21.2 [9; 38.9] | 16.1 [5.4; 33.7] | 100 [59; 100] | 1.27 [0.61; 1.51] | 0 [0; 2.38] | 31.6 [17.5; 48.6] |
| Weakness | 40 [5.3; 85.3] | 66.7 [48.2; 82] | 15.4 [1.9; 45.4] | 88 [68.8; 97.4] | 1.2 [0.33; 2.97] | 0.9 [0.34; 1.51] | 63.2 [46; 78.2] | |
| Subscapularis | ||||||||
| Belly-press | Pain | 50 [6.8; 93.2] | 74.3 [56.7; 87.5] | 18.2 [2.2; 51.8] | 92.9 [76.5; 99.1] | 1.94 [0.53; 4.71] | 0.67 [0.2; 1.23] | 71.8 [55.1; 85] |
| Weakness | 0 [0; 60.2] | 91.4 [76.9; 98.2] | 0 [0; 70.8] | 88.9 [73.9; 96.9] | 0 [0; 7.83] | 1.09 [0.47; 1.19] | 82 [66.5; 92.5] | |
| Lift-off | Weakness | 0 [0; 60.2] | 94.1 [80.3; 99.3] | 0 [0; 84.2] | 88.9 [73.9; 96.9] | 0 [0; 12.24] | 1.06 [0.46; 1.14] | 84.2 [68.7; 94] |
| Lag sign | 0 [0; 60.2] | 82.3 [65.5; 93.2] | 0 [0; 45.9] | 87.5 [71; 96.5] | 0 [0; 3.37] | 1.21 [0.52; 1.4] | 73.7 [56.9; 86.6] | |
| Biceps | ||||||||
| Palm-up | Pain | 83.3 [35.9; 99.6] | 36.4 [20.4; 54.9] | 19.2 [6.5; 39.3] | 92.3 [64; 99.8] | 1.3 [0.7; 1.9] | 0.46 [0.08; 1.79] | 43.6 [27.8; 60.4] |
| Yergason a | Pain a | 66.7 [22.3; 95.7] | 81.8 [64.5; 93] | 40 [12.2; 73.8] | 93.1 [77.2; 99.1] | 3.7 [1.3; 8.7] | 0.41 [0.12; 0.89] | 79.5 [63.5; 90.7] |
a Relevant clinical test and response criteria on the basis of PLR and NLR.
| Clinical tests | Response criteria | Se (%) | Sp (%) | PPV (%) | NPV (%) | LR+ | LR− | Ac (%) |
|---|---|---|---|---|---|---|---|---|
| Supraspinatus | ||||||||
| Jobe a | Pain | 90.5 [69.6; 98.8] | 11.1 [1.4; 34.7] | 54.3 [36.6; 71.2] | 50 [6.7; 93.2] | 1.02 [0.78; 1.37] | 0.86 [0.16; 4.54] | 53.8 [37.2; 69.9] |
| Weakness a | 80.9 [58.1; 94.5] | 61.1 [35.7; 82.7] | 70.8 [48.9; 87.4] | 73.3 [44.9; 92.2] | 2.08 [1.21; 4.08] | 0.31 [0.12; 0.75] | 71.8 [55.1; 85] | |
| Full-can a | Pain | 85.7 [63.7; 96.9] | 50 [26; 74] | 66.7 [46; 83.5] | 75 [42.81; 94.5] | 1.71 [1.11; 3.01] | 0.29 [0.09; 0.81] | 69.2 [52.4; 83] |
| Weakness a | 66.7 [43; 85.4] | 66.7 [41; 86.7] | 70 [45.7; 88.1] | 63.2 [38.4; 83.7] | 2 [1.04; 4.29] | 0.5 [0.24; 0.96] | 66.7 [49.8; 80.9] | |
| Infraspinatus | ||||||||
| Hornblower | Weakness | 12.5 [0.3; 52.6] | 96.8 [83.3; 99.9] | 50 [1.3; 98.7] | 81.1 [64.8; 92] | 3.87 [0.42; 33.92] | 0.9 [0.54; 1.08] | 79.5 [63.5; 90.7] |
| Dropping | Weakness | 0 [0; 36.9] | 100 [88.8; 100] | [0; 100] a | 79.5 [63.5; 90.7] | [0 – infinity] a | 1 [0; infinity] | 79.5 [63.5; 90.7] |
| Gate | Weakness | 25 [3.2; 65.1] | 96.8 [83.3; 99.9] | 66.7 [9.4; 99.2] | 83.3 [67.2; 93.6] | 7.75 [1.08; 54.11] | 0.77 [0.42; 0.99] | 82 [66.5; 92.5] |
| Resisted lateral rotation a | Pain | 50 [15.7; 84.3] | 35.5 [19.2; 54.6] | 16.7 [4.7; 37.4] | 73.3 [44.9; 92.2] | 0.77 [0.32; 1.38] | 1.41 [0.55; 2.94] | 38.5 [23.4; 55.4] |
| Weakness a | 62.5 [24.5; 91.5] | 74.2 [55.4; 88.1] | 38.5 [13.9; 68.4] | 88.5 [69.8; 97.5] | 2.42 [1; 5.16] | 0.5 [0.18; 1] | 71.8 [55.1; 85] | |
| Patte | Pain | 85.7 [42.1; 99.6] | 19.3 [7.4; 37.5] | 19.3 [7.4; 37.5] | 85.7 [42.1; 99.6] | 1.06 [0.59; 1.42] | 0.74 [0.12; 3.47] | 31.6 [17.5; 48.6] |
| Weakness | 57.1 [18.4; 90.1] | 71 [52; 85.8] | 30.8 [9.1; 61.4] | 88 [68.8; 97.4] | 1.97 [0.76; 4.21] | 0.6 [0.22; 1.15] | 68.4 [51.3; 82.5] | |
| Subscapularis | ||||||||
| Belly-press | Pain | 40 [5.3; 85.3] | 73.5 [55.6; 87.1] | 18.2 [2.3; 51.8] | 89.3 [71.8; 97.7] | 1.51 [0.41; 3.95] | 0.82 [0.31; 1.33] | 69.2 [52.4; 83] |
| Weakness | 60 [14.7; 94.7] | 100 [89.7; 100] | 100 [29.2; 100] | 94.4 [81.3; 99.3] | [5.63; infinity] a | 0.4 [0.12; 0.78] | 94.9 [82.7; 99.4] | |
| Lift-off a | Weakness | 50 [6.7; 93.2] | 100 [89.7; 100] | 100 [15.8; 100] | 94.4 [81.3; 99.3] | [4.62; infinity] a | 0.5 [0.15; 0.87] | 94.7 [82.2; 99.4] |
| Lag sign a | 75 [19.4; 99.4] | 91.2 [76.3; 98.1] | 50 [11.8; 88.2] | 96.9 [83.8; 99.9] | 8.5 [2.33; 26.65] | 0.27 [0.05; 0.78] | 89.5 [75.2; 97.1] | |
| Biceps | ||||||||
| Palm-up | Pain | 0 [0; 97.5] | 31.6 [17.5; 48.6] | 0 [0; 13.2] | 92.3 [64; 99.8] | 0 [0; 1.21] | 3.17 [0.39; 4.35] | 30.8 [17; 47.6] |
| Yergason | Pain | 0 [0; 97.5] | 73.7 [56.9; 86.6] | 0 [0; 30.8] | 96.5 [82.2; 99.9]) | 0 [0; 3.7] | 1.36 [0.17; 1.45] | 71.8 [55.1; 85] |
a Relevant clinical test and response criteria on the basis of PLR and NLR.
1.11.3.1
Tendinopathy as reference
No clinical test showed clinical diagnostic relevance for tendinopathy of the 3 cuff tendons ( Table 2 ). Contrary to the palm-up test, Yergason’s test with pain as a clinical response criterion gave relevant LR values for tendinopathy of the long head of the biceps.
1.11.3.2
Full-thickness as reference
For diagnosis of a supraspinatus full-thickness tear, the Jobe and full-can test results showed clinical relevance with weakness as the response criterion ( Table 3 ). For an infraspinatus full-thickness tear, the resisted lateral rotation test had the best performance with weakness as the clinical response. For subscapularis full-thickness tears, the belly-press test with weakness as the clinical response and the lift-off test with weakness or lag sign as a clinical response gave relevant negative LRs. However, the lift-off test with the lag sign as a clinical response was the only test demonstrating a relevant PLR for subscapularis full-thickness tears. A 100% specificity prevented estimation of PLR for the lift-off and belly-press tests with weakness as a clinical response.
We further investigated the value of the association of the 5 relevant clinical tests, providing the number of negative patients with US diagnosing a rotator cuff lesion and the number of positive patients with normal US. Nine patients had a negative clinical testing. In three of them US found a rotator cuff lesion which was a tear of the supraspinatus tendon. True negative clinical testing was therefore 67% of cases. Fourteen patients had normal US. Half of them had however a positive clinical testing.
1.12
Discussion
Our results indicate suitable clinical relevance for 5 of the 11 clinical tests for diagnosis of degenerative changes of the rotator cuff tendons. The robustness and usefulness of our results are supported by agreement with the guidelines the STARD statement for reporting studies of diagnostic accuracy .
Some findings are in accordance with previous reports. The Jobe test with weakness as a clinical response and supraspinatus full-thickness tear as a reference was assessed in one study . Results indicated LRs close to ours. Other studies provided conflicting results, but the diagnostic references differed. Partial- and full-thickness tear data were pooled, or tendons were not individually distinguished . Comparison with our results is therefore limited. With weakness as clinical response, one study found the full-can test with suitable diagnostic relevance for a supraspinatus full-thickness tear, which agrees with our results . In another study, the results were similar with rotator cuff tear as a reference . However, the full-can test results did not reach clinical relevance with pooled partial- and full-thickness tear data as a reference . In our experience, the Jobe test results with weakness as a clinical response showed slightly better performance than the full-can test for diagnosis of a supraspinatus full-thickness tear. However, the significance of the difference remains unknown.
Several clinical tests have been investigated for the infraspinatus tendon . Weakness was the criterion for the diagnosis of an infraspinatus full-thickness tear in one study assessing the Patte test . For resisted lateral rotation, the diagnostic reference was non-specific because data were pooled partial- or full-thickness infraspinatus tear in one study and partial- or full-thickness tear of the rotator cuff in others . Furthermore, the criteria for clinical response were pooled weakness and pain data in one of these studies . The reference was fatty degenerescence by tomodensitometry in another study assessing the hornblower and dropping tests . The hornblower, dropping and Patte tests were reported to be relevant in these conditions. In previous studies, the value of the resisted lateral rotation arm by the side for full-thickness infraspinatus tear appeared limited by low specificity with weakness as a clinical response and by low sensitivity with pain or weakness as a response . In our experience, resisted lateral rotation with weakness as a clinical response was specific and was the only test with results reaching thresholds of clinical relevance for full-thickness infraspinatus tendon tear. These contradictory results may be explained by differences in reference criteria: full-thickness infraspinatus tear, pooled partial- and full-thickness infraspinatus tear and full-thickness tear of the rotator cuff tendon. Furthermore, the profile of patients and therefore the anatomical characteristics of the infraspinatus tears may vary widely among studies because patients were candidates for surgery in previous studies but not ours.
Comparisons of our results with previous reports for clinical tests of the subscapularis tendon and long head of the biceps tendon appear limited for the same reasons. Tendinopathy and full-thickness tear of the subscapularis were studied separately, with partial tear included in tendinopathy in our study. The lift-off test with weakness as a clinical response was previously found to have diagnostic relevance for subscapularis tendinopathy with or without tear but not pooled partial- and full-thickness subscapularis tear as a reference . The belly-press test has been assessed with pooled partial- and full-thickness tears of the subscapularis as a reference without reaching clinical relevance ; the test showed high specificity but low sensitivity. In our experience, the lift-off and belly-press tests both seemed suitable for diagnosis of full-thickness subscapularis tear but not tendinopathy. The relevance was fully validated for the lift-off test with lag sign as a clinical response. The low diagnostic relevance of the palm-up test for tendinopathy of the long head of the biceps was confirmed by our results. The Yergason’s test with biceps tendinopathy as a reference has not been previously investigated. We found that this test was the only one to have diagnostic value for long head biceps tendinopathy.
Our results do not support the diagnostic value of clinical tests with pain as a clinical response, which has previously been advocated for supraspinatus, infraspinatus and subscapularis tendinopathy . Reference method was surgical findings and not US as we used. Finally, our results agree with conclusions of a systematic review and guidelines that recommend the Jobe test, resisted lateral rotation and belly-press test with weakness as a clinical response for diagnosis of full-thickness tears of supraspinatus, infraspinatus and subscapularis tendons, respectively . Our results indicate that 3 additional tests could also be used. We also underline that clinical tests should be assessed and used considering specific response criteria, and specific reference diagnoses, involving the type of the lesion and also the precise tendon in which it is found. Unfortunately the confusion between response criteria of the tests and between reference diagnoses remains observed in publications , some of them considered as high-level studies and selected for meta-analysis .
Our study has several limitations. Our reference method for tendon abnormalities was not surgery but, rather, US. The diagnostic value of US compared with surgery for full-thickness tears is sensitivity 58 to 100% and specificity 78 to 100% . It greatly varies according to the frequency of the US transducer and operator. We used US at 7 to 15 MHz performed by a trained musculoskeletal radiologist. US analysis was standardized according to well-established criteria . Suitable interobserver reliability, namely 79 to 100%, has previously been reported using US in patients with tendon lesions of the shoulder . Because the diagnosis of partial tear by US is challenging, we did not consider partial tears separately as a diagnostic reference and instead considered them together with tendinopathy, which may have contributed to the low diagnostic value that we found for clinical tests of rotator cuff with tendinopathy as a reference. In addition, our patients were candidates not for surgery but, rather, for conservative treatment. Therefore, they may be not representative of all patients with shoulder pain. However, our population could be considered representative of patients examined in the clinic, namely rehabilitation rheumatology. Finally, our sample size prevented any robust subgroup analysis. We did not assess reproducibility of US results, and assessors were senior physicians experienced in rotator cuff disorders. Because of the well-known long learning curve needed for clinical and US evaluation of rotator cuff disorders, we underline the need for courses and practice for clinical and US examinations of such conditions.
In conclusion, our study revealed that 5 clinical tests satisfied clinical relevance in diagnosing full-thickness tear of supraspinatus, infraspinatus or subscapularis tendons or tendinopathy of the long head of the biceps. According to their profile, clinical tests should be investigated only with appropriate reference criteria. Some previous studies were conducted with pooled disorders, unrelated to the aim of each clinical test and each response criteria. Further studies are needed with caution on the methodology and, namely, diagnostic reference and clinical response criteria.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgements
Laura Smales was a medical editor of the final version of the manuscript.
2
Version française
2.1
Introduction
La douleur d’épaule chez l’adulte est un motif fréquent de consultation notamment en médecine générale où elle représente la troisième plainte ostéo-articulaire . Les tendinopathies dégénératives de la coiffe des rotateurs (TDCR) sont l’étiologie la plus commune et leur fréquence augmente avec l’âge . Elles incluent les tendinopathies et les ruptures partielles ou totales des tendons du supra-épineux, de l’infra-épineux ou du subscapulaire. Elles peuvent être associées à une tendinopathie de la longue portion du biceps.
Le recueil de l’histoire clinique et l’examen physique doivent être minutieux pour établir le diagnostic et instaurer le traitement approprié . De nombreux tests, dont la description et l’interprétation initiales sont précises, ont été proposés pour explorer la coiffe des rotateurs . Néanmoins, certains tests ont une description proche et peuvent être confondus entre eux. D’autre part, il paraît impossible de réaliser l’ensemble des tests lors d’une consultation. De ce fait, les tests à effectuer doivent être sélectionnés selon leur performance diagnostique. Peu d’études ont évalué cette performance en corrélation avec l’échographie et les résultats obtenus sont controversés . Ces variations peuvent être expliquées par la méthodologie utilisée et les populations étudiées. En effet, la plupart des patients inclus dans ces études sont issus du milieu chirurgical et peuvent être différents de la population émanant du milieu médical.
Afin de déterminer les tests les plus performants, nous avons évalué 11 tests cliniques et nous les avons corrélés avec les résultats de l’échographie chez des patients souffrant de TDCR consultant dans une unité de rhumatologie.
2.2
Méthodes
L’étude a été menée de manière prospective. Les tests cliniques ont été réalisés conformément à la description princeps et les critères de réponse aux tests ont été établis avant le début de l’étude. Les participants ont donné leur consentement éclairé.
2.3
Patients
Des patients, consultant dans un service de rhumatologie d’un centre hospitalier universitaire parisien pour une rééducation ambulatoire d’une TDCR, ont été inclus de façon prospective. Un âge supérieur à 40 ans, une douleur d’épaule évoluant depuis au moins 1 mois et un diagnostic de TDCR étaient nécessaires à l’inclusion. Les patients avec une limitation passive ou une instabilité de l’épaule, une calcification tendineuse sur l’imagerie, un antécédent de chirurgie, de fracture humérale ou une infiltration de l’épaule dans le mois précédent étaient exclus de l’étude de même que ceux ayant une pathologie ostéo-articulaire inflammatoire, une néoplasie, une atteinte neurologique ou cervicale. L’absence de consentement éclairé ou d’échographie ne permettait pas l’inclusion.
2.4
Examen clinique
Les données cliniques des patients recueillies à l’inclusion comportaient le sexe, l’âge, le côté dominant, la durée de la douleur, la recherche d’un traumatisme déclenchant et le niveau de douleur mesuré par une échelle visuelle analogique (EVA) échelonnée de 0 à 100. Le degré d’invalidité a été mesuré par EVA et par la réalisation du questionnaire DASH (Disabilities of Arm, Shoulder and Hand) échelonnés de 0 à 100 . Un rhumatologue expérimenté a réalisé, à l’inclusion, l’examen physique et recueilli les résultats des tests cliniques de coiffe chez tous les patients sans connaître les résultats de l’échographie de la coiffe des rotateurs.
2.5
Tests cliniques pour le tendon du supra-épineux
Pour l’évaluation du tendon du supra-épineux, la manœuvre de Jobe et le full-can test ont été utilisés. La manœuvre de Jobe ou empty-can test a été réalisée sur le membre supérieur en extension, à 90° d’abduction, 30° d’antépulsion et en rotation médiale amenant le pouce vers le bas ( Fig. 1A ) . Le full-can test a été réalisé dans la même position que le test de Jobe mais le membre supérieur en rotation latérale de 45° ( Fig. 1B ) . La positivité de ces tests a été cherchée contre-résistance de l’examinateur qui abaisse le membre supérieur du patient, la main sur son avant-bras, pour 2 critères différents : douleur et faiblesse.